Related Research Articles

Health informatics is the study and implementation of computer structures and algorithms to improve communication, understanding, and management of medical information. It can be viewed as branch of engineering and applied science.

The terms medical record, health record and medical chart are used somewhat interchangeably to describe the systematic documentation of a single patient's medical history and care across time within one particular health care provider's jurisdiction. A medical record includes a variety of types of "notes" entered over time by healthcare professionals, recording observations and administration of drugs and therapies, orders for the administration of drugs and therapies, test results, X-rays, reports, etc. The maintenance of complete and accurate medical records is a requirement of health care providers and is generally enforced as a licensing or certification prerequisite.

An electronic health record (EHR) is the systematized collection of patient and population electronically stored health information in a digital format. These records can be shared across different health care settings. Records are shared through network-connected, enterprise-wide information systems or other information networks and exchanges. EHRs may include a range of data, including demographics, medical history, medication and allergies, immunization status, laboratory test results, radiology images, vital signs, personal statistics like age and weight, and billing information.
eHealth describes healthcare services which are supported by digital processes, communication or technology such as electronic prescribing, Telehealth, or Electronic Health Records (EHRs). The use of electronic processes in healthcare dated back to at least the 1990s. Usage of the term varies as it covers not just "Internet medicine" as it was conceived during that time, but also "virtually everything related to computers and medicine". A study in 2005 found 51 unique definitions. Some argue that it is interchangeable with health informatics with a broad definition covering electronic/digital processes in health while others use it in the narrower sense of healthcare practice using the Internet. It can also include health applications and links on mobile phones, referred to as mHealth or m-Health. Key components of eHealth include electronic health records (EHRs), telemedicine, health information exchange, mobile health applications, wearable devices, and online health information. These technologies enable healthcare providers, patients, and other stakeholders to access, manage, and exchange health information more effectively, leading to improved communication, decision-making, and overall healthcare outcomes.
A clinical decision support system (CDSS) is a health information technology that provides clinicians, staff, patients, and other individuals with knowledge and person-specific information to help health and health care. CDSS encompasses a variety of tools to enhance decision-making in the clinical workflow. These tools include computerized alerts and reminders to care providers and patients, clinical guidelines, condition-specific order sets, focused patient data reports and summaries, documentation templates, diagnostic support, and contextually relevant reference information, among other tools. CDSSs constitute a major topic in artificial intelligence in medicine.
Protected health information (PHI) under U.S. law is any information about health status, provision of health care, or payment for health care that is created or collected by a Covered Entity, and can be linked to a specific individual. This is interpreted rather broadly and includes any part of a patient's medical record or payment history.
Patient portals are healthcare-related online applications that allow patients to interact and communicate with their healthcare providers, such as physicians and hospitals. Typically, portal services are available on the Internet at all hours of the day and night. Some patient portal applications exist as stand-alone web sites and sell their services to healthcare providers. Other portal applications are integrated into the existing web site of a healthcare provider. Still others are modules added onto an existing electronic medical record (EMR) system. What all of these services share is the ability of patients to interact with their medical information via the Internet. Currently, the lines between an EMR, a personal health record, and a patient portal are blurring. For example, Intuit Health and Microsoft HealthVault describe themselves as personal health records (PHRs), but they can interface with EMRs and communicate through the Continuity of Care Record standard, displaying patient data on the Internet so it can be viewed through a patient portal.
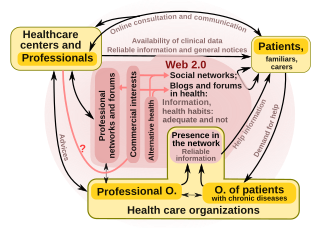
"Health 2.0" is a term introduced in the mid-2000s, as the subset of health care technologies mirroring the wider Web 2.0 movement. It has been defined variously as including social media, user-generated content, and cloud-based and mobile technologies. Some Health 2.0 proponents see these technologies as empowering patients to have greater control over their own health care and diminishing medical paternalism. Critics of the technologies have expressed concerns about possible misinformation and violations of patient privacy.
Health information technology (HIT) is health technology, particularly information technology, applied to health and health care. It supports health information management across computerized systems and the secure exchange of health information between consumers, providers, payers, and quality monitors. Based on a 2008 report on a small series of studies conducted at four sites that provide ambulatory care – three U.S. medical centers and one in the Netherlands, the use of electronic health records (EHRs) was viewed as the most promising tool for improving the overall quality, safety and efficiency of the health delivery system.
