Lassa fever, also known as Lassa hemorrhagic fever, is a type of viral hemorrhagic fever caused by the Lassa virus. Many of those infected by the virus do not develop symptoms. When symptoms occur they typically include fever, weakness, headaches, vomiting, and muscle pains. Less commonly there may be bleeding from the mouth or gastrointestinal tract. The risk of death once infected is about one percent and frequently occurs within two weeks of the onset of symptoms. Of those who survive, about a quarter have hearing loss, which improves within three months in about half of these cases.

Hand, foot, and mouth disease (HFMD) is a common infection caused by a group of enteroviruses. It typically begins with a fever and feeling generally unwell. This is followed a day or two later by flat discolored spots or bumps that may blister, on the hands, feet and mouth and occasionally buttocks and groin. Signs and symptoms normally appear 3–6 days after exposure to the virus. The rash generally resolves on its own in about a week. Fingernail and toenail loss may occur a few weeks later, but they will regrow with time.
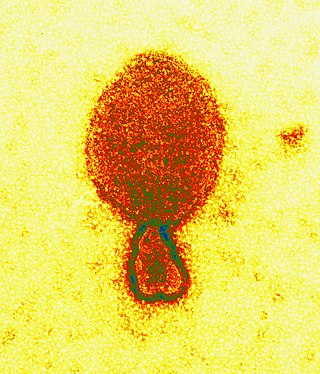
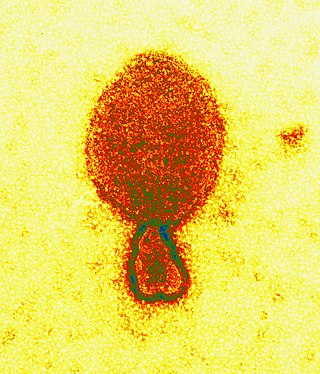
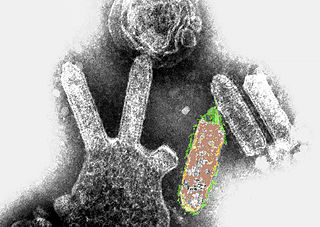
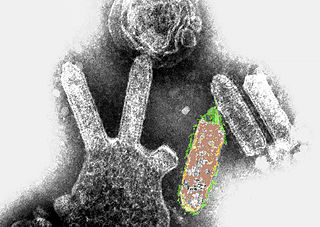
Henipavirus is a genus of negative-strand RNA viruses in the family Paramyxoviridae, order Mononegavirales containing six established species, and numerous others still under study. Henipaviruses are naturally harboured by several species of small mammals, notably pteropid fruit bats, microbats of several species, and shrews. Henipaviruses are characterised by long genomes and a wide host range. Their recent emergence as zoonotic pathogens capable of causing illness and death in domestic animals and humans is a cause of concern.

Japanese encephalitis (JE) is an infection of the brain caused by the Japanese encephalitis virus (JEV). While most infections result in little or no symptoms, occasional inflammation of the brain occurs. In these cases, symptoms may include headache, vomiting, fever, confusion and seizures. This occurs about 5 to 15 days after infection.
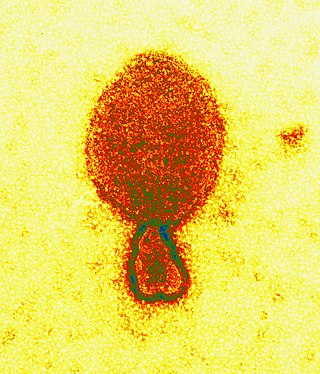
Hendra virus is a zoonotic virus found solely in Australia. First isolated in 1994, the virus has since been connected to numerous outbreaks of disease in domestic horses and seven human cases. Hendra virus belongs to the genus Henipavirus, which also contains the zoonotic Nipah virus. The reservoir species of Hendra virus are four species of bat within the genus Pteropus native to Australia.

Nipah virus is a bat-borne, zoonotic virus that causes Nipah virus infection in humans and other animals, a disease with a very high mortality rate (40-75%). Numerous disease outbreaks caused by Nipah virus have occurred in South East Africa and Southeast Asia. Nipah virus belongs to the genus Henipavirus along with the Hendra virus, which has also caused disease outbreaks.

Viral hemorrhagic fevers (VHFs) are a diverse group of animal and human illnesses. VHFs may be caused by five distinct families of RNA viruses: the families Filoviridae, Flaviviridae, Rhabdoviridae, and several member families of the Bunyavirales order such as Arenaviridae, and Hantaviridae. All types of VHF are characterized by fever and bleeding disorders and all can progress to high fever, shock and death in many cases. Some of the VHF agents cause relatively mild illnesses, such as the Scandinavian nephropathia epidemica, while others, such as Ebola virus, can cause severe, life-threatening disease.

Kyasanur forest disease (KFD) is a tick-borne viral haemorrhagic fever endemic to South-western part of India. The disease is caused by a virus belonging to the family Flaviviridae. KFDV is transmitted to humans through the bite of infected hard ticks which act as a reservoir of KFDV.
Australian bat lyssavirus (ABLV), originally named Pteropid lyssavirus (PLV), is a enzootic virus closely related to the rabies virus. It was first identified in a 5-month-old juvenile black flying fox collected near Ballina in northern New South Wales, Australia, in January 1995 during a national surveillance program for the recently identified Hendra virus. ABLV is the seventh member of the genus Lyssavirus and the only Lyssavirus member present in Australia. ABLV has been categorized to the Phylogroup I of the Lyssaviruses.

