Related Research Articles

Immunology is a branch of biology and medicine that covers the study of immune systems in all organisms.

The lymphatic system, or lymphoid system, is an organ system in vertebrates that is part of the immune system, and complementary to the circulatory system. It consists of a large network of lymphatic vessels, lymph nodes, lymphoid organs, lymphoid tissues and lymph. Lymph is a clear fluid carried by the lymphatic vessels back to the heart for re-circulation. The Latin word for lymph, lympha, refers to the deity of fresh water, "Lympha".

Sertoli cells are a type of sustentacular "nurse" cell found in human testes which contribute to the process of spermatogenesis as a structural component of the seminiferous tubules. They are activated by follicle-stimulating hormone (FSH) secreted by the adenohypophysis and express FSH receptor on their membranes.

In immunology, a memory B cell (MBC) is a type of B lymphocyte that forms part of the adaptive immune system. These cells develop within germinal centers of the secondary lymphoid organs. Memory B cells circulate in the blood stream in a quiescent state, sometimes for decades. Their function is to memorize the characteristics of the antigen that activated their parent B cell during initial infection such that if the memory B cell later encounters the same antigen, it triggers an accelerated and robust secondary immune response. Memory B cells have B cell receptors (BCRs) on their cell membrane, identical to the one on their parent cell, that allow them to recognize antigen and mount a specific antibody response.
The regulatory T cells (Tregs or Treg cells), formerly known as suppressor T cells, are a subpopulation of T cells that modulate the immune system, maintain tolerance to self-antigens, and prevent autoimmune disease. Treg cells are immunosuppressive and generally suppress or downregulate induction and proliferation of effector T cells. Treg cells express the biomarkers CD4, FOXP3, and CD25 and are thought to be derived from the same lineage as naïve CD4+ cells. Because effector T cells also express CD4 and CD25, Treg cells are very difficult to effectively discern from effector CD4+, making them difficult to study. Research has found that the cytokine transforming growth factor beta (TGF-β) is essential for Treg cells to differentiate from naïve CD4+ cells and is important in maintaining Treg cell homeostasis.

The blood–testis barrier is a physical barrier between the blood vessels and the seminiferous tubules of the animal testes. The name "blood-testis barrier" is misleading as it is not a blood-organ barrier in a strict sense, but is formed between Sertoli cells of the seminiferous tubule and isolates the further developed stages of germ cells from the blood. A more correct term is the Sertoli cell barrier (SCB).
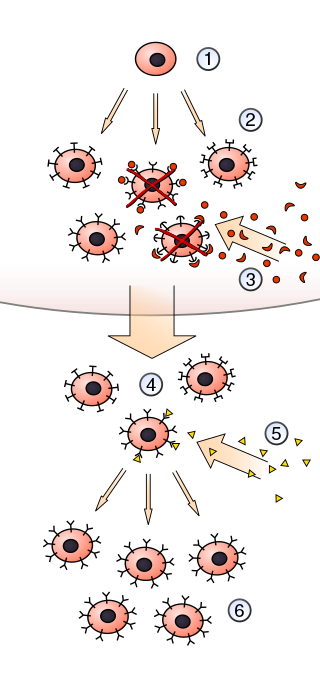
In immunology, clonal selection theory explains the functions of cells of the immune system (lymphocytes) in response to specific antigens invading the body. The concept was introduced by Australian doctor Frank Macfarlane Burnet in 1957, in an attempt to explain the great diversity of antibodies formed during initiation of the immune response. The theory has become the widely accepted model for how the human immune system responds to infection and how certain types of B and T lymphocytes are selected for destruction of specific antigens.
Gut-associated lymphoid tissue (GALT) is a component of the mucosa-associated lymphoid tissue (MALT) which works in the immune system to protect the body from invasion in the gut.
Memory T cells are a subset of T lymphocytes that might have some of the same functions as memory B cells. Their lineage is unclear.