The Office of the National Coordinator for Health Information Technology (ONC) is a staff division of the Office of the Secretary, within the U.S. Department of Health and Human Services. ONC leads national health IT efforts, charged as the principal federal entity to coordinate nationwide efforts to implement and use the most advanced health information technology and the electronic exchange of health information.
Clinical point of care (POC) is the point in time when clinicians deliver healthcare products and services to patients at the time of care.
The Fast Healthcare Interoperability Resources standard is a set of rules and specifications for exchanging electronic health care data. It is designed to be flexible and adaptable, so that it can be used in a wide range of settings and with different health care information systems. The goal of FHIR is to enable the seamless and secure exchange of health care information, so that patients can receive the best possible care. The standard describes data formats and elements and an application programming interface (API) for exchanging electronic health records (EHR). The standard was created by the Health Level Seven International (HL7) health-care standards organization.
Digital health is a discipline that includes digital care programs, technologies with health, healthcare, living, and society to enhance the efficiency of healthcare delivery and to make medicine more personalized and precise. It uses information and communication technologies to facilitate understanding of health problems and challenges faced by people receiving medical treatment and social prescribing in more personalised and precise ways. The definitions of digital health and its remits overlap in many ways with those of health and medical informatics.
Health information on the Internet refers to all health-related information communicated through or available on the Internet.

OpenNotes is a research initiative and international movement located at Beth Israel Deaconess Medical Center.
Health care analytics is the health care analysis activities that can be undertaken as a result of data collected from four areas within healthcare; claims and cost data, pharmaceutical and research and development (R&D) data, clinical data, and patient behavior and sentiment data (patient behaviors and preferences,. Health care analytics is a growing industry in the United States, expected to grow to more than $31 billion by 2022. The industry focuses on the areas of clinical analysis, financial analysis, supply chain analysis, as well as marketing, fraud and HR analysis.

Artificial intelligence in healthcare is a term used to describe the use of machine-learning algorithms and software, or artificial intelligence (AI), to copy human cognition in the analysis, presentation, and understanding of complex medical and health care data, or to exceed human capabilities by providing new ways to diagnose, treat, or prevent disease. Specifically, AI is the ability of computer algorithms to arrive at approximate conclusions based solely on input data.
Health data is any data "related to health conditions, reproductive outcomes, causes of death, and quality of life" for an individual or population. Health data includes clinical metrics along with environmental, socioeconomic, and behavioral information pertinent to health and wellness. A plurality of health data are collected and used when individuals interact with health care systems. This data, collected by health care providers, typically includes a record of services received, conditions of those services, and clinical outcomes or information concerning those services. Historically, most health data has been sourced from this framework. The advent of eHealth and advances in health information technology, however, have expanded the collection and use of health data—but have also engendered new security, privacy, and ethical concerns. The increasing collection and use of health data by patients is a major component of digital health.
Federal and state governments, insurance companies and other large medical institutions are heavily promoting the adoption of electronic health records. The US Congress included a formula of both incentives and penalties for EMR/EHR adoption versus continued use of paper records as part of the Health Information Technology for Economic and Clinical Health (HITECH) Act, enacted as part of the, American Recovery and Reinvestment Act of 2009.

Dean Forrest Sittig is an American biomedical informatician specializing in clinical informatics. He is a professor in Biomedical Informatics at the University of Texas Health Science Center at Houston and Executive Director of the Clinical Informatics Research Collaborative (CIRCLE). Sittig was elected as a fellow of the American College of Medical Informatics in 1992, the Healthcare Information and Management Systems Society in 2011, and was a founding member of the International Academy of Health Sciences Informatics in 2017. Since 2004, he has worked with Joan S. Ash, a professor at Oregon Health & Science University to interview several Pioneers in Medical Informatics, including G. Octo Barnett, MD, Morris F. Collen, MD, Donald E. Detmer, MD, Donald A. B. Lindberg, MD, Nina W. Matheson, ML, DSc, Clement J. McDonald, MD, and Homer R. Warner, MD, PhD.
References
- 1 2 3 4 5 Tang, Paul; Ash, Joan; Bates, David; Overhage, J.; Sands, Daniel (2006). "Personal Health Records: Definitions, Benefits, and Strategies for Overcoming Barriers to Adoption". Journal of the American Medical Informatics Association. 13 (2): 121–126. doi:10.1197/jamia.M2025. PMC 1447551 . PMID 16357345.
- ↑ "Computerisation of personal health records". Health Visitor. 51 (6): 227. June 1978. PMID 248054.
- ↑ Dragstedt, CA (14 April 1956). "Personal health log". Journal of the American Medical Association. 160 (15): 1320. doi:10.1001/jama.1956.02960500050013. PMID 13306552.
