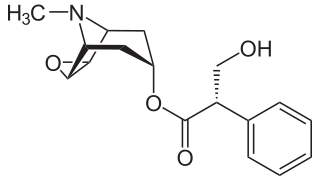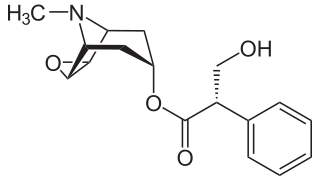
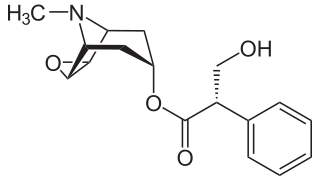
Scopolamine, also known as hyoscine, or Devil's Breath, is a natural or synthetically produced tropane alkaloid and anticholinergic drug that is used as a medication to treat motion sickness and postoperative nausea and vomiting. It is also sometimes used before surgery to decrease saliva. When used by injection, effects begin after about 20 minutes and last for up to 8 hours. It may also be used orally and as a transdermal patch since it has been long known to have transdermal bioavailability.

Atropine is a tropane alkaloid and anticholinergic medication used to treat certain types of nerve agent and pesticide poisonings as well as some types of slow heart rate, and to decrease saliva production during surgery. It is typically given intravenously or by injection into a muscle. Eye drops are also available which are used to treat uveitis and early amblyopia. The intravenous solution usually begins working within a minute and lasts half an hour to an hour. Large doses may be required to treat some poisonings.
An antiemetic is a drug that is effective against vomiting and nausea. Antiemetics are typically used to treat motion sickness and the side effects of opioid analgesics, general anaesthetics, and chemotherapy directed against cancer. They may be used for severe cases of gastroenteritis, especially if the patient is dehydrated.

Haloperidol, sold under the brand name Haldol among others, is a typical antipsychotic medication. Haloperidol is used in the treatment of schizophrenia, tics in Tourette syndrome, mania in bipolar disorder, delirium, agitation, acute psychosis, and hallucinations from alcohol withdrawal. It may be used by mouth or injection into a muscle or a vein. Haloperidol typically works within 30 to 60 minutes. A long-acting formulation may be used as an injection every four weeks by people with schizophrenia or related illnesses, who either forget or refuse to take the medication by mouth.

Hyoscyamine is a naturally occurring tropane alkaloid and plant toxin. It is a secondary metabolite found in certain plants of the family Solanaceae, including henbane, mandrake, angel's trumpets, jimsonweed, the sorcerers' tree, and Atropa belladonna. It is the levorotary isomer of atropine and thus sometimes known as levo-atropine.

Abdominal pain, also known as a stomach ache, is a symptom associated with both non-serious and serious medical issues. Since the abdomen contains most of the body's vital organs, it can be an indicator of a wide variety of diseases. Given that, approaching the examination of a person and planning of a differential diagnosis is extremely important.

Dicycloverine, also known as dicyclomine, sold under the brand name Bentyl among others, is a medication that is used to treat spasms of the intestines such as occur in irritable bowel syndrome. It is taken by mouth or by injection into a muscle. While it has been used in baby colic and enterocolitis, evidence does not support these uses.

Ipratropium bromide, sold under the trade name Atrovent among others, is a type of anticholinergic medication which is applied by different routes: inhaler, nebulizer, or nasal spray, for different reasons.
Hyoscine is a medication used to treat motion sickness and postoperative nausea and vomiting.

Leuprorelin, also known as leuprolide, is a manufactured version of a hormone used to treat prostate cancer, breast cancer, endometriosis, uterine fibroids, as part of transgender hormone therapy, for early puberty, or to perform chemical castration of violent sex offenders. It is given by injection into a muscle or under the skin.

Deliriants are a subclass of hallucinogen. The term was coined in the early 1980s to distinguish these drugs from psychedelics such as LSD and dissociatives such as ketamine, due to their primary effect of causing delirium, as opposed to the more lucid and less disturbed states produced by other types of hallucinogens. The term generally refers to anticholinergic drugs, which are substances that inhibit the function of the neurotransmitter acetylcholine. Common examples of deliriants include plants of the genera Datura and Brugmansia as well as higher than recommended dosages of diphenhydramine (Benadryl). A number of plant deliriants such as that of the Solanaceae family, particularly in the Americas have been used by some indigenous cultures to reach delirious and altered states for traditions or rituals, such as rites of passage, divination or communicating with the ancestors. Despite their long history of use, deliriants are the least-studied class of hallucinogens in terms of their behavioral and neurological effects.
A death rattle is noisy breathing that often occurs in someone who is near death. It is caused by an accumulation of fluids such as saliva and bronchial secretions in the throat and upper airways. Those who are dying may lose their ability to swallow and may have increased production of bronchial secretions, resulting in such an accumulation. Usually, two or three days earlier, symptoms of approaching death can be observed, such as saliva accumulating in the throat, difficulty taking even a spoonful of water, shortness of breath, and rapid chest movement. While death rattle is a strong indication that someone is near death, it can also be produced by other problems that cause interference with the swallowing reflex, such as brain injuries.

