Bowel obstruction, also known as intestinal obstruction, is a mechanical or functional obstruction of the intestines which prevents the normal movement of the products of digestion. Either the small bowel or large bowel may be affected. Signs and symptoms include abdominal pain, vomiting, bloating and not passing gas. Mechanical obstruction is the cause of about 5 to 15% of cases of severe abdominal pain of sudden onset requiring admission to hospital.

Ischemia or ischaemia is a restriction in blood supply to any tissue, muscle group, or organ of the body, causing a shortage of oxygen that is needed for cellular metabolism. Ischemia is generally caused by problems with blood vessels, with resultant damage to or dysfunction of tissue i.e. hypoxia and microvascular dysfunction. It also implies local hypoxia in a part of a body resulting from constriction.

Enteritis is inflammation of the small intestine. It is most commonly caused by food or drink contaminated with pathogenic microbes, such as Serratia, but may have other causes such as NSAIDs, radiation therapy as well as autoimmune conditions like coeliac disease. Symptoms include abdominal pain, cramping, diarrhoea, dehydration, and fever. Related diseases of the gastrointestinal system involve inflammation of the stomach and large intestine.

Vascular surgery is a surgical subspecialty in which vascular diseases involving the arteries, veins, or lymphatic vessels, are managed by medical therapy, minimally-invasive catheter procedures and surgical reconstruction. The specialty evolved from general and cardiovascular surgery where it refined the management of just the vessels, no longer treating the heart or other organs. Modern vascular surgery includes open surgery techniques, endovascular techniques and medical management of vascular diseases - unlike the parent specialities. The vascular surgeon is trained in the diagnosis and management of diseases affecting all parts of the vascular system excluding the coronaries and intracranial vasculature. Vascular surgeons also are called to assist other physicians to carry out surgery near vessels, or to salvage vascular injuries that include hemorrhage control, dissection, occlusion or simply for safe exposure of vascular structures.

Abdominal pain, also known as a stomach ache, is a symptom associated with both non-serious and serious medical issues. Since the abdomen contains most of the body's vital organs, it can be an indicator of a wide variety of diseases. Given that, approaching the examination of a person and planning of a differential diagnosis is extremely important.

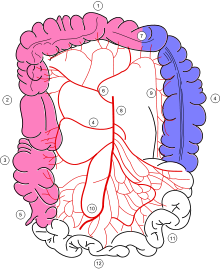
Gastrointestinal diseases refer to diseases involving the gastrointestinal tract, namely the esophagus, stomach, small intestine, large intestine and rectum, and the accessory organs of digestion, the liver, gallbladder, and pancreas.

A volvulus is when a loop of intestine twists around itself and the mesentery that supports it, resulting in a bowel obstruction. Symptoms include abdominal pain, abdominal bloating, vomiting, constipation, and bloody stool. Onset of symptoms may be rapid or more gradual. The mesentery may become so tightly twisted that blood flow to part of the intestine is cut off, resulting in ischemic bowel. In this situation there may be fever or significant pain when the abdomen is touched.

Diverticular disease is when problems occur due to diverticulosis, a benign condition defined by the formation of pouches (diverticula) from the weak spots in the wall of the large intestine. This disease spectrum includes diverticulitis, symptomatic uncomplicated diverticular disease (SUDD), and segmental colitis associated with diverticulosis (SCAD). The most common symptoms across the disease spectrum are abdominal pain and bowel habit changes such as diarrhea or constipation. Otherwise, diverticulitis presents with systemic symptoms such as fever and elevated white blood cell count whereas SUDD and SCAD don’t. Treatment ranges from conservative bowel rest to medications such as antibiotics, antispasmodics, acetaminophen, mesalamine, rifaximin, and corticosteroids depending on the specific conditions.
Intestinal malrotation is a congenital anomaly of rotation of the midgut. It occurs during the first trimester as the fetal gut undergoes a complex series of growth and development. Malrotation can lead to a dangerous complication called volvulus, in which cases emergency surgery is indicated. Malrotation can refer to a spectrum of abnormal intestinal positioning, often including:

Lower gastrointestinal bleeding, commonly abbreviated LGIB, is any form of gastrointestinal bleeding in the lower gastrointestinal tract. LGIB is a common reason for seeking medical attention at a hospital's emergency department. LGIB accounts for 30–40% of all gastrointestinal bleeding and is less common than upper gastrointestinal bleeding (UGIB). It is estimated that UGIB accounts for 100–200 per 100,000 cases versus 20–27 per 100,000 cases for LGIB. Approximately 85% of lower gastrointestinal bleeding involves the colon, 10% are from bleeds that are actually upper gastrointestinal bleeds, and 3–5% involve the small intestine.