Immune tolerance, or immunological tolerance, or immunotolerance, is a state of unresponsiveness of the immune system to substances or tissues that would otherwise have the capacity to elicit an immune response in a given organism. It is induced by prior exposure to that specific antigen and contrasts with conventional immune-mediated elimination of foreign antigens. Tolerance is classified into central tolerance or peripheral tolerance depending on where the state is originally induced—in the thymus and bone marrow (central) or in other tissues and lymph nodes (peripheral). The mechanisms by which these forms of tolerance are established are distinct, but the resulting effect is similar.
Neural tissue engineering is a specific sub-field of tissue engineering. Neural tissue engineering is primarily a search for strategies to eliminate inflammation and fibrosis upon implantation of foreign substances. Often foreign substances in the form of grafts and scaffolds are implanted to promote nerve regeneration and to repair damage caused to nerves of both the central nervous system (CNS) and peripheral nervous system (PNS) by an injury.
In immunology, peripheral tolerance is the second branch of immunological tolerance, after central tolerance. It takes place in the immune periphery. Its main purpose is to ensure that self-reactive T and B cells which escaped central tolerance do not cause autoimmune disease. Peripheral tolerance prevents immune response to harmless food antigens and allergens, too.

CD69 is a human transmembrane C-Type lectin protein encoded by the CD69 gene. It is an early activation marker that is expressed in hematopoietic stem cells, T cells, and many other cell types in the immune system. It is also implicated in T cell differentiation as well as lymphocyte retention in lymphoid organs.
Testicular Immunology is the study of the immune system within the testis. It includes an investigation of the effects of infection, inflammation and immune factors on testicular function. Two unique characteristics of testicular immunology are evident: (1) the testis is described as an immunologically privileged site, where suppression of immune responses occurs; and, (2) some factors which normally lead to inflammation are present at high levels in the testis, where they regulate the development of sperm instead of promoting inflammation.

Mucosal immunology is the study of immune system responses that occur at mucosal membranes of the intestines, the urogenital tract, and the respiratory system. The mucous membranes are in constant contact with microorganisms, food, and inhaled antigens. In healthy states, the mucosal immune system protects the organism against infectious pathogens and maintains a tolerance towards non-harmful commensal microbes and benign environmental substances. Disruption of this balance between tolerance and deprivation of pathogens can lead to pathological conditions such as food allergies, irritable bowel syndrome, susceptibility to infections, and more.
Chemorepulsion is the directional movement of a cell away from a substance. Of the two directional varieties of chemotaxis, chemoattraction has been studied to a much greater extent. Only recently have the key components of the chemorepulsive pathway been elucidated. The exact mechanism is still being investigated, and its constituents are currently being explored as likely candidates for immunotherapies.
Lymph node stromal cells are essential to the structure and function of the lymph node whose functions include: creating an internal tissue scaffold for the support of hematopoietic cells; the release of small molecule chemical messengers that facilitate interactions between hematopoietic cells; the facilitation of the migration of hematopoietic cells; the presentation of antigens to immune cells at the initiation of the adaptive immune system; and the homeostasis of lymphocyte numbers. Stromal cells originate from multipotent mesenchymal stem cells.
Skin immunity is a property of skin that allows it to resist infections from pathogens. In addition to providing a passive physical barrier against infection, the skin also contains elements of the innate and adaptive immune systems which allows it to actively fight infections. Hence the skin provides defense in depth against infection.
Tolerogenic therapy aims to induce immune tolerance where there is pathological or undesirable activation of the normal immune response. This can occur, for example, when an allogeneic transplantation patient develops an immune reaction to donor antigens, or when the body responds inappropriately to self antigens implicated in autoimmune diseases. It must provide absence of specific antibodies for exactly that antigenes.
Tolerogenic dendritic cells are heterogenous pool of dendritic cells with immuno-suppressive properties, priming immune system into tolerogenic state against various antigens. These tolerogenic effects are mostly mediated through regulation of T cells such as inducing T cell anergy, T cell apoptosis and induction of Tregs. Tol-DCs also affect local micro-environment toward tolerogenic state by producing anti-inflammatory cytokines.
