Related Research Articles

A retrovirus is a type of virus that inserts a DNA copy of its RNA genome into the DNA of a host cell that it invades, thus changing the genome of that cell. After invading a host cell's cytoplasm, the virus uses its own reverse transcriptase enzyme to produce DNA from its RNA genome, the reverse of the usual pattern, thus retro (backwards). The new DNA is then incorporated into the host cell genome by an integrase enzyme, at which point the retroviral DNA is referred to as a provirus. The host cell then treats the viral DNA as part of its own genome, transcribing and translating the viral genes along with the cell's own genes, producing the proteins required to assemble new copies of the virus. Many retroviruses cause serious diseases in humans, other mammals, and birds.

Antiviral drugs are a class of medication used for treating viral infections. Most antivirals target specific viruses, while a broad-spectrum antiviral is effective against a wide range of viruses. Antiviral drugs are one class of antimicrobials, a larger group which also includes antibiotic, antifungal and antiparasitic drugs, or antiviral drugs based on monoclonal antibodies. Most antivirals are considered relatively harmless to the host, and therefore can be used to treat infections. They should be distinguished from virucides, which are not medication but deactivate or destroy virus particles, either inside or outside the body. Natural virucides are produced by some plants such as eucalyptus and Australian tea trees.
The management of HIV/AIDS normally includes the use of multiple antiretroviral drugs as a strategy to control HIV infection. There are several classes of antiretroviral agents that act on different stages of the HIV life-cycle. The use of multiple drugs that act on different viral targets is known as highly active antiretroviral therapy (HAART). HAART decreases the patient's total burden of HIV, maintains function of the immune system, and prevents opportunistic infections that often lead to death. HAART also prevents the transmission of HIV between serodiscordant same-sex and opposite-sex partners so long as the HIV-positive partner maintains an undetectable viral load.
Protease inhibitors (PIs) are medications that act by interfering with enzymes that cleave proteins. Some of the most well known are antiviral drugs widely used to treat HIV/AIDS, hepatitis C and COVID-19. These protease inhibitors prevent viral replication by selectively binding to viral proteases and blocking proteolytic cleavage of protein precursors that are necessary for the production of infectious viral particles.

Ritonavir, sold under the brand name Norvir, is an antiretroviral medication used along with other medications to treat HIV/AIDS. This combination treatment is known as highly active antiretroviral therapy (HAART). Ritonavir is a protease inhibitor and is used with other protease inhibitors. It may also be used in combination with other medications to treat hepatitis C and COVID-19. It is taken by mouth. Tablets of ritonavir are not bioequivalent to capsules, as the tablets may result in higher peak plasma concentrations.

Zinc finger inhibitors, or zinc ejectors, are substances or compounds that interact adversely with zinc fingers and cause them to release their zinc from its binding site, disrupting the conformation of the polypeptide chain and rendering the zinc fingers ineffective, thereby preventing them from performing their associated cellular functions. This is typically accomplished through chelation of the zinc binding site. As zinc fingers are known to be involved in m-RNA regulation, reverse transcription, protection of synthesized viral DNA, transcription inhibition, and initial integration processes, prevention of zinc finger function can have drastic effects on the function of the cell or virus.
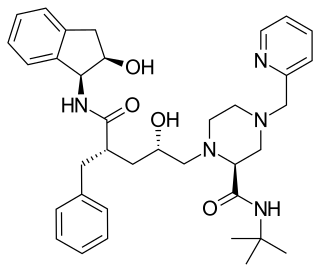
Nelfinavir, sold under the brand name Viracept, is an antiretroviral medication used in the treatment of HIV/AIDS. Nelfinavir belongs to the class of drugs known as protease inhibitors (PIs) and like other PIs is almost always used in combination with other antiretroviral drugs.
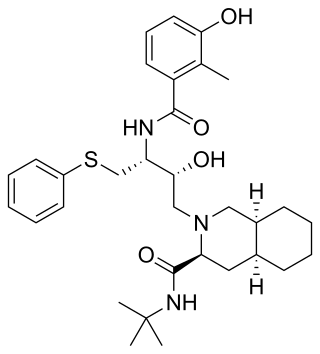
Indinavir is a protease inhibitor used as a component of highly active antiretroviral therapy to treat HIV/AIDS. It is soluble white powder administered orally in combination with other antiviral drugs. The drug prevents protease from functioning normally. Consequently, HIV viruses cannot reproduce, causing a decrease in the viral load. Commercially sold indinavir is indinavir anhydrous, which is indinavir with an additional amine in the hydroxyethylene backbone. This enhances its solubility and oral bioavailability, making it easier for users to intake. It was synthetically produced for the purpose of inhibiting the protease in the HIV virus.
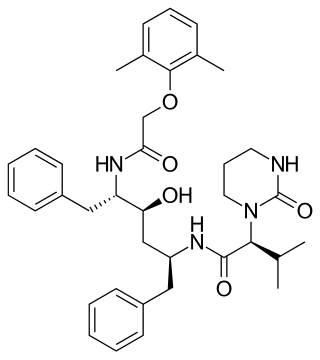
Lopinavir is an antiretroviral of the protease inhibitor class. It is used against HIV infections as a fixed-dose combination with another protease inhibitor, ritonavir (lopinavir/ritonavir).
Entry inhibitors, also known as fusion inhibitors, are a class of antiviral drugs that prevent a virus from entering a cell, for example, by blocking a receptor. Entry inhibitors are used to treat conditions such as HIV and hepatitis D.

