Dichlorodiphenyltrichloroethane, commonly known as DDT, is a colorless, tasteless, and almost odorless crystalline chemical compound, an organochloride. Originally developed as an insecticide, it became infamous for its environmental impacts. DDT was first synthesized in 1874 by the Austrian chemist Othmar Zeidler. DDT's insecticidal action was discovered by the Swiss chemist Paul Hermann Müller in 1939. DDT was used in the second half of World War II to limit the spread of the insect-borne diseases malaria and typhus among civilians and troops. Müller was awarded the Nobel Prize in Physiology or Medicine in 1948 "for his discovery of the high efficiency of DDT as a contact poison against several arthropods". The WHO's anti-malaria campaign of the 1950s and 1960s relied heavily on DDT and the results were promising, though there was a resurgence in developing countries afterwards.

Malaria is a mosquito-borne infectious disease that affects humans and other vertebrates. Human malaria causes symptoms that typically include fever, fatigue, vomiting, and headaches. In severe cases, it can cause jaundice, seizures, coma, or death. Symptoms usually begin 10 to 15 days after being bitten by an infected Anopheles mosquito. If not properly treated, people may have recurrences of the disease months later. In those who have recently survived an infection, reinfection usually causes milder symptoms. This partial resistance disappears over months to years if the person has no continuing exposure to malaria.

Anopheles or Marsh Mosquitoes is a genus of mosquito first described and named by J. W. Meigen in 1818. About 460 species are recognized; while over 100 can transmit human malaria, only 30–40 commonly transmit parasites of the genus Plasmodium, which cause malaria in humans in endemic areas. Anopheles gambiae is one of the best known, because of its predominant role in the transmission of the most dangerous malaria parasite species – Plasmodium falciparum.
Tropical diseases are diseases that are prevalent in or unique to tropical and subtropical regions. The diseases are less prevalent in temperate climates, due in part to the occurrence of a cold season, which controls the insect population by forcing hibernation. However, many were present in northern Europe and northern America in the 17th and 18th centuries before modern understanding of disease causation. The initial impetus for tropical medicine was to protect the health of colonial settlers, notably in India under the British Raj. Insects such as mosquitoes and flies are by far the most common disease carrier, or vector. These insects may carry a parasite, bacterium or virus that is infectious to humans and animals. Most often disease is transmitted by an insect bite, which causes transmission of the infectious agent through subcutaneous blood exchange. Vaccines are not available for most of the diseases listed here, and many do not have cures.

Vector control is any method to limit or eradicate the mammals, birds, insects or other arthropods which transmit disease pathogens. The most frequent type of vector control is mosquito control using a variety of strategies. Several of the "neglected tropical diseases" are spread by such vectors.

Mosquito control manages the population of mosquitoes to reduce their damage to human health, economies, and enjoyment. Mosquito control is a vital public-health practice throughout the world and especially in the tropics because mosquitoes spread many diseases, such as malaria and the Zika virus.

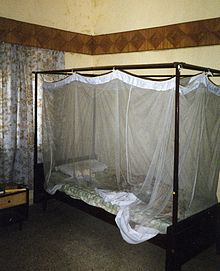
Deltamethrin is a pyrethroid ester insecticide. Deltamethrin plays a key role in controlling malaria vectors, and is used in the manufacture of long-lasting insecticidal mosquito nets; however, resistance of mosquitos and bed bugs to deltamethrin has seen a widespread increase.

The Anopheles gambiae complex consists of at least seven morphologically indistinguishable species of mosquitoes in the genus Anopheles. The complex was recognised in the 1960s and includes the most important vectors of malaria in sub-Saharan Africa, particularly of the most dangerous malaria parasite, Plasmodium falciparum. It is one of the most efficient malaria vectors known. The An. gambiae mosquito additionally transmits Wuchereria bancrofti which causes lymphatic filariasis, a symptom of which is elephantiasis.
Paratransgenesis is a technique that attempts to eliminate a pathogen from vector populations through transgenesis of a symbiont of the vector. The goal of this technique is to control vector-borne diseases. The first step is to identify proteins that prevent the vector species from transmitting the pathogen. The genes coding for these proteins are then introduced into the symbiont, so that they can be expressed in the vector. The final step in the strategy is to introduce these transgenic symbionts into vector populations in the wild. One use of this technique is to prevent mortality for humans from insect-borne diseases. Preventive methods and current controls against vector-borne diseases depend on insecticides, even though some mosquito breeds may be resistant to them. There are other ways to fully eliminate them. “Paratransgenesis focuses on utilizing genetically modified insect symbionts to express molecules within the vector that are deleterious to pathogens they transmit.” The acidic bacteria Asaia symbionts are beneficial in the normal development of mosquito larvae; however, it is unknown what Asais symbionts do to adult mosquitoes.