References
- 1 2 Hong S, Van Kaer L (November 1999). "Immune privilege: keeping an eye on natural killer T cells". The Journal of Experimental Medicine. 190 (9): 1197–200. doi:10.1084/jem.190.9.1197. PMC 2195673 . PMID 10544192.
- ↑ Sun Z, Zhang M, Zhao XH, Liu ZH, Gao Y, Samartzis D, Wang HQ, Luo ZJ (2013). "Immune cascades in human intervertebral disc: the pros and cons". International Journal of Clinical and Experimental Medicine . 6 (6): 1009–1014. PMC 3657352 . PMID 23696917.
- ↑ Fujihara Y, Takato T, Hoshi K (2014). "Macrophage-inducing FasL on chondrocytes forms immune privilege in cartilage tissue engineering, enhancing in vivo regeneration". Stem Cells. 32 (2): 1208–1219. doi: 10.1002/stem.1636 . PMID 24446149.
- ↑ Abazari A, Jomha NM, Elliott JA, McGann LE (2013). "Cryopreservation of articular cartilage". Cryobiology . 66 (3): 201–209. doi: 10.1016/j.cryobiol.2013.03.001 . PMID 23499618.
- ↑ Ziv, Y.et al (2006). Nature Neuroscience, Immune cells contribute to the maintenance of neurogenesis and spatial learning abilities in adulthood 9, 268 - 275.
- ↑ Kent A. Why Doesn't a Mother Reject Her Fetus? Rev Obstet Gynecol. 2009 Winter;2(1):67-8. PMID 19399300; PMCID: PMC2672992.
- ↑ Niederkorn, Jerry Y. (2017-01-27). "Corneal Transplantation and Immune Privilege". International Reviews of Immunology. 32 (1): 57–67. doi:10.3109/08830185.2012.737877. ISSN 0883-0185. PMC 3885418 . PMID 23360158.
- ↑ Garrett JC, Steensen RN, Stevensen RN (1991). "Meniscal transplantation in the human knee: a preliminary report". Arthroscopy: The Journal of Arthroscopic and Related Surgery. 7 (1): 57–62. doi:10.1016/0749-8063(91)90079-D. PMID 2009121.
- 1 2 Janeway, C. A.Jr., Travers, P., Walport, M., Shlomchik. M.J. (2005). ImmunoBiology, the immune system in health and disease 6th Edition. Garland Science.
- ↑ "Autoimmunity". webMIC 419: Immunology. University of Arizona. Archived from the original on 2003-06-10.
- ↑ Green DR, Ware CF (June 1997). "Fas-ligand: privilege and peril". Proc Natl Acad Sci USA. 94 (12): 5986–90. Bibcode:1997PNAS...94.5986G. doi: 10.1073/pnas.94.12.5986 . PMC 33671 . PMID 9177153.
- ↑ Keino H, Takeuchi M, Kezuka T, Hattori T, Usui M, Taguchi O, Streilein JW, Stein-Streilein J (March 2006). "Induction of eye-derived tolerance does not depend on naturally occurring CD4+CD25+ T regulatory cells". Investigative Ophthalmology & Visual Science. 47 (3): 1047–55. doi: 10.1167/iovs.05-0110 . PMID 16505040.
- ↑ Streilein JW, Stein-Streilein J (2002). "Anterior chamber associated immune deviation (ACAID): regulation, biological relevance, and implications for therapy". International Reviews of Immunology. 21 (2–3): 123–52. doi:10.1080/08830180212066. PMID 12424840. S2CID 40690072.
- ↑ Lambe T, Leung JC, Ferry H, Bouriez-Jones T, Makinen K, Crockford TL, Jiang HR, Nickerson JM, Peltonen L, Forrester JV, Cornall RJ (2007). "Limited Peripheral T Cell Anergy Predisposes to Retinal Autoimmunity". The Journal of Immunology. 178 (7): 4276–4283. doi: 10.4049/jimmunol.178.7.4276 . PMID 17371984.