A resistance mutation is a mutation in a virus gene that allows the virus to become resistant to treatment with a particular antiviral drug. The term was first used in the management of HIV, the first virus in which genome sequencing was routinely used to look for drug resistance. At the time of infection, a virus will infect and begin to replicate within a preliminary cell. As subsequent cells are infected, random mutations will occur in the viral genome. When these mutations begin to accumulate, antiviral methods will kill the wild type strain, but will not be able to kill one or many mutated forms of the original virus. At this point a resistance mutation has occurred because the new strain of virus is now resistant to the antiviral treatment that would have killed the original virus. Resistance mutations are evident and widely studied in HIV due to its high rate of mutation and prevalence in the general population. Resistance mutation is now studied in bacteriology and parasitology.

HIV ribosomal frameshift signal is a ribosomal frameshift (PRF) that human immunodeficiency virus (HIV) uses to translate several different proteins from the same sequence.
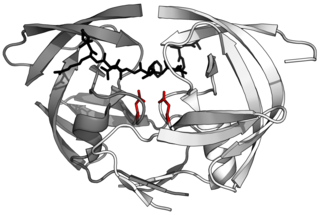
HIV-1 protease (PR) is a retroviral aspartyl protease (retropepsin), an enzyme involved with peptide bond hydrolysis in retroviruses, that is essential for the life-cycle of HIV, the retrovirus that causes AIDS. HIV protease cleaves newly synthesized polyproteins at nine cleavage sites to create the mature protein components of an HIV virion, the infectious form of a virus outside of the host cell. Without effective HIV protease, HIV virions remain uninfectious.

Bevirimat is an anti-HIV drug derived from a betulinic acid-like compound, first isolated from Syzygium claviflorum, a Chinese herb. It is believed to inhibit HIV by a novel mechanism, so-called maturation inhibition. It is not currently U.S. Food and Drug Administration (FDA) approved. It was originally developed by the pharmaceutical company Panacos and reached Phase IIb clinical trials. Myriad Genetics announced on January 21, 2009 the acquisition of all rights to bevirimat for $7M USD. On June 8, 2010 Myriad Genetics announced that it was halting the development of maturation inhibitors, including bevirimat, to focus more on their oncology portfolio.
Many major physiological processes depend on regulation of proteolytic enzyme activity and there can be dramatic consequences when equilibrium between an enzyme and its substrates is disturbed. In this prospective, the discovery of small-molecule ligands, like protease inhibitors, that can modulate catalytic activities has an enormous therapeutic effect. Hence, inhibition of the HIV protease is one of the most important approaches for the therapeutic intervention in HIV infection and their development is regarded as major success of structure-based drug design. They are highly effective against HIV and have, since the 1990s, been a key component of anti-retroviral therapies for HIV/AIDS.
The ChemDB HIV, Opportunistic Infection and Tuberculosis Therapeutics Database is a publicly available tool developed by the National Institute of Allergy and Infectious Diseases to compile preclinical data on small molecules with potential therapeutic action against HIV/AIDS and related opportunistic infections.

