Related Research Articles
An HIV vaccine is a potential vaccine that could be either a preventive vaccine or a therapeutic vaccine, which means it would either protect individuals from being infected with HIV or treat HIV-infected individuals.

Vaccine efficacy or vaccine effectiveness is the percentage reduction of disease cases in a vaccinated group of people compared to an unvaccinated group. For example, a vaccine efficacy or effectiveness of 80% indicates an 80% decrease in the number of disease cases among a group of vaccinated people compared to a group in which nobody was vaccinated. When a study is carried out using the most favorable, ideal or perfectly controlled conditions, such as those in a clinical trial, the term vaccine efficacy is used. On the other hand, when a study is carried out to show how well a vaccine works when they are used in a bigger, typical population under less-than-perfectly controlled conditions, the term vaccine effectiveness is used.

The phases of clinical research are the stages in which scientists conduct experiments with a health intervention to obtain sufficient evidence for a process considered effective as a medical treatment. For drug development, the clinical phases start with testing for drug safety in a few human subjects, then expand to many study participants to determine if the treatment is effective. Clinical research is conducted on drug candidates, vaccine candidates, new medical devices, and new diagnostic assays.

Galidesivir is an antiviral drug, an adenosine analog. It was developed by BioCryst Pharmaceuticals with funding from NIAID, originally intended as a treatment for hepatitis C, but subsequently developed as a potential treatment for deadly filovirus infections such as Ebola virus disease and Marburg virus disease, as well as Zika virus. Currently, galidesivir is under phase 1 human trial in Brazil for coronavirus.

The COVID-19 pandemic, also known as the coronavirus pandemic, is a global pandemic of coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The novel virus was first identified in an outbreak in the Chinese city of Wuhan in December 2019. Attempts to contain it there failed, allowing the virus to spread to other areas of Asia and later worldwide in 2020. The World Health Organization (WHO) declared the outbreak a public health emergency of international concern (PHEIC) on 30 January 2020. The WHO ended its PHEIC declaration on 5 May 2023. As of 16 September 2023, the pandemic had caused 770,562,703 cases and 6,957,203 confirmed deaths, ranking it fifth in the deadliest epidemics and pandemics in history.

Coronavirus disease 2019 (COVID-19) is a contagious disease caused by the virus SARS-CoV-2. The first known case was identified in Wuhan, China, in December 2019. The disease quickly spread worldwide, resulting in the COVID-19 pandemic.
Inovio Pharmaceuticals is an American biotechnology company focused on the discovery, development, and commercialization of synthetic DNA products for treating cancers and infectious diseases. In April 2020, Inovio was among some 100 companies, academic centers, or research organizations developing a vaccine candidate for treating people infected with COVID-19, with more than 170 total vaccine candidates in development.
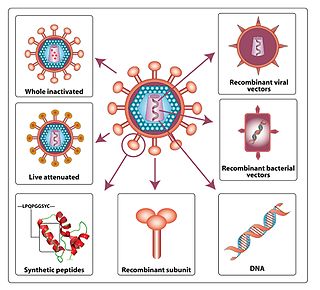
A COVID‑19 vaccine is a vaccine intended to provide acquired immunity against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes coronavirus disease 2019 (COVID‑19).

COVID-19 drug development is the research process to develop preventative therapeutic prescription drugs that would alleviate the severity of coronavirus disease 2019 (COVID-19). From early 2020 through 2021, several hundred drug companies, biotechnology firms, university research groups, and health organizations were developing therapeutic candidates for COVID-19 disease in various stages of preclinical or clinical research, with 419 potential COVID-19 drugs in clinical trials, as of April 2021.
Helen Y. Chu is an American immunologist who is an assistant professor of medicine at the University of Washington. Her research considers maternal immunization, with a focus on influenza and respiratory syncytial virus. During the COVID-19 pandemic, Chu was the first physician to recognise community transmission of the coronavirus disease within the United States.
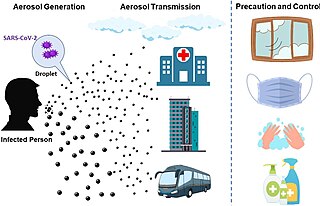
The transmission of COVID-19 is the passing of coronavirus disease 2019 from person to person. COVID-19 is mainly transmitted when people breathe in air contaminated by droplets/aerosols and small airborne particles containing the virus. Infected people exhale those particles as they breathe, talk, cough, sneeze, or sing. Transmission is more likely the closer people are. However, infection can occur over longer distances, particularly indoors.
ChAdOx1 is an adenoviral vector for vaccines that was developed by the Jenner Institute, University of Oxford. The vector is a chimpanzee adenovirus modified to avoid its replication.

ZF2001, trade-named Zifivax or ZF-UZ-VAC-2001, is an adjuvanted protein subunit COVID-19 vaccine developed by Anhui Zhifei Longcom in collaboration with the Institute of Microbiology at the Chinese Academy of Sciences. The vaccine candidate is in Phase III trials with 29,000 participants in China, Ecuador, Malaysia, Pakistan, and Uzbekistan.

