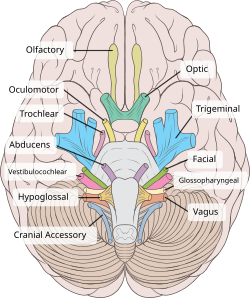
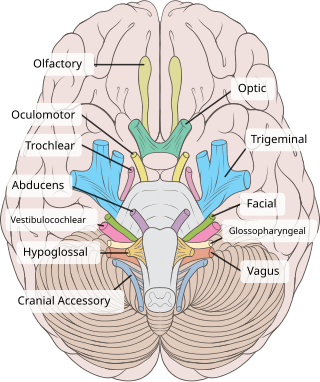
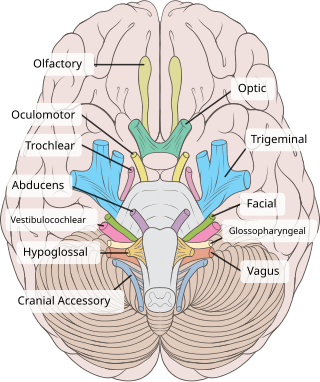
Cranial nerves are the nerves that emerge directly from the brain, of which there are conventionally considered twelve pairs. Cranial nerves relay information between the brain and parts of the body, primarily to and from regions of the head and neck, including the special senses of vision, taste, smell, and hearing.
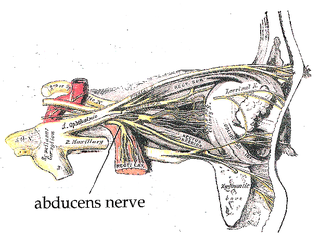
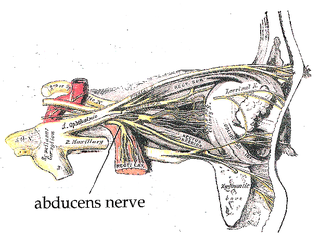
The abducens nerve or abducent nerve, also known as the sixth cranial nerve, cranial nerve VI, or simply CN VI, is a cranial nerve in humans and various other animals that controls the movement of the lateral rectus muscle, one of the extraocular muscles responsible for outward gaze. It is a somatic efferent nerve.
Articles related to anatomy include:
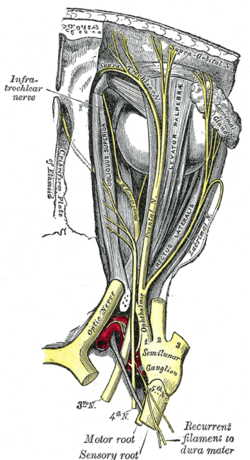
The trochlear nerve, also known as the fourth cranial nerve, cranial nerve IV, or CN IV, is a cranial nerve that innervates a single muscle - the superior oblique muscle of the eye. Unlike most other cranial nerves, the trochlear nerve is exclusively a motor nerve.

The pupillary light reflex (PLR) or photopupillary reflex is a reflex that controls the diameter of the pupil, in response to the intensity (luminance) of light that falls on the retinal ganglion cells of the retina in the back of the eye, thereby assisting in adaptation of vision to various levels of lightness/darkness. A greater intensity of light causes the pupil to constrict, whereas a lower intensity of light causes the pupil to dilate. Thus, the pupillary light reflex regulates the intensity of light entering the eye. Light shone into one eye will cause both pupils to constrict.
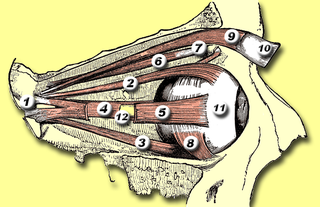
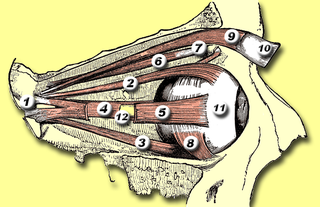
The superior oblique muscle or obliquus oculi superior is a fusiform muscle originating in the upper, medial side of the orbit which abducts, depresses and internally rotates the eye. It is the only extraocular muscle innervated by the trochlear nerve.

The fibers of the oculomotor nerve arise from a nucleus in the midbrain, which lies in the gray substance of the floor of the cerebral aqueduct and extends in front of the aqueduct for a short distance into the floor of the third ventricle. From this nucleus the fibers pass forward through the tegmentum, the red nucleus, and the medial part of the substantia nigra, forming a series of curves with a lateral convexity, and emerge from the oculomotor sulcus on the medial side of the cerebral peduncle.

The accommodation reflex is a reflex action of the eye, in response to focusing on a near object, then looking at a distant object, comprising coordinated changes in vergence, lens shape (accommodation) and pupil size. It is dependent on cranial nerve II, superior centers (interneuron) and cranial nerve III. The change in the shape of the lens is controlled by ciliary muscles inside the eye. Changes in contraction of the ciliary muscles alter the focal distance of the eye, causing nearer or farther images to come into focus on the retina; this process is known as accommodation. The reflex, controlled by the parasympathetic nervous system, involves three responses: pupil constriction, lens accommodation, and convergence.