- ↑ Zenclussen A.C. (2006). "Regulatory T cells in pregnancy". Springer Seminars in Immunopathology. 28 (1): 31–39. doi:10.1007/s00281-006-0023-6. PMID 16838178. S2CID 40735131.
- ↑ Zenclussen AC, Schumacher A, Zenclussen ML, Wafula P, Volk HD (April 2007). "Immunology of pregnancy: cellular mechanisms allowing fetal survival within the maternal uterus". Expert Reviews in Molecular Medicine. 9 (10): 1–14. doi:10.1017/S1462399407000294. PMID 17462112. S2CID 12507493.
- 1 2 Hedger MP, Hales DB (2006). "Immunophysiology of the Male Reproductive Tract". In Neill JD (ed.). Knobil and Neill's Physiology of Reproduction. Elsevier. pp. 1195–1286. ISBN 978-0-12-515401-7.
- 1 2 3 Fijak M, Meinhardt A (2006). "The testis in immune privilege". Immunological Reviews. 213 (1): 66–81. doi: 10.1111/j.1600-065X.2006.00438.x . PMID 16972897. S2CID 3048709.
- ↑ Kohno S, Munoz JA, Williams TM, Teuscher C, Bernard CC, Tung KS (1983). "Immunopathology of murine experimental allergic orchitis". J. Immunol. 130 (6): 2675–2682. doi: 10.4049/jimmunol.130.6.2675 . PMID 6682874. S2CID 7199215.
- ↑ Teuscher C, Wild GC, Tung KS (1982). "Immunochemical analysis of guinea pig sperm autoantigens". Biol. Reprod. 26 (2): 218–229. doi: 10.1095/biolreprod26.2.218 . PMID 7039703.
- ↑ Kaur, Gurvinder; Thompson, Lea Ann; Dufour, Jannette M. (2014-06-01). "Sertoli cells – Immunological sentinels of spermatogenesis". Seminars in Cell & Developmental Biology. Regulation of Spermatogenesis Part II & DNA Replication. 30: 36–44. doi:10.1016/j.semcdb.2014.02.011. PMC 4043859 . PMID 24603046.
- ↑ Kaur, Gurvinder; Thompson, Lea Ann; Dufour, Jannette M. (2017-01-27). "Sertoli cells- Immunological sentinels of spermatogenesis". Seminars in Cell & Developmental Biology. 30: 36–44. doi:10.1016/j.semcdb.2014.02.011. ISSN 1084-9521. PMC 4043859 . PMID 24603046.
- ↑ Mital, Payal; Hinton, Barry T.; Dufour, Jannette M. (2011-05-01). "The blood-testis and blood-epididymis barriers are more than just their tight junctions". Biology of Reproduction. 84 (5): 851–858. doi:10.1095/biolreprod.110.087452. ISSN 1529-7268. PMC 4574632 . PMID 21209417.
- ↑ Kern S, Robertson SA, Mau VJ, Maddocks S (1995). "Cytokine secretion by macrophages in the rat testis". Biol. Reprod. 53 (6): 1407–1416. doi: 10.1095/biolreprod53.6.1407 . PMID 8562698.
- ↑ O'Bryan MK, Gerdprasert O, Nikolic-Paterson DJ, Meinhardt A, Muir JA, Foulds LM, Phillips DJ, de Kretser DM, Hedger MP (2005). "Cytokine profiles in the testes of rats treated with lipopolysaccharide reveal localized suppression of inflammatory responses". Am J Physiol Regul Integr Comp Physiol. 288 (6): R1744–R1755. doi:10.1152/ajpregu.00651.2004. PMID 15661966. S2CID 15841104.
- 1 2 3 Galea I, Bechmann I, Perry VH (January 2007). "What is immune privilege (not)?". Trends in Immunology. 28 (1): 12–8. doi:10.1016/j.it.2006.11.004. PMID 17129764.