SARS-CoV-2, the virus that causes COVID-19, was isolated in late 2019. Its genetic sequence was published on 11 January 2020, triggering the urgent international response to prepare for an outbreak and hasten development of a preventive COVID-19 vaccine. Since 2020, vaccine development has been expedited via unprecedented collaboration in the multinational pharmaceutical industry and between governments. By June 2020, tens of billions of dollars were invested by corporations, governments, international health organizations, and university research groups to develop dozens of vaccine candidates and prepare for global vaccination programs to immunize against COVID‑19 infection. According to the Coalition for Epidemic Preparedness Innovations (CEPI), the geographic distribution of COVID‑19 vaccine development shows North American entities to have about 40% of the activity, compared to 30% in Asia and Australia, 26% in Europe, and a few projects in South America and Africa.

EpiVacCorona is a peptide-based vaccine against COVID-19 developed by the Russian VECTOR Center of Virology. The lack of protective effectiveness of EpiVacCorona, which is still in use in Russia, has been reported in scientific literature and in the media. The vaccine consists of three chemically synthesized peptides that are conjugated to a large carrier protein. This protein is a fusion product of a viral nucleocapsid protein and a bacterial MBP protein. A phase III clinical trial to show whether or not the vaccine can protect people against COVID-19 was launched in November 2020 with more than three thousand participants. The conclusions and results of the trial have not been made public.

ZyCoV-D is a DNA plasmid-based COVID-19 vaccine developed by Indian pharmaceutical company Cadila Healthcare, with support from the Biotechnology Industry Research Assistance Council. It is approved for emergency use in India.

The Sanofi–GSK COVID-19 vaccine sold under the brand name VidPrevtyn Beta, is a COVID-19 vaccine developed by Sanofi Pasteur and GSK.

A viral vector vaccine is a vaccine that uses a viral vector to deliver genetic material (DNA) that can be transcribed by the recipient's host cells as mRNA coding for a desired protein, or antigen, to elicit an immune response. As of April 2021, six viral vector vaccines, four COVID-19 vaccines and two Ebola vaccines, have been authorized for use in humans.

AWcorna, originally termed ARCoV and also known as the Walvax COVID-19 vaccine, is an mRNA COVID-19 vaccine developed by Walvax Biotechnology, Suzhou Abogen Biosciences, and the PLA Academy of Military Science. In contrast to other mRNA COVID vaccines, such as those by Pfizer-BioNtech and Moderna, this vaccine primarily targets the Sars-CoV-2 receptor-binding domain of the spike protein, rather than the entire spike protein. It is approved for Phase III trials in China, Mexico, Indonesia, and Nepal.

