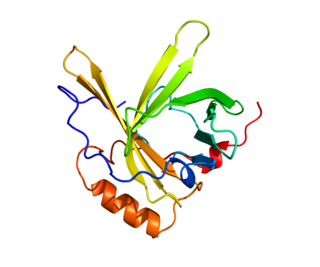
Apolipoprotein AI(Apo-AI) is a protein that in humans is encoded by the APOA1 gene. [5] [6] As the major component of HDL particles, it has a specific role in lipid metabolism.
Apolipoprotein AI(Apo-AI) is a protein that in humans is encoded by the APOA1 gene. [5] [6] As the major component of HDL particles, it has a specific role in lipid metabolism.
APOA1 is located on chromosome 11, with its specific location being 11q23-q24. The gene contains 4 exons. [7] The encoded apolipoprotein AI, is a 28.1 kDa protein composed of 243 amino acids; 21 peptides have been observed through mass spectrometry data. [8] [9] Due to alternative splicing, there exists multiple transcript variants of APOA1, including at least one which encodes a Apo-AI preprotein. [7]
Apolipoprotein AI is the major protein component of high density lipoprotein (HDL) particles in plasma. [10]
Chylomicrons secreted from the intestinal enterocyte also contain Apo-AI, but it is quickly transferred to HDL in the bloodstream. [11]
The protein, as a component of HDL particles, enables efflux of fat molecules by accepting fats from within cells (including macrophages within the walls of arteries which have become overloaded with ingested fats from oxidized LDL particles) for transport (in the water outside cells) elsewhere, including back to LDL particles or to the liver for excretion.
It is a cofactor for lecithin–cholesterol acyltransferase (LCAT) which is responsible for the formation of most plasma cholesteryl esters. Apolipoprotein AI has also been isolated as a prostacyclin (PGI2) stabilizing factor, and thus may have an anticlotting effect. [12] Defects in the gene encoding it are associated with HDL deficiencies, including Tangier disease, and with systemic non-neuropathic amyloidosis. [7]
Apo-AI is often used as a biomarker for prediction of cardiovascular diseases. The ratio apoB-100/apoA-I (i.e. LDL & larger particles vs. HDL particles), NMR measured lipoprotein (low density lipoprotein (LDL)/(HDL) particle ratios even more so, has always had a stronger correlation with myocardial infarction event rates than older methods of measuring lipid transport in the water outside cells. [13]
Apo-AI is routinely measured using immunoassays such as ELISA or nephelometry.
Apo-AI can be used to create in vitro lipoprotein nanodiscs for cell-free membrane expression systems. [14]
As a major component of the high-density lipoprotein complex (protective "fat removal" particles), Apo-AI helps to clear fats, including cholesterol, from white blood cells within artery walls, making the white blood cells (WBCs) less likely to become fat overloaded, transform into foam cells, die and contribute to progressive atheroma. Five of nine men found to carry a mutation (E164X) who were at least 35 years of age had developed premature coronary artery disease. [15] One of four mutants of Apo-AI is present in roughly 0.3% of the Japanese population, but is found in 6% of those with low HDL cholesterol levels. [16]
ApoA-I Milano is a naturally occurring mutant of Apo-AI, found in a few families in Limone sul Garda, Italy, and, by genetic + church record family tree detective work, traced to a single individual, Giovanni Pomarelli, in the 18th century. [17] Described in 1980, it was the first known molecular abnormality of apolipoproteins. [18] Paradoxically, carriers of this mutation have very low HDL-C (HDL-Cholesterol) levels, but no increase in the risk of heart disease, often living to age 100 or older. This unusual observation was what lead Italian investigators to track down what was going on and lead to the discovery of apoA-I Milano (the city, Milano, ~160 km away, in which the researcher's lab was located). Biochemically, apo A1 contains an extra cysteine bridge, causing it to exist as a homodimer or as a heterodimer with Apo-AII. However, the enhanced cardioprotective activity of this mutant (which likely depends on fat & cholesterol efflux) cannot easily be replicated by other cysteine mutants. [19]