- 1 2 AHIMA e-HIM Personal Health Record Work Group (July 2005). "The Role of the Personal Health Record in the EHR". Journal of AHIMA. 76 (7): 64A–D. PMID 16097127. Archived from the original on 20 September 2008.
- 1 2 Personal Health Working Group (1 July 2003). Connecting for Health: A Public-Private Collaborative (PDF) (Report). Markle Foundation. Archived from the original (PDF) on 4 January 2007.
- 1 2 America's Health Insurance Plans (13 December 2006). "What are Personal Health Records (PHRs)?". Archived from the original (DOC) on 5 March 2009.
- 1 2 3 4 5 Flaumenhaft, Y.; Ben-Assuli, O. (2018). "Personal health records, global policy and regulation review". Health Policy. 122 (8): 815–826. doi:10.1016/j.healthpol.2018.05.002. PMID 29884294. S2CID 46998430.
- ↑ "Personal Health Records and the HIPAA Privacy Rule" (PDF). Office of Civil Rights. U.S. Department of Health and Human Services. 15 December 2008. Archived (PDF) from the original on 17 February 2017.
- ↑ "MyChart". Cleveland Clinic. Retrieved 29 March 2011.
- 1 2 3 Archer, N.; Fevrier-Thomas, U.; Lokker, C.; et al. (2011). "Personal health records: A scoping review". Journal of the American Medical Informatics Association. 18 (4): 515–22. doi:10.1136/amiajnl-2011-000105. PMC 3128401 . PMID 21672914.
- 1 2 3 4 5 Assadi, V.; Hassanein, K. (2017). "Consumer Adoption of Personal Health Record Systems: A Self-Determination Theory Perspective". Journal of Medical Internet Research. 19 (7): e270. doi: 10.2196/jmir.7721 . PMC 5553007 . PMID 28751301.
- 1 2 3 4 5 Ford, E.W.; Hesse, B.W.; Huerta, T.R. (2016). "Personal Health Record Use in the United States: Forecasting Future Adoption Levels". Journal of Medical Internet Research. 18 (3): e73. doi: 10.2196/jmir.4973 . PMC 4830902 . PMID 27030105.
- ↑ "What is digital health technology and what can it do for me?". NIHR Evidence. 2022. doi:10.3310/nihrevidence_53447. S2CID 252584020.
- 1 2 3 Kaelber, David C.; Jha, Ashish K.; Johnston, Douglas; Middleton, Blackford; Bates, David W. (Nov–Dec 2008). "A Research Agenda for Personal Health Records (PHRs)". Journal of the American Medical Informatics Association. 15 (6): 729–36. doi:10.1197/jamia.M2547. PMC 2585530 . PMID 18756002.
- ↑ Roehrs, A.; da Costa, C.A.; da Rosa Righi, R.; de Oliveira, K.S.F. (2017). "Personal Health Records: A Systematic Literature Review". Journal of Medical Internet Research. 19 (1): e13. doi: 10.2196/jmir.5876 . PMC 5251169 . PMID 28062391.
- ↑ UK Department of Health (1993). Changing Childbirth, Part II: Survey of good communications practice in maternity services. London: HMSO. pp. 25–26. ISBN 978-0-11-321623-9. OCLC 925009321.
- ↑ "Scottish Woman Held Maternity Record". Healthcare Improvement Scotland. NHS Scotland. Retrieved 2 January 2015.
- ↑ "All Wales Maternity Record (Cofnod Mamolaeth Cymru Gyfan)". All Wales Child Protection Procedures Review Group. 8 July 2008. Archived from the original (PDF) on 27 June 2013.
- ↑ "About the notes". Perinatal Institute. Archived from the original on 17 May 2013.
- ↑ Fawdry, R; Bewley, S; Cumming, G; Perry, H (2011). "Data re-entry overload: time for a paradigm shift in maternity IT?". Journal of the Royal Society of Medicine. 104 (10): 405–412. doi: 10.1258/jrsm.2011.110153 . PMC 3184532 . PMID 21969478.
- ↑ Kardas G, Tunali ET; Tunali (Jan 2006). "Design and implementation of a smart-card-based healthcare information system". Comput Methods Programs Biomed. 81 (1): 66–78. doi:10.1016/j.cmpb.2005.10.006. PMID 16356586.(subscription required)
- ↑ Wright A, Sittig DF; Sittig (2007). "Encryption Characteristics of Two USB-based Personal Health Record Devices". J Am Med Inform Assoc. 14 (4): 397–9. doi:10.1197/jamia.M2352. PMC 2244899 . PMID 17460132.