Crimean–Congo hemorrhagic fever (CCHF) is a viral disease. Symptoms of CCHF may include fever, muscle pains, headache, vomiting, diarrhea, and bleeding into the skin. Onset of symptoms is less than two weeks following exposure. Complications may include liver failure. Survivors generally recover around two weeks after onset.
The central nervous system (CNS) controls most of the functions of the body and mind. It comprises the brain, spinal cord and the nerve fibers that branch off to all parts of the body. The CNS viral diseases are caused by viruses that attack the CNS. Existing and emerging viral CNS infections are major sources of human morbidity and mortality.
Lujo is a bisegmented RNA virus—a member of the family Arenaviridae—and a known cause of viral hemorrhagic fever (VHF) in humans. Its name was suggested by the Special Pathogens Unit of the National Institute for Communicable Diseases of the National Health Laboratory Service (NICD-NHLS) by using the first two letters of the names of the cities involved in the 2008 outbreak of the disease, Lusaka (Zambia) and Johannesburg. It is the second pathogenic Arenavirus to be described from the African continent—the first being Lassa virus—and since 2012 has been classed as a "Select Agent" under U.S. law.
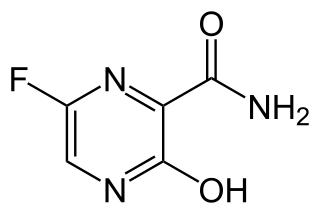
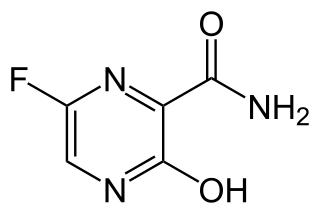
Favipiravir, sold under the brand name Avigan among others, is an antiviral medication used to treat influenza in Japan. It is also being studied to treat a number of other viral infections, including SARS-CoV-2. Like the experimental antiviral drugs T-1105 and T-1106, it is a pyrazinecarboxamide derivative.

The bat virome is the group of viruses associated with bats. Bats host a diverse array of viruses, including all seven types described by the Baltimore classification system: (I) double-stranded DNA viruses; (II) single-stranded DNA viruses; (III) double-stranded RNA viruses; (IV) positive-sense single-stranded RNA viruses; (V) negative-sense single-stranded RNA viruses; (VI) positive-sense single-stranded RNA viruses that replicate through a DNA intermediate; and (VII) double-stranded DNA viruses that replicate through a single-stranded RNA intermediate. The greatest share of bat-associated viruses identified as of 2020 are of type IV, in the family Coronaviridae.

There have been several outbreaks of Nipah virus in Kerala, some of which have been traced to fruit bats. The National Institute of Virology in Pune confirmed the first case of Nipah virus in Kerala in May 2018.

Virus is a 2019 Indian Malayalam-language medical thriller film co-produced and directed by Aashiq Abu set against the backdrop of the 2018 Nipah virus outbreak in Kerala. The film was written by Muhsin Parari and Suhas-Sharfu. It stars an ensemble cast that includes Kunchacko Boban, Indrajith Sukumaran, Asif Ali, Tovino Thomas, Parvathy Thiruvothu, Rahman, Indrans, Jinu Joseph, Sreenath Bhasi, Dileesh Pothan, Rima Kallingal, Madonna Sebastian, Ramya Nambeeshan, Joju George, Soubin Shahir and Revathi.
Daniel R. Lucey is an American physician, researcher, senior scholar and adjunct professor of infectious diseases at Georgetown University, and a research associate in anthropology at the Smithsonian National Museum of Natural History, where he has co-organised an exhibition on eight viral outbreaks.

The 1998–1999 Malaysia Nipah virus outbreak was a Nipah virus outbreak occurring from September 1998 to May 1999 in the states of Perak, Negeri Sembilan and Selangor in Malaysia. A total of 265 cases of acute encephalitis with 105 deaths caused by the virus were reported in the three states throughout the outbreak. The Malaysian health authorities at first thought that Japanese encephalitis (JE) was the cause of the infection. This misunderstanding hampered the deployment of effective measures to prevent the spread, before the disease was identified by a local virologist from the Faculty of Medicine, University of Malaya as a newly discovered agent. It was named Nipah virus (NiV). The disease was as deadly as the Ebola virus disease (EVD), but attacked the brain system instead of the blood vessels. University of Malaya's Faculty of Medicine and the University of Malaya Medical Centre played a major role in serving as a major referral centre for the outbreak, treating majority of the Nipah patients and was instrumental in isolating the novel virus and researched on its features.
Ghanaian bat henipavirus (also known Kumasi virus belongs to the genus Henipavirus in the family Paramyxoviridae. Human infections are caused by zoonotic events where the virus crosses over from another animal species. Therefore, humans are not the innate host for this virus family but instead become infected by peripheral viral reservoirs such as bats and other carriers of the virus. When these virus are spread to humans through zoonotic events they have been found to be one of the most deadly viruses with the capability to infect humans, with mortality rates between 50 and 100%. Therefore, these viruses have been classified as a biosafety level four virus with regards to its pathogenesis when it infects humans.