COVID-19 vaccine clinical research uses clinical research to establish the characteristics of COVID-19 vaccines. These characteristics include efficacy, effectiveness and safety. As of November 2022, 40 vaccines are authorized by at least one national regulatory authority for public use:
References
- 1 2 Lambkin-Williams, Rob; Noulin, Nicolas; Mann, Alex; Catchpole, Andrew; Gilbert, Anthony S. (22 June 2018). "The human viral challenge model: accelerating the evaluation of respiratory antivirals, vaccines and novel diagnostics". Respiratory Research. 19 (1): 123. doi: 10.1186/s12931-018-0784-1 . ISSN 1465-993X. PMC 6013893 . PMID 29929556.
- 1 2 3 4 5 6 7 8 9 10 Eyal N, Lipsitch M, Smith PG (31 March 2020). "Human challenge studies to accelerate coronavirus vaccine licensure". The Journal of Infectious Diseases. 221 (11): 1752–1756. doi:10.1093/infdis/jiaa152. PMC 7184325 . PMID 32232474.
- 1 2 3 4 5 6 7 8 9 10 Callaway E (April 2020). "Should scientists infect healthy people with the coronavirus to test vaccines?". Nature. 580 (7801): 17. Bibcode:2020Natur.580...17C. doi:10.1038/d41586-020-00927-3. PMID 32218549. S2CID 256820005.
- 1 2 Adams-Phipps, Jupiter; Toomey, Danny; Więcek, Witold; Schmit, Virginia; Wilkinson, James; Scholl, Keller; Jamrozik, Joshua; Roestenberg, Meta; Manheim, David (11 October 2022). "A Systematic Review of Human Challenge Trials, Designs, and Safety". Clinical Infectious Diseases. 76 (4): 609–619. doi: 10.1093/cid/ciac820 . PMC 9938741 . PMID 36219704.
- ↑ Cohen, Jon (18 May 2016). "Studies that intentionally infect people with disease-causing bugs are on the rise". Science. 352 (6288): 882–885. doi:10.1126/science.aaf5726.
- 1 2 3 4 "Key criteria for the ethical acceptability of COVID-19 human challenge studies" (PDF). World Health Organization. 6 May 2020. Retrieved 18 May 2020.
- 1 2 3 4 Cohen, Jon (31 March 2020). "Speed coronavirus vaccine testing by deliberately infecting volunteers? Not so fast, some scientists warn". Science. doi:10.1126/science.abc0006. S2CID 216451224 . Retrieved 19 April 2020.
- ↑ "World's first coronavirus Human Challenge study receives ethics approval in the UK". GOV.UK. Retrieved 18 February 2021.
- 1 2 Wade Hemsworth (13 May 2020). "McMaster researcher contributes to WHO guidelines for COVID-19 vaccine testing". McMaster University Medical School, Hamilton, Canada. Retrieved 25 May 2020.
- ↑ Eric Boodman (13 March 2020). "Coronavirus vaccine clinical trial starting without usual animal data". STAT. Retrieved 19 April 2020.
- ↑ Metzger, W. G.; Ehni, H.-J.; Kremsner, P. G.; Mordmüller, B. G. (2019). "Experimental infections in humans—historical and ethical reflections". Tropical Medicine & International Health. 24 (12): 1384–1390. doi: 10.1111/tmi.13320 . ISSN 1365-3156. PMID 31654450.
- ↑ Gordon, SB; Rylance, J; Luck, A; Jambo, K; Ferreira, DM; Manda-Taylor, L; Bejon, P; Ngwira, B; Littler, K; Seager, Z; Gibani, M; Gmeiner, M; Roestenberg, M; Mlombe, Y; Wellcome Trust CHIM workshop, participants. (2017). "A framework for Controlled Human Infection Model (CHIM) studies in Malawi: Report of a Wellcome Trust workshop on CHIM in Low Income Countries held in Blantyre, Malawi". Wellcome Open Research. 2: 70. doi: 10.12688/wellcomeopenres.12256.1 . PMC 5627502 . PMID 29018841.
- 1 2 Binik, Ariella (May 2020). "What risks should be permissible in controlled human infection model studies?". Bioethics. 34 (4): 420–430. doi:10.1111/bioe.12736. PMID 32115747. S2CID 211727412.
- ↑ D, Sinclair; K, Abba; K, Zaman; F, Qadri; PM, Graves (16 March 2011). "Oral vaccines for preventing cholera". The Cochrane Database of Systematic Reviews. 2011 (3): CD008603. doi:10.1002/14651858.CD008603.pub2. PMC 6532691 . PMID 21412922.
- ↑ Waddington, Claire S.; Darton, Thomas C.; Woodward, William E.; Angus, Brian; Levine, Myron M.; Pollard, Andrew J. (1 May 2014). "Advancing the management and control of typhoid fever: A review of the historical role of human challenge studies". Journal of Infection. 68 (5): 405–418. doi:10.1016/j.jinf.2014.01.006. ISSN 0163-4453. PMID 24491597.
- 1 2 3 4 5 J, Tuju; G, Kamuyu; Lm, Murungi; Fha, Osier (1 October 2017). "Vaccine candidate discovery for the next generation of malaria vaccines". Immunology. 152 (2): 195–206. doi:10.1111/imm.12780. PMC 5588761 . PMID 28646586.
- ↑ Osowicki, Joshua; Azzopardi, Kristy I.; McIntyre, Liam; Rivera-Hernandez, Tania; Ong, Cheryl-lynn Y.; Baker, Ciara; Gillen, Christine M.; Walker, Mark J.; Smeesters, Pierre R.; Davies, Mark R.; Steer, Andrew C. (13 February 2019). "A Controlled Human Infection Model of Group A Streptococcus Pharyngitis: Which Strain and Why?". mSphere. 4 (1): e00647–18, /msphere/4/1/mSphere647–18.atom. doi:10.1128/mSphere.00647-18. PMC 6374595 . PMID 30760615.
- ↑ McShane, Helen (15 May 2020). "Controlled Human Infection Models: Is it Really Feasible to Give People Tuberculosis?". American Journal of Respiratory and Critical Care Medicine. 201 (10): 1180–1181. doi:10.1164/rccm.201912-2408ED. PMC 7233336 . PMID 31904993. S2CID 210041310.
- ↑ MacLennan, Calman A; Aguilar, Anastazia Older; Steele, A Duncan (9 December 2019). "Consensus Report on Shigella Controlled Human Infection Model: Introduction and Overview". Clinical Infectious Diseases. 69 (Supplement_8): S577–S579. doi:10.1093/cid/ciz886. PMC 6901124 . PMID 31816066.
- ↑ Merkel, Tod J (11 July 2020). "Toward a Controlled Human Infection Model of Pertussis". Clinical Infectious Diseases. 71 (2): 412–414. doi:10.1093/cid/ciz842. PMC 7353834 . PMID 31552410.
- ↑ Rose, Anuradha; Sekhar, Amrita (July 2019). "Bioethics of establishing a CHIM model for dengue vaccine development". International Journal of Infectious Diseases. 84: S74–S79. doi: 10.1016/j.ijid.2019.01.013 . PMID 30641207.
- 1 2 3 4 Plotkin, Stanley A.; Caplan, Arthur (20 April 2020). "Extraordinary diseases require extraordinary solutions". Vaccine. 38 (24): 3987–8. doi:10.1016/j.vaccine.2020.04.039. PMC 7167540 . PMID 32331807.
- ↑ "UK plan to be first to run human challenge Covid trials". BBC News. 20 October 2020.