| Hernia | |
|---|---|
 | |
| Diagram of an indirect inguinal hernia (view from the side) | |
| Specialty | General surgery |
| Symptoms | Pain especially with coughing, bulging area [1] |
| Complications | Bowel strangulation [1] |
| Usual onset | < 1 year and > 50 years old (groin hernias) [2] |
| Risk factors | Smoking, chronic obstructive pulmonary disease, obesity, pregnancy, peritoneal dialysis, collagen vascular disease, connective tissue disease [1] [2] [3] |
| Diagnostic method | Based on symptoms, medical imaging [1] |
| Treatment | Observation, surgery [1] |
| Frequency | 18.5 million (2015) [4] |
| Deaths | 59,800 (2015) [5] |
A hernia (pl.: hernias or herniae, from Latin, meaning 'rupture') is the abnormal exit of tissue or an organ, such as the bowel, through the wall of the cavity in which it normally resides. [1] The term is also used for the normal development of the intestinal tract, referring to the retraction of the intestine from the extra-embryonal navel coelom into the abdomen in the healthy embryo at about 7½ weeks.
Contents
- Pathogenesis
- Epidemiology
- Signs and symptoms
- Complications
- Causes
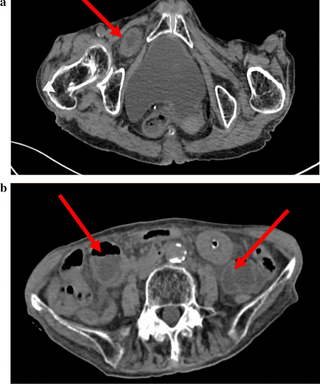
- Diagnosis
- Inguinal
- Femoral
- Umbilical
- Incisional
- Diaphragmatic
- Other hernias
- Treatment
- Truss
- Surgery
- Recovery
- References
- External links
Various types of hernias can occur, [6] most commonly involving the abdomen, and specifically the groin. [6] Groin hernias are most commonly inguinal hernias but may also be femoral hernias. [1] Other types of hernias include hiatus, incisional, and umbilical hernias. [6] Symptoms are present in about 66% of people with groin hernias. [1] This may include pain or discomfort in the lower abdomen, especially with coughing, exercise, or urinating or defecating. [1] Often, it gets worse throughout the day and improves when lying down. [1] A bulge may appear at the site of hernia, that becomes larger when bending down. [1]
Groin hernias occur more often on the right than left side. [1] The main concern is bowel strangulation, where the blood supply to part of the bowel is blocked. [1] This usually produces severe pain and tenderness in the area. [1] Hiatus, or hiatal hernias often result in heartburn but may also cause chest pain or pain while eating. [3]
Risk factors for the development of a hernia include smoking, chronic obstructive pulmonary disease, obesity, pregnancy, peritoneal dialysis, collagen vascular disease and previous open appendectomy, among others. [1] [2] [3] Predisposition to hernias is genetic [7] and occur more often in certain families. [8] [9] [10] [1] Deleterious mutations causing predisposition to hernias seem to have dominant inheritance (especially for men). It is unclear if groin hernias are associated with heavy lifting. [1] Hernias can often be diagnosed based on signs and symptoms. [1] Occasionally, medical imaging is used to confirm the diagnosis or rule out other possible causes. [1] The diagnosis of hiatus hernias is often done by endoscopy. [3]
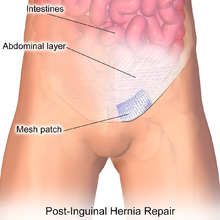
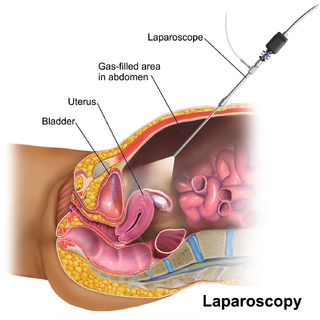
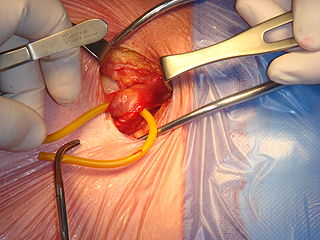
Groin hernias that do not cause symptoms in males do not need to be repaired. [1] Repair, however, is generally recommended in women due to the higher rate of femoral hernias, which have more complications. [1] If strangulation occurs, immediate surgery is required. [1] Repair may be done by open surgery, laparoscopic surgery, or robotic-assisted surgery. [1] Open surgery has the benefit of possibly being done under local anesthesia rather than general anesthesia. [1] Laparoscopic surgery generally has less pain following the procedure. [1] A hiatus hernia may be treated with lifestyle changes such as raising the head of the bed, weight loss and adjusting eating habits. [3] The medications H2 blockers or proton pump inhibitors may help. [3] If the symptoms do not improve with medications, a surgery known as laparoscopic Nissen fundoplication may be an option. [3]
Globally in 2019, there were 32.53 million prevalent cases of inguinal, femoral, and abdominal hernias, with a 95% uncertainty interval ranging from 27.71 to 37.79 million. Additionally, there were 13.02 million incident cases, with an uncertainty interval of 10.68 to 15.49 million. These figures reflect a 36.00% increase in prevalent cases and a 63.67% increase in incident cases compared to the numbers reported in 1990. [11] About 27% of males and 3% of females develop a groin hernia at some point in their lives. [1] Inguinal, femoral and abdominal hernias were present in 18.5 million people and resulted in 59,800 deaths in 2015. [4] [5] Groin hernias occur most often before the age of 1 and after the age of 50. [2] It is not known how commonly hiatus hernias occur, with estimates in North America varying from 10% to 80%. [3] The first known description of a hernia dates back to at least 1550 BC, in the Ebers Papyrus from Egypt. [12]