Eye movement includes the voluntary or involuntary movement of the eyes. Eye movements are used by a number of organisms to fixate, inspect and track visual objects of interests. A special type of eye movement, rapid eye movement, occurs during REM sleep.
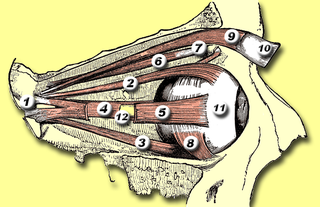
The levator palpebrae superioris is the muscle in the orbit that elevates the upper eyelid.

The lateral rectus muscle is a muscle on the lateral side of the eye in the orbit. It is one of six extraocular muscles that control the movements of the eye. The lateral rectus muscle is responsible for lateral movement of the eyeball, specifically abduction. Abduction describes the movement of the eye away from the midline, allowing the eyeball to move horizontally in the lateral direction, bringing the pupil away from the midline of the body.
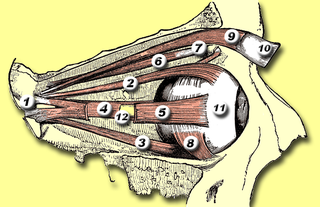
The inferior oblique muscle or obliquus oculi inferior is a thin, narrow muscle placed near the anterior margin of the floor of the orbit. The inferior oblique is one of the extraocular muscles, and is attached to the maxillary bone (origin) and the posterior, inferior, lateral surface of the eye (insertion). The inferior oblique is innervated by the inferior branch of the oculomotor nerve.

The extraocular muscles, or extrinsic ocular muscles, are the seven extrinsic muscles of the eye in humans and other animals. Six of the extraocular muscles, the four recti muscles, and the superior and inferior oblique muscles, control movement of the eye. The other muscle, the levator palpebrae superioris, controls eyelid elevation. The actions of the six muscles responsible for eye movement depend on the position of the eye at the time of muscle contraction.

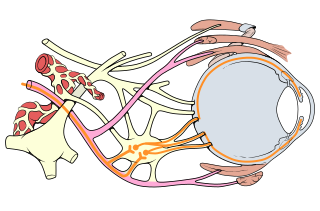
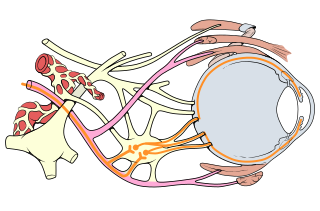
The Edinger–Westphal nucleus is one of two nuclei of the oculomotor nerve and is located in the midbrain. It receives afferents from both pretectal nuclei. It contains parasympathetic pre-ganglionic neuron cell bodies that synapse in the ciliary ganglion. It contributes the autonomic, parasympathetic component to the oculomotor nerve, ultimately providing innervation to the iris sphincter muscle and ciliary muscle to mediate the pupillary light reflex and accommodation, respectively.

The ciliary ganglion is a parasympathetic ganglion located just behind the eye in the posterior orbit. It is 1–2 mm in diameter and in humans contains approximately 2,500 neurons. The ganglion contains postganglionic parasympathetic neurons. These neurons supply the pupillary sphincter muscle, which constricts the pupil, and the ciliary muscle which contracts to make the lens more convex. Both of these muscles are involuntary since they are controlled by the parasympathetic division of the autonomic nervous system.

The short ciliary nerves are nerves of the orbit around the eye. They are branches of the ciliary ganglion. They supply parasympathetic and sympathetic nerve fibers to the ciliary muscle, iris, and cornea. Damage to the short ciliary nerve may result in loss of the pupillary light reflex, or mydriasis.

The cranial nerve exam is a type of neurological examination. It is used to identify problems with the cranial nerves by physical examination. It has nine components. Each test is designed to assess the status of one or more of the twelve cranial nerves (I-XII). These components correspond to testing the sense of smell (I), visual fields and acuity (II), eye movements and pupils, sensory function of face (V), strength of facial (VII) and shoulder girdle muscles (XI), hearing and balance, taste, pharyngeal movement and reflex, tongue movements (XII).
Oculomotor nerve palsy or oculomotor neuropathy is an eye condition resulting from damage to the third cranial nerve or a branch thereof. As the name suggests, the oculomotor nerve supplies the majority of the muscles controlling eye movements. Damage to this nerve will result in an inability to move the eye normally. The nerve also supplies the upper eyelid muscle and is accompanied by parasympathetic fibers innervating the muscles responsible for pupil constriction. The limitations of eye movement resulting from the condition are generally so severe that patients are often unable to maintain normal eye alignment when gazing straight ahead, leading to strabismus and, as a consequence, double vision (diplopia).
In neuroanatomy, corticomesencephalic tract is a descending nerve tract that originates in the frontal eye field and terminate in the midbrain. Its fibers mediate conjugate eye movement.

The ciliary ganglion is a parasympathetic ganglion located just behind the eye in the posterior orbit. Three types of axons enter the ciliary ganglion but only the preganglionic parasympathetic axons synapse there. The entering axons are arranged into three roots of the ciliary ganglion, which join enter the posterior surface of the ganglion.