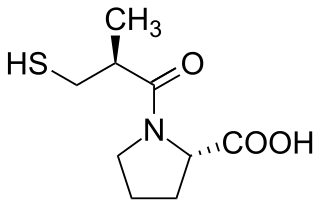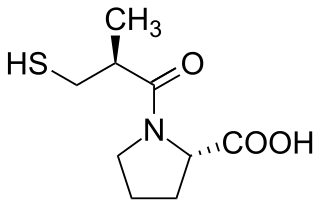
Angiotensin-converting-enzyme inhibitors are a class of medication used primarily for the treatment of high blood pressure and heart failure. This class of medicine works by causing relaxation of blood vessels as well as a decrease in blood volume, which leads to lower blood pressure and decreased oxygen demand from the heart.

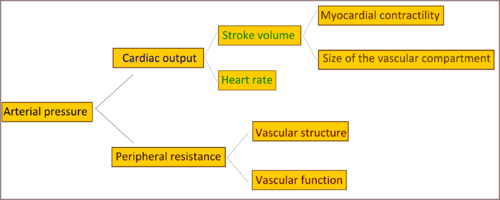
Blood pressure (BP) is the pressure of circulating blood against the walls of blood vessels. Most of this pressure results from the heart pumping blood through the circulatory system. When used without qualification, the term "blood pressure" refers to the pressure in a brachial artery, where it is most commonly measured. Blood pressure is usually expressed in terms of the systolic pressure over diastolic pressure in the cardiac cycle. It is measured in millimeters of mercury (mmHg) above the surrounding atmospheric pressure, or in kilopascals (kPa). The difference between the systolic and diastolic pressures is known as pulse pressure, while the average pressure during a cardiac cycle is known as mean arterial pressure.

Hypertension, also known as high blood pressure, is a long-term medical condition in which the blood pressure in the arteries is persistently elevated. High blood pressure usually does not cause symptoms itself. It is, however, a major risk factor for stroke, coronary artery disease, heart failure, atrial fibrillation, peripheral arterial disease, vision loss, chronic kidney disease, and dementia. Hypertension is a major cause of premature death worldwide.

Renin, also known as an angiotensinogenase, is an aspartic protease protein and enzyme secreted by the kidneys that participates in the body's renin–angiotensin–aldosterone system (RAAS)—also known as the renin–angiotensin–aldosterone axis—that increases the volume of extracellular fluid and causes arterial vasoconstriction. Thus, it increases the body's mean arterial blood pressure.

The renin–angiotensin system (RAS), or renin–angiotensin–aldosterone system (RAAS), is a hormone system that regulates blood pressure, fluid and electrolyte balance, and systemic vascular resistance.

Angiotensin is a peptide hormone that causes vasoconstriction and an increase in blood pressure. It is part of the renin–angiotensin system, which regulates blood pressure. Angiotensin also stimulates the release of aldosterone from the adrenal cortex to promote sodium retention by the kidneys.
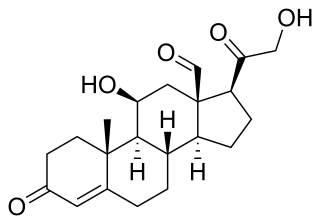
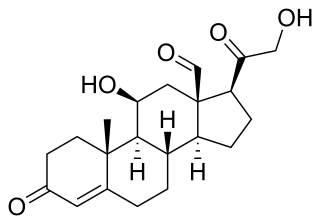
Aldosterone is the main mineralocorticoid steroid hormone produced by the zona glomerulosa of the adrenal cortex in the adrenal gland. It is essential for sodium conservation in the kidney, salivary glands, sweat glands, and colon. It plays a central role in the homeostatic regulation of blood pressure, plasma sodium (Na+), and potassium (K+) levels. It does so primarily by acting on the mineralocorticoid receptors in the distal tubules and collecting ducts of the nephron. It influences the reabsorption of sodium and excretion of potassium (from and into the tubular fluids, respectively) of the kidney, thereby indirectly influencing water retention or loss, blood pressure, and blood volume. When dysregulated, aldosterone is pathogenic and contributes to the development and progression of cardiovascular and kidney disease. Aldosterone has exactly the opposite function of the atrial natriuretic hormone secreted by the heart.

Vasodilation, also known as vasorelaxation, is the widening of blood vessels. It results from relaxation of smooth muscle cells within the vessel walls, in particular in the large veins, large arteries, and smaller arterioles. Blood vessel walls are composed of endothelial tissue and a basal membrane lining the lumen of the vessel, concentric smooth muscle layers on top of endothelial tissue, and an adventitia over the smooth muscle layers. Relaxation of the smooth muscle layer allows the blood vessel to dilate, as it is held in a semi-constricted state by sympathetic nervous system activity. Vasodilation is the opposite of vasoconstriction, which is the narrowing of blood vessels.
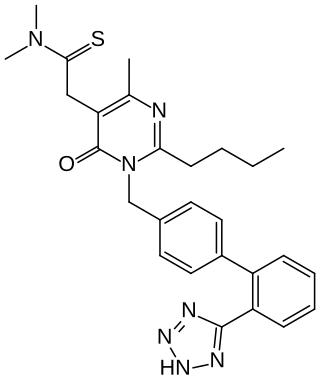
Antihypertensives are a class of drugs that are used to treat hypertension. Antihypertensive therapy seeks to prevent the complications of high blood pressure, such as stroke, heart failure, kidney failure and myocardial infarction. Evidence suggests that reduction of the blood pressure by 5 mmHg can decrease the risk of stroke by 34% and of ischaemic heart disease by 21%, and can reduce the likelihood of dementia, heart failure, and mortality from cardiovascular disease. There are many classes of antihypertensives, which lower blood pressure by different means. Among the most important and most widely used medications are thiazide diuretics, calcium channel blockers, ACE inhibitors, angiotensin II receptor antagonists (ARBs), and beta blockers.
Essential hypertension is a form of hypertension without an identifiable physiologic cause. It is the most common type affecting 85% of those with high blood pressure. The remaining 15% is accounted for by various causes of secondary hypertension. Essential hypertension tends to be familial and is likely to be the consequence of an interaction between environmental and genetic factors. Hypertension can increase the risk of cerebral, cardiac, and renal events.

