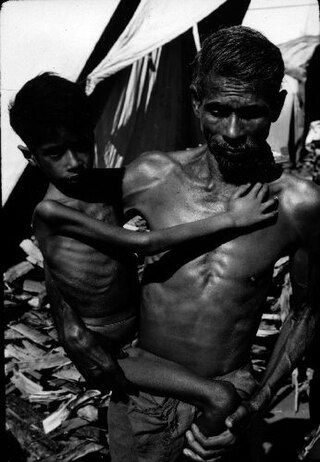
Kwashiorkor is a form of severe protein malnutrition characterized by edema and an enlarged liver with fatty infiltrates. It is thought to be caused by sufficient calorie intake, but with insufficient protein consumption, which distinguishes it from marasmus. Recent studies have found that a lack of antioxidant micronutrients such as β-carotene, lycopene, other carotenoids, and vitamin C as well as the presence of aflatoxins may play a role in the development of the disease. However, the exact cause of kwashiorkor is still unknown. Inadequate food supply is correlated with occurrences of kwashiorkor; occurrences in high income countries are rare. It occurs amongst weaning children to ages of about five years old.

Human nutrition deals with the provision of essential nutrients in food that are necessary to support human life and good health. Poor nutrition is a chronic problem often linked to poverty, food security, or a poor understanding of nutritional requirements. Malnutrition and its consequences are large contributors to deaths, physical deformities, and disabilities worldwide. Good nutrition is necessary for children to grow physically and mentally, and for normal human biological development.

Malnutrition occurs when an organism gets too few or too many nutrients, resulting in health problems. Specifically, it is "a deficiency, excess, or imbalance of energy, protein and other nutrients" which adversely affects the body's tissues and form. Malnutrition is not receiving the correct amount of nutrition.
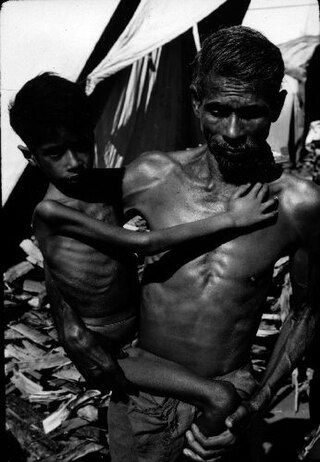
Marasmus is a form of severe malnutrition characterized by energy deficiency. It can occur in anyone with severe malnutrition but usually occurs in children. Body weight is reduced to less than 62% of the normal (expected) body weight for the age. Marasmus occurrence increases prior to age 1, whereas kwashiorkor occurrence increases after 18 months. It can be distinguished from kwashiorkor in that kwashiorkor is protein deficiency with adequate energy intake whereas marasmus is inadequate energy intake in all forms, including protein. This clear-cut separation of marasmus and kwashiorkor is however not always clinically evident as kwashiorkor is often seen in a context of insufficient caloric intake, and mixed clinical pictures, called marasmic kwashiorkor, are possible. Protein wasting in kwashiorkor generally leads to edema and ascites, while muscular wasting and loss of subcutaneous fat are the main clinical signs of marasmus, which makes the ribs and joints protrude.

India's population in 2021 as per World Bank is 1.39 billion. Being the world's most populous country and one of its fastest-growing economies, India experiences both challenges and opportunities in context of public health. India is a hub for pharmaceutical and biotechnology industries; world-class scientists, clinical trials and hospitals yet country faces daunting public health challenges like child undernutrition, high rates of neonatal and maternal mortality, growth in noncommunicable diseases, high rates of road traffic accidents and other health related issues.
Food fortification or enrichment is the process of adding micronutrients to food. It can be carried out by food manufacturers, or by governments as a public health policy which aims to reduce the number of people with dietary deficiencies within a population. The predominant diet within a region can lack particular nutrients due to the local soil or from inherent deficiencies within the staple foods; the addition of micronutrients to staples and condiments can prevent large-scale deficiency diseases in these cases.

Protein–energy undernutrition (PEU), once called protein-energy malnutrition (PEM), is a form of malnutrition that is defined as a range of conditions arising from coincident lack of dietary protein and/or energy (calories) in varying proportions. The condition has mild, moderate, and severe degrees.
Health can affect intelligence in various ways. Conversely, intelligence can affect health. Health effects on intelligence have been described as being among the most important factors in the origins of human group differences in IQ test scores and other measures of cognitive ability. Several factors can lead to significant cognitive impairment, particularly if they occur during pregnancy and childhood when the brain is growing and the blood–brain barrier of the child is less effective. Such impairment may sometimes be permanent, sometimes be partially or wholly compensated for by later growth.
Health care services in Nepal are provided by both public and private sectors and are generally regarded as failing to meet international standards. Prevalence of disease is significantly higher in Nepal than in other South Asian countries, especially in rural areas. Moreover, the country's topographical and sociological diversity results in periodic epidemics of infectious diseases, epizootics and natural hazards such as floods, forest fires, landslides, and earthquakes. But, recent surge in Non communicable diseases has emerged as the main public health concern and this accounts for more than two-thirds of total mortality in country. A large section of the population, particularly those living in rural poverty, are at risk of infection and mortality by communicable diseases, malnutrition and other health-related events. Nevertheless, some improvements in health care can be witnessed; most notably, there has been significant improvement in the field of maternal health. These improvements include:

Micronutrient deficiency is defined as the sustained insufficient supply of vitamins and minerals needed for growth and development, as well as to maintain optimal health. Since some of these compounds are considered essentials, micronutrient deficiencies are often the result of an inadequate intake. However, it can also be associated to poor intestinal absorption, presence of certain chronic illnesses and elevated requirements.