Methylscopolamine or methscopolamine, usually provided as the bromide or nitrate salt, is an oral medication used along with other medications to treat peptic ulcers by reducing stomach acid secretion. Proton pump inhibitors and antihistamine medications have made this use obsolete. It can also be used for stomach or intestinal spasms, to reduce salivation, and to treat motion sickness. Methscopolamine is also commonly used as a drying agent, to dry up post-nasal drip, in cold, irritable bowel syndrome and allergy medications
Hypersalivation or hypersialosis is the excessive production of saliva. It has also been defined as increased amount of saliva in the mouth, which may also be caused by decreased clearance of saliva.
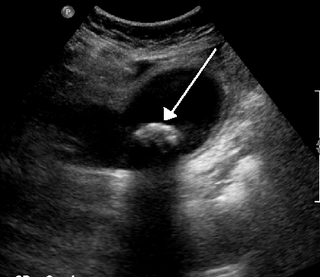
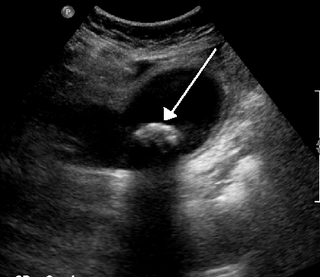
Biliary colic, also known as symptomatic cholelithiasis, a gallbladder attack or gallstone attack, is when a colic occurs due to a gallstone temporarily blocking the cystic duct. Typically, the pain is in the right upper part of the abdomen, and can be severe. Pain usually lasts from 15 minutes to a few hours. Often, it occurs after eating a heavy meal, or during the night. Repeated attacks are common. Cholecystokinin - a gastrointestinal hormone - plays a role in the colic, as following the consumption of fatty meals, the hormone triggers the gallbladder to contract, which may expel stones into the duct and temporarily block it until being successfully passed.
A muscarinic receptor antagonist (MRA), also called an antimuscarinic, is a type of anticholinergic agent that blocks the activity of the muscarinic acetylcholine receptor. The muscarinic receptor is a protein involved in the transmission of signals through certain parts of the nervous system, and muscarinic receptor antagonists work to prevent this transmission from occurring. Notably, muscarinic antagonists reduce the activation of the parasympathetic nervous system. The normal function of the parasympathetic system is often summarised as "rest-and-digest", and includes slowing of the heart, an increased rate of digestion, narrowing of the airways, promotion of urination, and sexual arousal. Muscarinic antagonists counter this parasympathetic "rest-and-digest" response, and also work elsewhere in both the central and peripheral nervous systems.
Pain in cancer may arise from a tumor compressing or infiltrating nearby body parts; from treatments and diagnostic procedures; or from skin, nerve and other changes caused by a hormone imbalance or immune response. Most chronic (long-lasting) pain is caused by the illness and most acute (short-term) pain is caused by treatment or diagnostic procedures. However, radiotherapy, surgery and chemotherapy may produce painful conditions that persist long after treatment has ended.

Cancer and nausea are associated in about fifty percent of people affected by cancer. This may be as a result of the cancer itself, or as an effect of the treatment such as chemotherapy, radiation therapy, or other medication such as opiates used for pain relief. About 70 to 80% of people undergoing chemotherapy experience nausea or vomiting. Nausea and vomiting may also occur in people not receiving treatment, often as a result of the disease involving the gastrointestinal tract, electrolyte imbalance, or as a result of anxiety. Nausea and vomiting may be experienced as the most unpleasant side effects of cytotoxic drugs and may result in patients delaying or refusing further radiotherapy or chemotherapy.
Peripherally selective drugs have their primary mechanism of action outside of the central nervous system (CNS), usually because they are excluded from the CNS by the blood–brain barrier. By being excluded from the CNS, drugs may act on the rest of the body without producing side-effects related to their effects on the brain or spinal cord. For example, most opioids cause sedation when given at a sufficiently high dose, but peripherally selective opioids can act on the rest of the body without entering the brain and are less likely to cause sedation. These peripherally selective opioids can be used as antidiarrheals, for instance loperamide (Imodium).

Cholinergic blocking drugs are a group of drugs that block the action of acetylcholine (ACh), a neurotransmitter, in synapses of the cholinergic nervous system. They block acetylcholine from binding to cholinergic receptors, namely the nicotinic and muscarinic receptors.