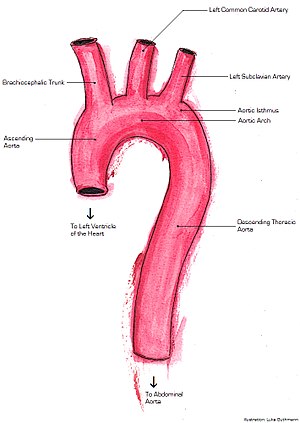
The aorta is the main and largest artery in the human body, originating from the left ventricle of the heart, branching upwards immediately after, and extending down to the abdomen, where it splits at the aortic bifurcation into two smaller arteries. The aorta distributes oxygenated blood to all parts of the body through the systemic circulation.

Aortic dissection (AD) occurs when an injury to the innermost layer of the aorta allows blood to flow between the layers of the aortic wall, forcing the layers apart. In most cases, this is associated with a sudden onset of severe chest or back pain, often described as "tearing" in character. Also, vomiting, sweating, and lightheadedness may occur. Other symptoms may result from decreased blood supply to other organs, such as stroke, lower extremity ischemia, or mesenteric ischemia. Aortic dissection can quickly lead to death from insufficient blood flow to the heart or complete rupture of the aorta.
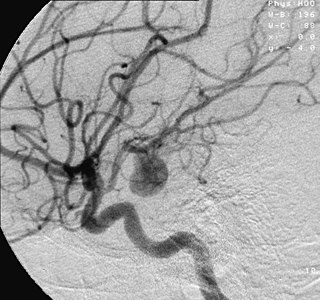
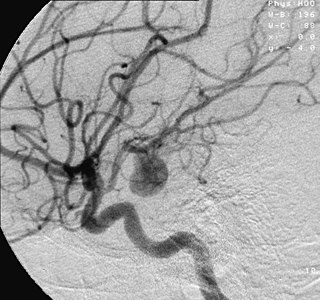
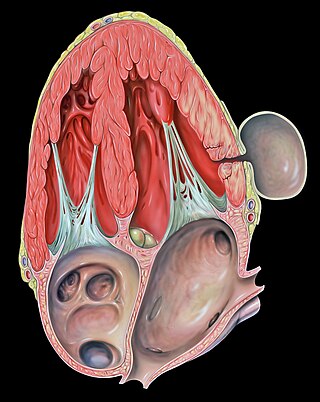
An aneurysm is an outward bulging, likened to a bubble or balloon, caused by a localized, abnormal, weak spot on a blood vessel wall. Aneurysms may be a result of a hereditary condition or an acquired disease. Aneurysms can also be a nidus for clot formation (thrombosis) and embolization. As an aneurysm increases in size, the risk of rupture, which leads to uncontrolled bleeding, increases. Although they may occur in any blood vessel, particularly lethal examples include aneurysms of the Circle of Willis in the brain, aortic aneurysms affecting the thoracic aorta, and abdominal aortic aneurysms. Aneurysms can arise in the heart itself following a heart attack, including both ventricular and atrial septal aneurysms. There are congenital atrial septal aneurysms, a rare heart defect.

Interventional radiology (IR) is a medical specialty that performs various minimally-invasive procedures using medical imaging guidance, such as x-ray fluoroscopy, computed tomography, magnetic resonance imaging, or ultrasound. IR performs both diagnostic and therapeutic procedures through very small incisions or body orifices. Diagnostic IR procedures are those intended to help make a diagnosis or guide further medical treatment, and include image-guided biopsy of a tumor or injection of an imaging contrast agent into a hollow structure, such as a blood vessel or a duct. By contrast, therapeutic IR procedures provide direct treatment—they include catheter-based medicine delivery, medical device placement, and angioplasty of narrowed structures.

Vascular surgery is a surgical subspecialty in which vascular diseases involving the arteries, veins, or lymphatic vessels, are managed by medical therapy, minimally-invasive catheter procedures and surgical reconstruction. The specialty evolved from general and cardiovascular surgery where it refined the management of just the vessels, no longer treating the heart or other organs. Modern vascular surgery includes open surgery techniques, endovascular techniques and medical management of vascular diseases - unlike the parent specialities. The vascular surgeon is trained in the diagnosis and management of diseases affecting all parts of the vascular system excluding the coronaries and intracranial vasculature. Vascular surgeons also are called to assist other physicians to carry out surgery near vessels, or to salvage vascular injuries that include hemorrhage control, dissection, occlusion or simply for safe exposure of vascular structures.