- ↑ Brown, Aaron; Weihl, Bill (24 June 2011). "An update on Google Health and Google PowerMeter". The Official Google Blog. Retrieved 19 December 2011.
- 1 2 Lohr, Steve (2011-06-24). "Google Is Closing Its Health Records Service". The New York Times. ISSN 0362-4331 . Retrieved 2016-12-10.
- ↑ Fernández-Alemán, José Luis; Seva-Llor, Carlos Luis; Toval, Ambrosio; Ouhbi, Sofia; Fernández-Luque, Luis (2013-11-13). "Free Web-based Personal Health Records: An Analysis of Functionality". Journal of Medical Systems. 37 (6): 9990. doi:10.1007/s10916-013-9990-z. ISSN 0148-5598. PMID 24221916. S2CID 17143499.
- ↑ Menon, Shailaja; Singh, Hardeep; Meyer, Ashley N. D.; Belmont, Elisabeth; Sittig, Dean F. (2014-01-01). "Electronic health record-related safety concerns: a cross-sectional survey". Journal of Healthcare Risk Management. 34 (1): 14–26. doi:10.1002/jhrm.21146. ISSN 2040-0861. PMID 25070253.
- ↑ Paton, C.; Hansen, M.; Fernandez-Luque, L.; Lau, A. Y. S. (2012-01-01). "Self-Tracking, Social Media and Personal Health Records for Patient Empowered Self-Care. Contribution of the IMIA Social Media Working Group". Yearbook of Medical Informatics. 7: 16–24. ISSN 2364-0502. PMID 22890336.
- ↑ Gartrell, K.; Trinkoff, A. M.; Storr, C. L.; Wilson, M. L.; Gurses, A. P. (2015-01-01). "Testing the Electronic Personal Health Record Acceptance Model by Nurses for Managing Their Own Health: A Cross-sectional Survey". Applied Clinical Informatics. 6 (2): 224–247. doi:10.4338/ACI-2014-11-RA-0107. ISSN 1869-0327. PMC 4493327 . PMID 26171072.
- ↑ Braunstein, Mark (5 August 2014). "Free The Health Data: Grahame Grieve On FHIR". InformationWeek . Retrieved 22 November 2014.
- ↑ Kaelber, David; Pan, Eric (2008). "The Value of Personal Health Record (PHR) Systems". AMIA Annu Symp Proc. 2008: 343–347. PMC 2655982 . PMID 18999276.
- ↑ UK Department of Health (21 May 2012). "The power of information: giving people control of the health and care information they need". Gov.UK.
- ↑ Davies, Peter (30 July 2012). "Should patients be able to control their own records". BMJ. 345 (e4905): e4905. doi:10.1136/bmj.e4905. PMID 22846414. S2CID 41225013 . Retrieved 30 August 2012.(subscription required)
- ↑ Morgenthaler, John. "Moving Toward an Open Standard, Universal Health Record". Smart Publications. Archived from the original on 11 November 2007.
- 1 2 Kim, Matthew; Johnson, Kevin (2002). "Personal health records: evaluation of functionality and utility". Journal of the American Medical Informatics Association. 9 (2): 171–180. doi:10.1197/jamia.M0978. PMC 344574 . PMID 11861632.
- 1 2 Showell, C. (2017). "Barriers to the use of personal health records by patients: A structured review". PeerJ. 5: e3268. doi: 10.7717/peerj.3268 . PMC 5410160 . PMID 28462058.
- ↑ Lober, WB; Zierler, B; Herbaugh, AL; Shinstrom, SE; Stolyar, A; Kim, EH; Kim, Y (2006), "Barriers to the use of a Personal Health Record by an Elderly Population", AMIA Annu Symp Proc, vol. 2006, pp. 514–8, PMC 1839577 , PMID 17238394
- ↑ Liu, L.S.; Shih, P.C.; Hayes, G.R. (2011). "Barriers to the adoption and use of personal health record systems". Proceedings of the 2011 iConference. pp. 363–70. CiteSeerX 10.1.1.720.8152 . doi:10.1145/1940761.1940811. ISBN 9781450301213. S2CID 546214.
{{cite book}}: CS1 maint: date and year (link) - 1 2 3 4 Redling, R. (2012). "Personal Health Record Usage and Medical Practices". Physicians Practice. 22. Retrieved 29 June 2018.