- ↑ Carson MJ, Doose JM, Melchior B, Schmid CD, Ploix CC (October 2006). "CNS immune privilege: hiding in plain sight". Immunol. Rev. 213 (1): 48–65. doi:10.1111/j.1600-065X.2006.00441.x. PMC 2633103 . PMID 16972896.
- ↑ Mendez-Fernandez Y.V.; et al. (2005). "Anatomical and cellular requirements for the activation and migration of virus-specific CD8+ T cells to the brain during Theiler's virus infection". Journal of Virology. 79 (5): 3063–3070. doi:10.1128/jvi.79.5.3063-3070.2005. PMC 548433 . PMID 15709026.
- ↑ Hatterer E, et al. (2006). "How to drain without lymphatics? Dendritic cells migrate from the cerebrospinal fluid to the B-cell follicles of cervical lymph nodes". Blood. 107 (2): 806–812. doi: 10.1182/blood-2005-01-0154 . PMID 16204309.
- ↑ Wenkel H, et al. (2000). "Systemic immune deviation in the CNS does not necessarily depend on the integrity of the blood–brain barrier". Journal of Immunology. 164 (10): 5125–5131. doi: 10.4049/jimmunol.164.10.5125 . PMID 10799870.
- ↑ Niederkorn, Jerry Y. (2013-01-13). "Corneal Transplantation and Immune Privilege". International Reviews of Immunology. 32 (1): 57–67. doi:10.3109/08830185.2012.737877. ISSN 0883-0185. PMC 3885418 . PMID 23360158.
- ↑ Taylor, Andrew W. (2016-01-01). "Ocular Immune Privilege and Transplantation". Frontiers in Immunology. 7: 37. doi: 10.3389/fimmu.2016.00037 . PMC 4744940 . PMID 26904026.
- ↑ Kaur, Gurvinder; Thompson, Lea Ann; Pasham, Mithun; Tessanne, Kim; Long, Charles R.; Dufour, Jannette M. (2017-01-04). "Sustained Expression of Insulin by a Genetically Engineered Sertoli Cell Line after Allotransplantation in Diabetic BALB/c Mice". Biology of Reproduction. 90 (5): 109. doi:10.1095/biolreprod.113.115600. ISSN 0006-3363. PMC 4076370 . PMID 24695630.
- ↑ Li, Yang; Xue, Wujun; Liu, Hongbao; Fan, Ping; Wang, Xiaohong; Ding, Xiaoming; Tian, Xiaohui; Feng, Xinshun; Pan, Xiaoming (2013-02-20). "Combined Strategy of Endothelial Cells Coating, Sertoli Cells Coculture and Infusion Improves Vascularization and Rejection Protection of Islet Graft". PLOS ONE. 8 (2): e56696. Bibcode:2013PLoSO...856696L. doi: 10.1371/journal.pone.0056696 . ISSN 1932-6203. PMC 3577699 . PMID 23437215.
- ↑ Luca, Giovanni; Arato, Iva; Mancuso, Francesca; Calvitti, Mario; Falabella, Giulia; Murdolo, Giuseppe; Basta, Giuseppe; Cameron, Don F.; Hansen, Barbara C. (2016-11-01). "Xenograft of microencapsulated Sertoli cells restores glucose homeostasis in db/db mice with spontaneous diabetes mellitus". Xenotransplantation. 23 (6): 429–439. doi:10.1111/xen.12274. ISSN 1399-3089. PMID 27678013. S2CID 46744082.
- ↑ Medawar, P. B. (2017-01-04). "Immunity to Homologous Grafted Skin. III. The Fate of Skin Homographs Transplanted to the Brain, to Subcutaneous Tissue, and to the Anterior Chamber of the Eye". British Journal of Experimental Pathology. 29 (1): 58–69. ISSN 0007-1021. PMC 2073079 . PMID 18865105.