An aortic aneurysm is an enlargement (dilatation) of the aorta to greater than 1.5 times normal size. They usually cause no symptoms except when ruptured. Occasionally, there may be abdominal, back, or leg pain. The prevalence of abdominal aortic aneurysm ("AAA") has been reported to range from 2 to 12% and is found in about 8% of men more than 65 years of age. The mortality rate attributable to AAA is about 15,000 per year in the United States and 6,000 to 8,000 per year in the United Kingdom and Ireland. Between 2001 and 2006, there were approximately 230,000 AAA surgical repairs performed on Medicare patients in the United States.

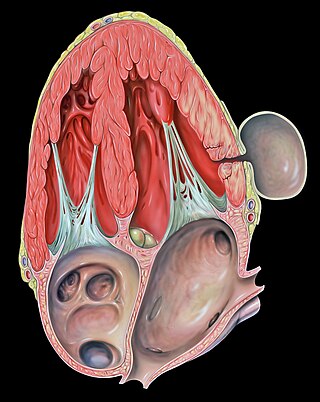
Abdominal aortic aneurysm (AAA) is a localized enlargement of the abdominal aorta such that the diameter is greater than 3 cm or more than 50% larger than normal. An AAA usually causes no symptoms, except during rupture. Occasionally, abdominal, back, or leg pain may occur. Large aneurysms can sometimes be felt by pushing on the abdomen. Rupture may result in pain in the abdomen or back, low blood pressure, or loss of consciousness, and often results in death.

A thoracic aortic aneurysm is an aortic aneurysm that presents primarily in the thorax.
A pseudoaneurysm, also known as a false aneurysm, is a locally contained hematoma outside an artery or the heart due to damage to the vessel wall. The injury passes through all three layers of the arterial wall, causing a leak, which is contained by a new, weak "wall" formed by the products of the clotting cascade. A pseudoaneurysm does not contain any layer of the vessel wall.

Blunt trauma, also known as blunt force trauma or non-penetrating trauma, is physical trauma or impactful force to a body part, often occurring with road traffic collisions, direct blows, assaults, injuries during sports, and particularly in the elderly who fall. It is contrasted with penetrating trauma which occurs when an object pierces the skin and enters a tissue of the body, creating an open wound and bruise.

A chest injury, also known as chest trauma, is any form of physical injury to the chest including the ribs, heart and lungs. Chest injuries account for 25% of all deaths from traumatic injury. Typically chest injuries are caused by blunt mechanisms such as direct, indirect, compression, contusion, deceleration, or blasts caused by motor vehicle collisions or penetrating mechanisms such as stabbings.
Hemoperitoneum is the presence of blood in the peritoneal cavity. The blood accumulates in the space between the inner lining of the abdominal wall and the internal abdominal organs. Hemoperitoneum is generally classified as a surgical emergency; in most cases, urgent laparotomy is needed to identify and control the source of the bleeding. In selected cases, careful observation may be permissible. The abdominal cavity is highly distensible and may easily hold greater than five liters of blood, or more than the entire circulating blood volume for an average-sized individual. Therefore, large-scale or rapid blood loss into the abdomen will reliably induce hemorrhagic shock and, if untreated, may rapidly lead to death.

Computed tomography angiography is a computed tomography technique used for angiography—the visualization of arteries and veins—throughout the human body. Using contrast injected into the blood vessels, images are created to look for blockages, aneurysms, dissections, and stenosis. CTA can be used to visualize the vessels of the heart, the aorta and other large blood vessels, the lungs, the kidneys, the head and neck, and the arms and legs. CTA can also be used to localise arterial or venous bleed of the gastrointestinal system.

Traumatic aortic rupture, also called traumatic aortic disruption or transection, is a condition in which the aorta, the largest artery in the body, is torn or ruptured as a result of trauma to the body. The condition is frequently fatal due to the profuse bleeding that results from the rupture. Since the aorta branches directly from the heart to supply blood to the rest of the body, the pressure within it is very great, and blood may be pumped out of a tear in the blood vessel very rapidly. This can quickly result in shock and death. Thus traumatic aortic rupture is a common killer in automotive accidents and other traumas, with up to 18% of deaths that occur in automobile collisions being related to the injury. In fact, aortic disruption due to blunt chest trauma is the second leading cause of injury death behind traumatic brain injury.