The baroreflex or baroreceptor reflex is one of the body's homeostatic mechanisms that helps to maintain blood pressure at nearly constant levels. The baroreflex provides a rapid negative feedback loop in which an elevated blood pressure causes the heart rate to decrease. Decreased blood pressure decreases baroreflex activation and causes heart rate to increase and to restore blood pressure levels. Their function is to sense pressure changes by responding to change in the tension of the arterial wall The baroreflex can begin to act in less than the duration of a cardiac cycle and thus baroreflex adjustments are key factors in dealing with postural hypotension, the tendency for blood pressure to decrease on standing due to gravity.

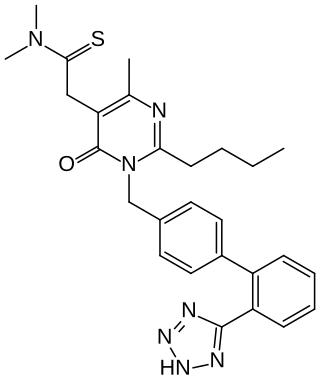
Telmisartan, sold under the brand name Micardis among others, is a medication used to treat high blood pressure, heart failure, and diabetic kidney disease. It is a reasonable initial treatment for high blood pressure. It is taken by mouth. Versions are available as the combination telmisartan/hydrochlorothiazide, telmisartan/cilnidipine and telmisartan/amlodipine.

A hypertensive emergency is very high blood pressure with potentially life-threatening symptoms and signs of acute damage to one or more organ systems. It is different from a hypertensive urgency by this additional evidence for impending irreversible hypertension-mediated organ damage (HMOD). Blood pressure is often above 200/120 mmHg, however there are no universally accepted cutoff values.

Renovascular hypertension is a condition in which high blood pressure is caused by the kidneys' hormonal response to narrowing of the arteries supplying the kidneys. When functioning properly this hormonal axis regulates blood pressure. Due to low local blood flow, the kidneys mistakenly increase blood pressure of the entire circulatory system. It is a form of secondary hypertension - a form of hypertension whose cause is identifiable.

Fenoldopam mesylate (Corlopam) is a drug and synthetic benzazepine derivative which acts as a selective D1 receptor partial agonist. Fenoldopam is used as an antihypertensive agent. It was approved by the Food and Drug Administration (FDA) in September 1997.

Aliskiren is the first in a class of drugs called direct renin inhibitors. It is used for essential (primary) hypertension. While used for high blood pressure, other better studied medications are typically recommended due to concerns of higher side effects and less evidence of benefit.

Salt consumption has been extensively studied for its role in human physiology and impact on human health. Chronic, high intake of dietary salt consumption is associated with hypertension and cardiovascular disease, in addition to other adverse health outcomes. Major health and scientific organizations, such as the World Health Organization, US Centers for Disease Control and Prevention, and American Heart Association, have established high salt consumption as a major risk factor for cardiovascular diseases and stroke.

Orthostatic hypertension is a medical condition consisting of a sudden and abrupt increase in blood pressure (BP) when a person stands up. Orthostatic hypertension is diagnosed by a rise in systolic BP of 20 mmHg or more when standing. Orthostatic diastolic hypertension is a condition in which the diastolic BP raises to 98 mmHg or over in response to standing, but this definition currently lacks clear medical consensus, so is subject to change. Orthostatic hypertension involving the systolic BP is known as systolic orthostatic hypertension.
Fimasartan is a non-peptide angiotensin II receptor antagonist (ARB) used for the treatment of hypertension and heart failure. Through oral administration, fimasartan blocks angiotensin II receptor type 1 (AT1 receptors), reducing pro-hypertensive actions of angiotensin II, such as systemic vasoconstriction and water retention by the kidneys. Concurrent administration of fimasartan with diuretic hydrochlorothiazide has shown to be safe in clinical trials. Fimasartan was approved for use in South Korea on September 9, 2010, and is available under the brand name Kanarb through Boryung Pharmaceuticals, who are presently seeking worldwide partnership.

Hypertension is a condition characterized by an elevated blood pressure in which the long term consequences include cardiovascular disease, kidney disease, adrenal gland tumors, vision impairment, memory loss, metabolic syndrome, stroke and dementia. It affects nearly 1 in 2 Americans and remains as a contributing cause of death in the United States. There are many genetic and environmental factors involved with the development of hypertension including genetics, diet, and stress.