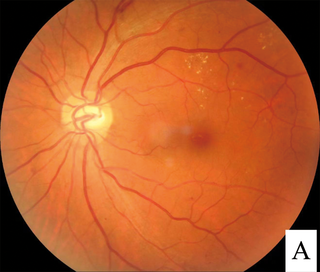
Retinopathy is any damage to the retina of the eyes, which may cause vision impairment. Retinopathy often refers to retinal vascular disease, or damage to the retina caused by abnormal blood flow. Age-related macular degeneration is technically included under the umbrella term retinopathy but is often discussed as a separate entity. Retinopathy, or retinal vascular disease, can be broadly categorized into proliferative and non-proliferative types. Frequently, retinopathy is an ocular manifestation of systemic disease as seen in diabetes or hypertension. Diabetes is the most common cause of retinopathy in the U.S. as of 2008. Diabetic retinopathy is the leading cause of blindness in working-aged people. It accounts for about 5% of blindness worldwide and is designated a priority eye disease by the World Health Organization.
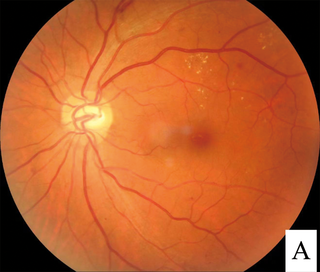
Diabetic retinopathy, is a medical condition in which damage occurs to the retina due to diabetes mellitus. It is a leading cause of blindness in developed countries.

Glaucoma is a group of eye diseases that lead to damage of the optic nerve, which transmits visual information from the eye to the brain. Glaucoma may cause vision loss if left untreated. It has been called the "silent thief of sight" because the loss of vision usually occurs slowly over a long period of time. A major risk factor for glaucoma is increased pressure within the eye, known as intraocular pressure (IOP). It is associated with old age, a family history of glaucoma, and certain medical conditions or medications. The word glaucoma comes from the Ancient Greek word γλαυκóς, meaning 'gleaming, blue-green, gray'.

Mydriasis is the dilation of the pupil, usually having a non-physiological cause, or sometimes a physiological pupillary response. Non-physiological causes of mydriasis include disease, trauma, or the use of certain types of drug. It may also be of unknown cause.
This is a partial list of human eye diseases and disorders.

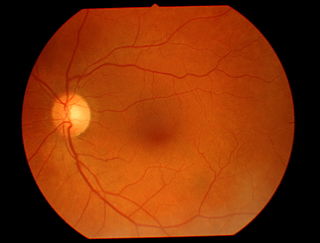
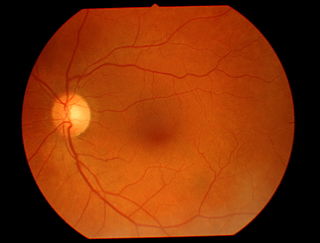
Ophthalmoscopy, also called funduscopy, is a test that allows a health professional to see inside the fundus of the eye and other structures using an ophthalmoscope. It is done as part of an eye examination and may be done as part of a routine physical examination. It is crucial in determining the health of the retina, optic disc, and vitreous humor.
Optic neuropathy is damage to the optic nerve from any cause. The optic nerve is a bundle of millions of fibers in the retina that sends visual signals to the brain. [1].
The red reflex refers to the reddish-orange reflection of light from the back of the eye, or fundus, observed when using an ophthalmoscope or retinoscope. The reflex relies on the transparency of optical media and reflects off the fundus back through media into the aperture of the ophthalmoscope. The red reflex is considered abnormal if there is any asymmetry between the eyes, dark spots, or white reflex (Leukocoria).
Ocular ischemic syndrome is the constellation of ocular signs and symptoms secondary to severe, chronic arterial hypoperfusion to the eye. Amaurosis fugax is a form of acute vision loss caused by reduced blood flow to the eye; it may be a warning sign of an impending stroke, as both stroke and retinal artery occlusion can be caused by thromboembolism due to atherosclerosis elsewhere in the body. Consequently, those with transient blurring of vision are advised to urgently seek medical attention for a thorough evaluation of the carotid artery. Anterior segment ischemic syndrome is a similar ischemic condition of anterior segment usually seen in post-surgical cases. Retinal artery occlusion leads to rapid death of retinal cells, thereby resulting in severe loss of vision.
The swinging-flashlight test, also known as the swinging light test, is used in medical examinations to identify a relative afferent pupillary defect.