Endovascular aneurysm repair (EVAR) is a type of minimally-invasive endovascular surgery used to treat pathology of the aorta, most commonly an abdominal aortic aneurysm (AAA). When used to treat thoracic aortic disease, the procedure is then specifically termed TEVAR for "thoracic endovascular aortic/aneurysm repair." EVAR involves the placement of an expandable stent graft within the aorta to treat aortic disease without operating directly on the aorta. In 2003, EVAR surpassed open aortic surgery as the most common technique for repair of AAA, and in 2010, EVAR accounted for 78% of all intact AAA repair in the United States.

Aortic rupture is the rupture or breakage of the aorta, the largest artery in the body. Aortic rupture is a rare, extremely dangerous condition. The most common cause is an abdominal aortic aneurysm that has ruptured spontaneously. Aortic rupture is distinct from aortic dissection, which is a tear through the inner wall of the aorta that can block the flow of blood through the aorta to the heart or abdominal organs.

Familial aortic dissection or FAD refers to the splitting of the wall of the aorta in either the arch, ascending or descending portions. FAD is thought to be passed down as an autosomal dominant disease and once inherited will result in dissection of the aorta, and dissecting aneurysm of the aorta, or rarely aortic or arterial dilation at a young age. Dissection refers to the actual tearing open of the aorta. However, the exact gene(s) involved has not yet been identified. It can occur in the absence of clinical features of Marfan syndrome and of systemic hypertension. Over time this weakness, along with systolic pressure, results in a tear in the aortic intima layer thus allowing blood to enter between the layers of tissue and cause further tearing. Eventually complete rupture of the aorta occurs and the pleural cavity fills with blood. Warning signs include chest pain, ischemia, and hemorrhaging in the chest cavity. This condition, unless found and treated early, usually results in death. Immediate surgery is the best treatment in most cases. FAD is not to be confused with PAU and IMH, both of which present in ways similar to that of familial aortic dissection.

A hybrid cardiac surgical procedure in a narrow sense is defined as a procedure that combines a conventional, more invasive surgical part with an interventional part, using some sort of catheter-based procedure guided by fluoroscopy imaging in a hybrid operating room (OR) without interruption. The hybrid technique has a reduced risk of surgical complications and has shown decreased recovery time. It can be used to treat numerous heart diseases and conditions and with the increasing complexity of each case, the hybrid surgical technique is becoming more common.

Open aortic surgery (OAS), also known as open aortic repair (OAR), describes a technique whereby an abdominal, thoracic or retroperitoneal surgical incision is used to visualize and control the aorta for purposes of treatment, usually by the replacement of the affected segment with a prosthetic graft. OAS is used to treat aneurysms of the abdominal and thoracic aorta, aortic dissection, acute aortic syndrome, and aortic ruptures. Aortobifemoral bypass is also used to treat atherosclerotic disease of the abdominal aorta below the level of the renal arteries. In 2003, OAS was surpassed by endovascular aneurysm repair (EVAR) as the most common technique for repairing abdominal aortic aneurysms in the United States.

Inflammatory aortic aneurysm (IAA), also known as Inflammatory abdominal aortic aneurysm (IAAA), is a type of abdominal aortic aneurysm (AAA) where the walls of the aneurysm become thick and inflamed. Similar to AAA, IAA occurs in the abdominal region. IAA is closely associated and believed to be a response to and extensive peri-aneurysmal fibrosis, which is the formation of excess fibrous connective tissue in an organ or tissue in a reparative or reactive process IAA accounts for 5-10% of aortic aneurysms. IAA occurs mainly in a population that is on average younger by 10 years than most AAA patients. Some common symptoms of IAA may include back pain, abdominal tenderness, fevers, weight loss or elevated Erythrocyte sedimentation rate (ESR) levels. Corticosteroids and other immunosuppressive drugs have been found to decrease symptoms and the degree of peri-aortic inflammation and fibrosis