Ogilvie syndrome, or acute colonic pseudo-obstruction is the acute dilatation of the colon in the absence of any mechanical obstruction in severely ill patients.
An acute abdomen refers to a sudden, severe abdominal pain. It is in many cases a medical emergency, requiring urgent and specific diagnosis. Several causes need immediate surgical treatment.
Abdominal angina is abdominal pain after eating that occurs in individuals with ongoing poor blood supply to their small intestines known as chronic mesenteric ischemia. Although the term angina alone usually denotes angina pectoris, angina by itself can also mean "any spasmodic, choking, or suffocative pain", with an anatomic adjective defining its focus; so, in this case, spasmodic pain in the abdomen. Stedman's Medical Dictionary Online defines abdominal angina as "intermittent abdominal pain, frequently occurring at a fixed time after eating, caused by inadequacy of the mesenteric circulation resulting from arteriosclerosis or other arterial disease. Synonym: intestinal angina."

A bowel resection or enterectomy is a surgical procedure in which a part of an intestine (bowel) is removed, from either the small intestine or large intestine. Often the word enterectomy is reserved for the sense of small bowel resection, in distinction from colectomy, which covers the sense of large bowel resection. Bowel resection may be performed to treat gastrointestinal cancer, bowel ischemia, necrosis, or obstruction due to scar tissue, volvulus, and hernias. Some patients require ileostomy or colostomy after this procedure as alternative means of excretion. Complications of the procedure may include anastomotic leak or dehiscence, hernias, or adhesions causing partial or complete bowel obstruction. Depending on which part and how much of the intestines are removed, there may be digestive and metabolic challenges afterward, such as short bowel syndrome.
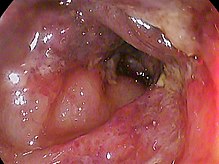
Stercoral ulcer is an ulcer of the colon due to pressure and irritation resulting from severe, prolonged constipation due to a large bowel obstruction, damage to the autonomic nervous system, or stercoral colitis. It is most commonly located in the sigmoid colon and rectum. Prolonged constipation leads to production of fecaliths, leading to possible progression into a fecaloma. These hard lumps irritate the rectum and lead to the formation of these ulcers. It results in fresh bleeding per rectum. These ulcers may be seen on imaging, such as a CT scan but are more commonly identified using endoscopy, usually a colonoscopy. Treatment modalities can include both surgical and non-surgical techniques.

Bowel infarction or gangrenous bowel represents an irreversible injury to the intestine resulting from insufficient blood flow. It is considered a medical emergency because it can quickly result in life-threatening infection and death. Any cause of bowel ischemia, the earlier reversible form of injury, may ultimately lead to infarction if uncorrected. The causes of bowel ischemia or infarction include primary vascular causes and other causes of bowel obstruction.

Intestinal ischemia is a medical condition in which injury to the large or small intestine occurs due to not enough blood supply. It can come on suddenly, known as acute intestinal ischemia, or gradually, known as chronic intestinal ischemia. The acute form of the disease often presents with sudden severe abdominal pain and is associated with a high risk of death. The chronic form typically presents more gradually with abdominal pain after eating, unintentional weight loss, vomiting, and fear of eating.
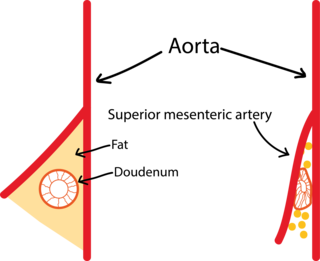
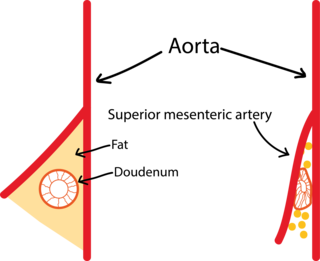
Superior mesenteric artery (SMA) syndrome is a gastro-vascular disorder in which the third and final portion of the duodenum is compressed between the abdominal aorta (AA) and the overlying superior mesenteric artery. This rare, potentially life-threatening syndrome is typically caused by an angle of 6–25° between the AA and the SMA, in comparison to the normal range of 38–56°, due to a lack of retroperitoneal and visceral fat. In addition, the aortomesenteric distance is 2–8 millimeters, as opposed to the typical 10–20. However, a narrow SMA angle alone is not enough to make a diagnosis, because patients with a low BMI, most notably children, have been known to have a narrow SMA angle with no symptoms of SMA syndrome.

Open aortic surgery (OAS), also known as open aortic repair (OAR), describes a technique whereby an abdominal, thoracic or retroperitoneal surgical incision is used to visualize and control the aorta for purposes of treatment, usually by the replacement of the affected segment with a prosthetic graft. OAS is used to treat aneurysms of the abdominal and thoracic aorta, aortic dissection, acute aortic syndrome, and aortic ruptures. Aortobifemoral bypass is also used to treat atherosclerotic disease of the abdominal aorta below the level of the renal arteries. In 2003, OAS was surpassed by endovascular aneurysm repair (EVAR) as the most common technique for repairing abdominal aortic aneurysms in the United States.

Colonic ulcer can occur at any age, in children however they are rare. Most common symptoms are abdominal pain and hematochezia.