Biofortification is the idea of breeding crops to increase their nutritional value. This can be done either through conventional selective breeding, or through genetic engineering. Biofortification differs from ordinary fortification because it focuses on making plant foods more nutritious as the plants are growing, rather than having nutrients added to the foods when they are being processed. This is an important improvement on ordinary fortification when it comes to providing nutrients for the rural poor, who rarely have access to commercially fortified foods. As such, biofortification is seen as an upcoming strategy for dealing with deficiencies of micronutrients in low and middle-income countries. In the case of iron, the WHO estimated that biofortification could help cure the 2 billion people suffering from iron deficiency-induced anemia.
Despite India's 50% increase in GDP since 2013, more than one third of the world's malnourished children live in India. Among these, half of the children under three years old are underweight.
The Save the Children State of the World's Mothers report (SOWM report) is an annual report by the Save the Children USA, which compiles statistics on the health of mothers and children and uses them to produce rankings of more than 170 countries, showing where mothers fare best and where they face the greatest hardships. The rankings are presented in the Mothers’ Index, which has been produced annually since the year 2000.
Malnutrition continues to be a problem in the Republic of South Africa, although it is not as common as in other countries of Sub-Saharan Africa.

Both maternal and child health are interdependent and substantially contributing to high burden of mortality worldwide. Every year, 289 000 women die due to complications in pregnancy and childbirth, and 6.6 million children below 5 years of age die of complications in the newborn period and of common childhood diseases. Sub-Saharan Africa (SSA), which includes Tanzania, contribute higher proportion of maternal and child mortality. Due to considerable proportion of mortality being attributed by maternal and child health, the United Nations together with other international agencies incorporated the two into Millennium Development Goals (MDGs) 4 and 5. In this regard, Tanzania through the Ministry of Health and Social Welfare (MoHSW) adopted different strategies and efforts to promote safe motherhood and improve child survival. Similarly, in an effort to improve maternal and child health, Tanzania's government has declared maternal and child health services to be exempt from user fees in government facilities.
Malnutrition is a condition that affects bodily capacities of an individual, including growth, pregnancy, lactation, resistance to illness, and cognitive and physical development. Malnutrition is commonly used in reference to undernourishment, or a condition in which an individual's diet does not include sufficient calories and proteins to sustain physiological needs, but it also includes overnourishment, or the consumption of excess calories.

Environmental enteropathy is an acquired small intestinal disorder characterized by gut inflammation, reduced absorptive surface area in small intestine, and disruption of intestinal barrier function. EE is most common amongst children living in low-resource settings. Acute symptoms are typically minimal or absent. EE can lead to malnutrition, anemia, stunted growth, impaired brain development, and impaired response to oral vaccinations.

Undernutrition in children, occurs when children do not consume enough calories, protein, or micronutrients to maintain good health. It is common globally and may result in both short and long term irreversible adverse health outcomes. Undernutrition is sometimes used synonymously with malnutrition, however, malnutrition could mean both undernutrition or overnutrition. The World Health Organization (WHO) estimates that malnutrition accounts for 54 percent of child mortality worldwide, which is about 1 million children. Another estimate, also by WHO, states that childhood underweight is the cause for about 35% of all deaths of children under the age of five worldwide.

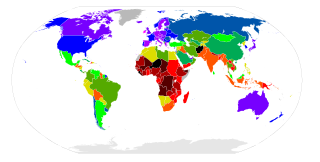
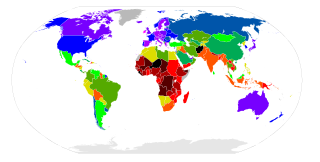
Child health and nutrition in Africa is concerned with the health care of children through adolescents in the various countries of Africa. The right to health and a nutritious and sufficient diet are internationally recognized human rights that are protected by international treaties. Millennium Development Goals (MDGs) 1, 4, 5 and 6 highlight, respectively, how poverty, hunger, child mortality, maternal health, the eradication of HIV/AIDS, malaria, tuberculosis and other diseases are of particular significance in the context of child health.
The first 1,000 days describes the period from conception to 24 months of age in child development. This is considered a "critical period" in which sufficient nutrition and environmental factors have life-long effects on a child's overall health. While adequate nutrition can be exceptionally beneficial during this critical period, inadequate nutrition may also be detrimental to the child. This is because children establish many of their lifetime epigenetic characteristics in their first 1,000 days. Medical and public health interventions early on in child development during the first 1,000 days may have higher rates of success compared to those achieved outside of this period.