- 1 2 3 Pushpangadan, S.; Seckman, C. (2015). "Consumer Perspective on Personal Health Records: A Review of the Literature". Online Journal of Nursing Informatics. 19 (1). Retrieved 29 June 2018.
- ↑ Office of the National Coordinator for Health Information Technology (February 2016). "Breaches of Unsecured Protected Health Information". Health IT Dashboard. Retrieved 3 July 2018.
- ↑ Cerrato, P. (28 June 2017). "Medical Data Breaches: The Latest Health Care Epidemic". GW Public Health Online Blog. Milken Institute School of Public Health, George Washington University. Retrieved 3 July 2018.
- 1 2 3 4 5 Weitzman, E.R.; Kelemen, S.; Kaci, L.; Mandl, K.D. (2012). "Willingness to share personal health record data for care improvement and public health: A survey of experienced personal health record users". BMC Medical Informatics and Decision Making. 12: 39. doi: 10.1186/1472-6947-12-39 . PMC 3403895 . PMID 22616619.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - 1 2 3 4 Ellison, A. (24 April 2014). "Top 3 Security Threats to the Healthcare Industry, Tips to Avoid Them". Becker's Health IT & CIO Report. Becker's Healthcare. Retrieved 3 July 2018.
- ↑ Health Information and Quality Authority (January 2012). "International Review of Secondary Use of Personal Health Information" (PDF). Health Information and Quality Authority. Retrieved 3 July 2018.
- ↑ Le Bris, A.; El Asri, W. (2017). "State of Cybersecurity & Cyber Threats in Healthcare Organizations: Applied Cybersecurity Strategy for Managers" (PDF). ESSEC Business School. Retrieved 3 July 2018.
- ↑ Davis, J. (21 March 2018). "OCR investigating Banner Health for 2016 breach of 3.7 million patient records". Healthcare IT News. HIMSS Media. Retrieved 3 July 2018.
- ↑ Sanborn, B.J. (20 April 2018). "UnityPoint Health System hit with cyberattack affecting 16,000 patients". Healthcare IT News. HIMSS Media. Retrieved 3 July 2018.
- ↑ Davis, J. (14 March 2018). "Medical data of 33,000 BJC HealthCare patients exposed online for 8 months". Healthcare IT News. HIMSS Media. Retrieved 3 July 2018.
- ↑ Davis, J. (12 January 2018). "Data of 43,000 patients breached after theft of unencrypted laptop". Healthcare IT News. HIMSS Media. Retrieved 3 July 2018.
- ↑ Sanborn, B.J. (23 May 2018). "LifeBridge Health reveals breach that compromised health data of 500,000 patients". Healthcare IT News. HIMSS Media. Retrieved 3 July 2018.
- ↑ Chouffani, R. (June 2018). "Medical records privacy a concern with increased mobile use". TechTarget SearchHealthIT. TechTarget. Retrieved 3 July 2018.
- ↑ Al-Sahan, A.; Saddik, B. (2016). "Perceived challenges for adopting the Personal Health Record (PHR) at Ministry of National Guard Health Affairs (MNGHA)- Riyadh". Online Journal of Public Health Informatics. 8 (3): e205. doi: 10.5210/ojphi.v8i3.6845 . PMC 5302467 . PMID 28210426.
- ↑ Bower, JK; Bollinger, CE; Foraker, RE; Hood, DB; Shoben, AB; Lai, AM (2017). "Active Use of Electronic Health Records (EHRs) and Personal Health Records (PHRs) for Epidemiologic Research: Sample Representativeness and Nonresponse Bias in a Study of Women During Pregnancy". eGEMs. 5 (1): 1263. doi:10.13063/2327-9214.1263. PMC 5340503 . PMID 28303255.
- 1 2 Bonander, J; Gates, S (2010). "Public health in an era of personal health records: Opportunities for innovation and new partnerships". Journal of Medical Internet Research. 12 (3): e33. doi: 10.2196/jmir.1346 . PMC 2956336 . PMID 20699216.
- 1 2 Lake Research Partners; American Viewpoint (1 November 2006). "Survey Finds Americans Want Electronic Personal Health Information to Improve Own Health Care" (PDF). Markle Foundation. Retrieved 29 June 2018.
{{cite web}}: CS1 maint: multiple names: authors list (link) - 1 2 King, R.J.; Garrett, N.; Kriseman, J.; et al. (2016). "A Community Health Record: Improving Health Through Multisector Collaboration, Information Sharing, and Technology". Preventing Chronic Disease. 13: 160101. doi:10.5888/pcd13.160101. PMC 5027852 . PMID 27609300.
- ↑ Investigating Decentralized Management of Health and Fitness Data