Recombinant Apo-AI Milano dimers formulated into liposomes can reduce atheromas in animal models by up to 30%. [20] Apo-AI Milano has also been shown in small clinical trials to have a statistically significant effect in reducing (reversing) plaque build-up on arterial walls. [21] [22]
In human trials the reversal of plaque build-up was measured over the course of five weeks. [21] [23]
A study from 2008 describes two novel susceptibility haplotypes, P2-S2-X1 and P1-S2-X1, discovered in ApoAI-CIII-AIV gene cluster on chromosome 11q23, which confer approximately threefold higher risk of coronary heart disease in normal [24] as well as in the patients having type 2 diabetes mellitus. [25]
A G/A polymorphism in the promoter of the APOA1 gene has been associated with the age at which Alzheimer disease is presented. [26] Protection from Alzheimer's disease by Apo-AI may rely on a synergistic interaction with alpha-tocopherol. [27] Amyloid deposited in the knee following surgery consists largely of Apo-AI secreted from chondrocytes (cartilage cells). [28] A wide variety of amyloidosis symptoms are associated with rare APOA1 mutants.
Apo-AI binds to lipopolysaccharide or endotoxin, and has a major role in the anti-endotoxin function of HDL. [29]
In one study, a decrease in Apo-AI levels was detected in schizophrenia patients' CSF, brain and peripheral tissues. [30]
Apolipoprotein AI and ApoE interact epistatically to modulate triglyceride levels in coronary heart disease patients. Individually, neither Apo-AI nor ApoE was found to be associated with triglyceride (TG) levels, but pairwise epistasis (additive x additive model) explored their significant synergistic contributions with raised TG levels (P<0.01). [31]
In a study from 2005 it was reported, that Apo-AI production is decreased by calcitriol. It was concluded, that this regulation happens on transcription level: calcitriol alters yet unknown coactivators or corepressors, resulting in repression of APOA1 promoter activity. Simultaneously, Apo-AI production was increased by vitamin D antagonist, ZK-191784. [32]
Exercise or statin treatment may cause an increase in HDL-C levels by inducing Apo-AI production, but this depends on the G/A promoter polymorphism. [33]
Apolipoprotein A1 has been shown to interact with:
Apolipoprotein AI binding precursor, a relative of APOA-1 abbreviated APOA1BP, has a predicted biochemical interaction with carbohydrate kinase domain containing protein. The relationship between these two proteins is substantiated by cooccurance across genomes and coexpression. [37] The ortholog of CARKD in E. coli contains a domain not present in any eukaryotic ortholog. This domain has a high sequence identity to APOA1BP. CARKD is a protein of unknown function, and the biochemical basis for this interaction is unknown.
Click on genes, proteins and metabolites below to link to respective articles. [§ 1]
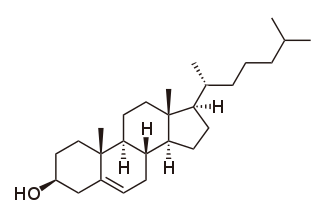
Cholesterol is the principal sterol of all higher animals, distributed in body tissues, especially the brain and spinal cord, and in animal fats and oils.
High-density lipoprotein (HDL) is one of the five major groups of lipoproteins. Lipoproteins are complex particles composed of multiple proteins which transport all fat molecules (lipids) around the body within the water outside cells. They are typically composed of 80–100 proteins per particle. HDL particles enlarge while circulating in the blood, aggregating more fat molecules and transporting up to hundreds of fat molecules per particle.