Indoor residual spraying or IRS is the process of spraying the inside of dwellings with an insecticide to kill mosquitoes that spread malaria. A dilute solution of insecticide is sprayed on the inside walls of certain types of dwellings—those with walls made from porous materials such as mud or wood but not plaster as in city dwellings. Mosquitoes are killed or repelled by the spray, preventing the transmission of the disease. In 2008, 44 countries employed IRS as a malaria control strategy. Several pesticides have historically been used for IRS, the first and most well-known being DDT.

Mosquito-borne diseases or mosquito-borne illnesses are diseases caused by bacteria, viruses or parasites transmitted by mosquitoes. Nearly 700 million people get a mosquito-borne illness each year resulting in over 725,000 deaths.
VectorBase is one of the five Bioinformatics Resource Centers (BRC) funded by the National Institute of Allergy and Infectious Diseases (NIAID), a component of the National Institutes of Health (NIH), which is an agency of the United States Department of Health and Human Services. VectorBase is focused on invertebrate vectors of human pathogens working with the sequencing centers and the research community to curate vector genomes.

Anopheles stephensi is a primary mosquito vector of malaria in urban India and is included in the same subgenus as Anopheles gambiae, the primary malaria vector in Africa. A. gambiae consists of a complex of morphologically identical species of mosquitoes, along with all other major malaria vectors; however, A. stephensi has not yet been included in any of these complexes. Nevertheless, two races of A. stephensi exist based on differences in egg dimensions and the number of ridges on the eggs; A. s. stephensisensu stricto, the type form, is a competent malaria vector that takes place in urban areas, and A. s. mysorensis, the variety form, exists in rural areas and exhibits considerable zoophilic behaviour, making it a poor malaria vector. However, A. s. mysorensis is a detrimental vector in Iran. An intermediate form also exists in rural communities and peri-urban areas, though its vector status is unknown. About 12% of malaria cases in India are due to A. stephensi.
Vestergaard is a company headquartered in Lausanne, Switzerland that manufactures public health tools for people in developing countries. Founded as Vestergaard Frandsen in 1957 as a uniform maker, the company evolved into a social enterprise making products for humanitarian aid in the 1990s. It is now best known for inventing the LifeStraw water filter and the PermaNet mosquito net.

Attractive toxic sugar baits (ATSBs) are oral insecticides designed to reduce malaria infections by killing the host vector – the mosquito – rather than the parasite itself.

Janet Hemingway is a British infectious diseases specialist. She is the former Director of Liverpool School of Tropical Medicine (LSTM) and founding Director of Infection Innovation Consortium and Professor of Tropical Medicine at LSTM. She is current President of the Royal Society of Tropical Medicine and Hygiene.
Thioester containing protein 1, often called TEP1 is a key component of the arthropod innate immune system. TEP1 was first identified as a key immunity gene in 2001 through functional studies on Anopheles gambiae mosquitoes.
Anopheles nili is a species of mosquito in the Culicidae family. It comprises the following elements: An. carnevalei, An. nili, An. ovengensis and An. somalicus. The scientific name of this species was first published in 1904 by Theobald. It is the main mosquito species found in the south Cameroon forest zone which bites humans. It is known as a problematic carrier of malaria, although newly discovered, closely related species in the same genus have also been found to interact with A. nili as a disease vector. In that, they both have similar feeding habits on local targets in the Cameroon region.

Quartan fever is one of the four types of malaria which can be contracted by humans.

Flaminia Catteruccia is an Italian professor of immunology and infectious disease at the Harvard T.H. Chan School of Public Health, studying the interactions between malaria and the Anopheles mosquitoes that transmit the parasites.