Simeprevir, sold under the brand name Olysio among others, is a medication used in combination with other medications for the treatment of hepatitis C. It is specifically used for hepatitis C genotype 1 and 4. Medications it is used with include sofosbuvir or ribavirin and peginterferon-alfa. Cure rates are in 80s to 90s percent. It may be used in those who also have HIV/AIDS. It is taken by mouth once daily for typically 12 weeks.

BMS-955176 is an experimental second generation HIV maturation inhibitor under development by Bristol-Myers Squibb for use in the treatment of HIV infection. By blocking the maturation of the virus, it prevents viral reproduction in host CD4+ T cells. First generation maturation inhibitors such as bevirimat were ineffective against some naturally occurring changes (polymorphisms) in the Gag protease polyprotein; BMS-955176 has been selected to better tolerate gag polymorphisms.
Broad-spectrum antivirals (BSAs) are a class of molecules or compounds, which inhibit the replication of a broad range of viruses. BSAs could be divided into experimental and investigational agents, and approved drugs. BSAs work by inhibiting viral proteins or by targeting host cell factors and processes exploited by different viruses during infection. As of 2021, there are 150 known BSAs in varying stages of development, effective against 78 human viruses. BSAs are potential candidates for treatment of emerging and re-emerging viruses, such as ebola, marburg, and SARS-CoV-2. Many BSAs show antiviral activity against other viruses than originally investigated. Efforts in drug repurposing for SARS-CoV-2 is currently underway. A database of BSAs and viruses they inhibit could be found here.
In the management of HIV/AIDS, HIV capsid inhibitors are antiretroviral medicines that target the capsid shell of the virus. Most current antiretroviral drugs used to treat HIV do not directly target the viral capsid. These have also been termed "Capsid-targeting Antivirals", "Capsid Effectors", and "Capsid Assembly Modulators (CAMs)". Because of this, drugs that specifically inhibit the HIV capsid are being developed in order to reduce the replication of HIV, and treat infections that have become resistant to current antiretroviral therapies.
References
- ↑ Salzwedel K, Martin DE, Sakalian M (2007). "Maturation inhibitors: a new therapeutic class targets the virus structure". AIDS Rev. 9 (3): 162–72. PMID 17982941. Archived from the original on 2016-08-03. Retrieved 2009-02-21.
- ↑ Adamson CS, Salzwedel K, Freed EO (August 2009). "Virus maturation as a new HIV-1 therapeutic target". Expert Opin. Ther. Targets. 13 (8): 895–908. doi:10.1517/14728220903039714. PMC 2737327 . PMID 19534569.
- ↑ Waheed AA, Freed EO (January 2012). "HIV type 1 gag as a target for antiviral therapy". AIDS Res. Hum. Retroviruses. 28 (1): 54–75. doi:10.1089/AID.2011.0230. PMC 3251841 . PMID 21848364.
- ↑ Jiang Y, Liu X, de Clercq E (2011). "New therapeutic approaches targeted at the late stages of the HIV-1 replication cycle". Curr. Med. Chem. 18 (1): 16–28. doi:10.2174/092986711793979751. PMID 21110817.
- ↑ Stoddart CA, Joshi P, Sloan B, Bare JC, Smith PC, Allaway GP, Wild CT, Martin DE (2007). "Potent activity of the HIV-1 maturation inhibitor bevirimat in SCID-hu Thy/Liv mice". PLOS ONE. 2 (11): e1251. Bibcode:2007PLoSO...2.1251S. doi: 10.1371/journal.pone.0001251 . PMC 2080775 . PMID 18043758.

- ↑ "New HIV maturation inhibitor MPC-9055". National AIDS Treatment Advocacy Project. 17 September 2008. Retrieved 10 June 2012.
- ↑ "Myriad Genetics suspends its HIV Maturation Inhibitor Program". AIDSmeds. 8 June 2012. Archived from the original on 8 September 2015. Retrieved 27 June 2012.