Low-density lipoprotein (LDL) is one of the five major groups of lipoprotein that transport all fat molecules around the body in extracellular water. These groups, from least dense to most dense, are chylomicrons, very low-density lipoprotein (VLDL), intermediate-density lipoprotein (IDL), low-density lipoprotein (LDL) and high-density lipoprotein (HDL). LDL delivers fat molecules to cells. LDL is involved in atherosclerosis, a process in which it is oxidized within the walls of arteries.

A lipoprotein is a biochemical assembly whose primary function is to transport hydrophobic lipid molecules in water, as in blood plasma or other extracellular fluids. They consist of a triglyceride and cholesterol center, surrounded by a phospholipid outer shell, with the hydrophilic portions oriented outward toward the surrounding water and lipophilic portions oriented inward toward the lipid center. A special kind of protein, called apolipoprotein, is embedded in the outer shell, both stabilising the complex and giving it a functional identity that determines its role.
Very-low-density lipoprotein (VLDL), density relative to extracellular water, is a type of lipoprotein made by the liver. VLDL is one of the five major groups of lipoproteins that enable fats and cholesterol to move within the water-based solution of the bloodstream. VLDL is assembled in the liver from triglycerides, cholesterol, and apolipoproteins. VLDL is converted in the bloodstream to low-density lipoprotein (LDL) and intermediate-density lipoprotein (IDL). VLDL particles have a diameter of 30–80 nanometers (nm). VLDL transports endogenous products, whereas chylomicrons transport exogenous (dietary) products. In the early 2010s both the lipid composition and protein composition of this lipoprotein were characterised in great detail.

Chylomicrons, also known as ultra low-density lipoproteins (ULDL), are lipoprotein particles that consist of triglycerides (85–92%), phospholipids (6–12%), cholesterol (1–3%), and proteins (1–2%). They transport dietary lipids, such as fats and cholesterol, from the intestines to other locations in the body, within the water-based solution of the bloodstream. ULDLs are one of the five major groups lipoproteins are divided into based on their density. A protein specific to chylomicrons is ApoB48.

Apolipoproteins are proteins that bind lipids to form lipoproteins. They transport lipids in blood, cerebrospinal fluid and lymph.
Hyperlipidemia is abnormally high levels of any or all lipids or lipoproteins in the blood. The term hyperlipidemia refers to the laboratory finding itself and is also used as an umbrella term covering any of various acquired or genetic disorders that result in that finding. Hyperlipidemia represents a subset of dyslipidemia and a superset of hypercholesterolemia. Hyperlipidemia is usually chronic and requires ongoing medication to control blood lipid levels.

The low-density lipoprotein receptor (LDL-R) is a mosaic protein of 839 amino acids that mediates the endocytosis of cholesterol-rich low-density lipoprotein (LDL). It is a cell-surface receptor that recognizes apolipoprotein B100 (ApoB100), which is embedded in the outer phospholipid layer of very low-density lipoprotein (VLDL), their remnants—i.e. intermediate-density lipoprotein (IDL), and LDL particles. The receptor also recognizes apolipoprotein E (ApoE) which is found in chylomicron remnants and IDL. In humans, the LDL receptor protein is encoded by the LDLR gene on chromosome 19. It belongs to the low density lipoprotein receptor gene family. It is most significantly expressed in bronchial epithelial cells and adrenal gland and cortex tissue.

Apolipoprotein E (Apo-E) is a protein involved in the metabolism of fats in the body of mammals. A subtype is implicated in Alzheimer's disease and cardiovascular diseases. It is encoded in humans by the gene APOE.

Apolipoprotein B (ApoB) is a protein that in humans is encoded by the APOB gene. It is commonly used to detect risk of atherosclerotic cardiovascular disease.

Apolipoprotein A-I Milano is a naturally occurring mutated variant of the apolipoprotein A1 protein found in human HDL, the lipoprotein particle that carries cholesterol from tissues to the liver and is associated with protection against cardiovascular disease. ApoA-I Milano was first identified by Dr. Cesare Sirtori in Milan, who also demonstrated that its presence significantly reduced cardiovascular disease, even though it caused a reduction in HDL levels and an increase in triglyceride levels.

Familial hypercholesterolemia (FH) is a genetic disorder characterized by high cholesterol levels, specifically very high levels of low-density lipoprotein cholesterol, in the blood and early cardiovascular diseases. The most common mutations diminish the number of functional LDL receptors in the liver or produce abnormal LDL receptors that never go to the cell surface to function properly. Since the underlying body biochemistry is slightly different in individuals with FH, their high cholesterol levels are less responsive to the kinds of cholesterol control methods which are usually more effective in people without FH. Nevertheless, treatment is usually effective.