Fundus photography involves photographing the rear of an eye, also known as the fundus. Specialized fundus cameras consisting of an intricate microscope attached to a flash enabled camera are used in fundus photography. The main structures that can be visualized on a fundus photo are the central and peripheral retina, optic disc and macula. Fundus photography can be performed with colored filters, or with specialized dyes including fluorescein and indocyanine green.

Intraocular hemorrhage is bleeding inside the eye. Bleeding can occur from any structure of the eye where there is vasculature or blood flow, including the anterior chamber, vitreous cavity, retina, choroid, suprachoroidal space, or optic disc.

Intraretinal microvascular abnormalities (IRMA) are abnormalities of the blood vessels that supply the retina of the eye, a sign of diabetic retinopathy. IRMA can be difficult to distinguish from and is likely a precursor to retinal neovascularization. One way to distinguish IRMA from retinal neovascularization is to perform fluorescein angiography. Since IRMA blood vessels are patent, unlike neovascular vessels, they do not leak, and therefore exhibit hyperfluorescence on fluorescein angiography.

Vitreous hemorrhage is the extravasation, or leakage, of blood into the areas in and around the vitreous humor of the eye. The vitreous humor is the clear gel that fills the space between the lens and the retina of the eye. A variety of conditions can result in blood leaking into the vitreous humor, which can cause impaired vision, floaters, and photopsia.
The eye is made up of the sclera, the iris, and the pupil, a black hole located at the center of the eye with the main function of allowing light to pass to the retina. Due to certain muscle spasms in the eye, the pupil can resemble a tadpole, which consists of a circular body, no arms or legs, and a tail.
Teleophthalmology is a branch of telemedicine that delivers eye care through digital medical equipment and telecommunications technology. Today, applications of teleophthalmology encompass access to eye specialists for patients in remote areas, ophthalmic disease screening, diagnosis and monitoring; as well as distant learning.
Photostress recovery time (PSRT) is the time taken for visual acuity to return to normal levels after the retina has been bleached by a bright light source. Photostress recovery time measurement procedure is known as photostress test. Normal recovery time is about 15–30 seconds.
Sickle cell retinopathy can be defined as retinal changes due to blood vessel damage in the eye of a person with a background of sickle cell disease. It can likely progress to loss of vision in late stages due to vitreous hemorrhage or retinal detachment. Sickle cell disease is a structural red blood cell disorder leading to consequences in multiple systems. It is characterized by chronic red blood cell destruction, vascular injury, and tissue ischemia causing damage to the brain, eyes, heart, lungs, kidneys, spleen, and musculoskeletal system.
Diabetic papillopathy is an ocular complication of diabetes mellitus characterized by optic disc swelling and edema of optic nerve head. The condition may affect both type 1 and type 2 diabetic patients.

The Heidelberg Retinal Tomography is a diagnostic procedure used in ophthalmology. The Heidelberg Retina Tomograph (HRT) is an ophthalmological confocal point scanning laser ophthalmoscope for examining the cornea and certain areas of the retina using different diagnostic modules. However, the most widely used area of application for HRT is the inspection of the optic nerve head (papilla) for early detection and follow-up of glaucoma. The procedure has established itself as an integral part of routine glaucoma diagnostics alongside the visual field examination (perimetry), the chamber angle examination (gonioscopy) and the measurement of intraocular pressure (tonometry). The HRT is the most widely used application of confocal scanning laser ophthalmoscopy.