Lipoprotein(a) is a low-density lipoprotein variant containing a protein called apolipoprotein(a). Genetic and epidemiological studies have identified lipoprotein(a) as a risk factor for atherosclerosis and related diseases, such as coronary heart disease and stroke.

Apolipoprotein C-III also known as apo-CIII, and apolipoprotein C3, is a protein that in humans is encoded by the APOC3 gene. Apo-CIII is secreted by the liver as well as the small intestine, and is found on triglyceride-rich lipoproteins such as chylomicrons, very low density lipoprotein (VLDL), and remnant cholesterol.
Apolipoprotein D (ApoD) is a protein that in humans is encoded by the APOD gene. Unlike other lipoproteins, which are mainly produced in the liver, apolipoprotein D is mainly produced in the brain and testes. It is a 29 kDa glycoprotein discovered in 1963 as a component of the high-density lipoprotein (HDL) fraction of human plasma. It is the major component of human mammary cyst fluid. The human gene encoding it was cloned in 1986 and the deduced protein sequence revealed that ApoD is a member of the lipocalin family, small hydrophobic molecule transporters. ApoD is 169 amino acids long, including a secretion peptide signal of 20 amino acids. It contains two glycosylation sites and the molecular weight of the mature protein varies from 20 to 32 kDa.
Endothelial lipase (LIPG) is a form of lipase secreted by vascular endothelial cells in tissues with high metabolic rates and vascularization, such as the liver, lung, kidney, and thyroid gland. The LIPG enzyme is a vital component to many biological processes. These processes include lipoprotein metabolism, cytokine expression, and lipid composition in cells. Unlike the lipases that hydrolyze Triglycerides, endothelial lipase primarily hydrolyzes phospholipids. Due to the hydrolysis specificity, endothelial lipase contributes to multiple vital systems within the body. On the contrary to the beneficial roles that LIPG plays within the body, endothelial lipase is thought to play a potential role in cancer and inflammation. Knowledge obtained in vitro and in vivo suggest the relations to these conditions, but human interaction knowledge lacks due to the recent discovery of endothelial lipase. Endothelial lipase was first characterized in 1999. The two independent research groups which are notable for this discovery cloned the endothelial lipase gene and identified the novel lipase secreted from endothelial cells. The anti-Atherosclerosis opportunity through alleviating plaque blockage and prospective ability to raise High-density lipoprotein (HDL) have gained endothelial lipase recognition.

ATP-binding cassette transporter ABCA1, also known as the cholesterol efflux regulatory protein (CERP) is a protein which in humans is encoded by the ABCA1 gene. This transporter is a major regulator of cellular cholesterol and phospholipid homeostasis.

Apolipoprotein A-V is a protein that in humans is encoded by the APOA5 gene on chromosome 11. It is significantly expressed in liver. The protein encoded by this gene is an apolipoprotein and an important determinant of plasma triglyceride levels, a major risk factor for coronary artery disease. It is a component of several lipoprotein fractions including VLDL, HDL, chylomicrons. It is believed that apoA-V affects lipoprotein metabolism by interacting with LDL-R gene family receptors. Considering its association with lipoprotein levels, APOA5 is implicated in metabolic syndrome. The APOA5 gene also contains one of 27 SNPs associated with increased risk of coronary artery disease.

Proprotein convertase subtilisin/kexin type 9 (PCSK9) is an enzyme encoded by the PCSK9 gene in humans on chromosome 1. It is the 9th member of the proprotein convertase family of proteins that activate other proteins. Similar genes (orthologs) are found across many species. As with many proteins, PCSK9 is inactive when first synthesized, because a section of peptide chains blocks their activity; proprotein convertases remove that section to activate the enzyme. The PCSK9 gene also contains one of 27 loci associated with increased risk of coronary artery disease.