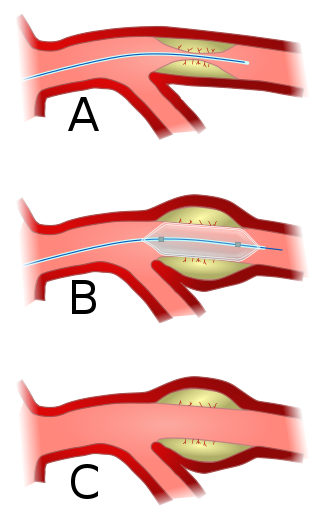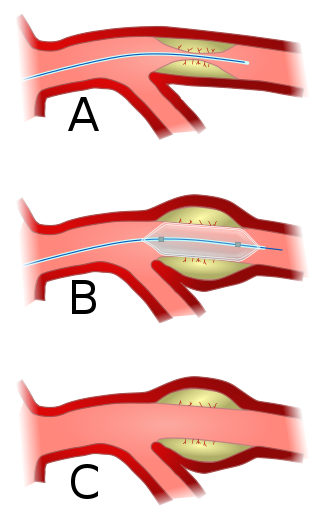
Angioplasty, also known as balloon angioplasty and percutaneous transluminal angioplasty (PTA), is a minimally invasive endovascular procedure used to widen narrowed or obstructed arteries or veins, typically to treat arterial atherosclerosis. A deflated balloon attached to a catheter is passed over a guide-wire into the narrowed vessel and then inflated to a fixed size. The balloon forces expansion of the blood vessel and the surrounding muscular wall, allowing an improved blood flow. A stent may be inserted at the time of ballooning to ensure the vessel remains open, and the balloon is then deflated and withdrawn. Angioplasty has come to include all manner of vascular interventions that are typically performed percutaneously.
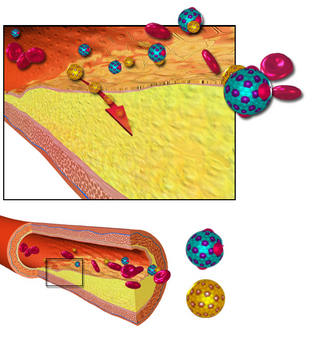
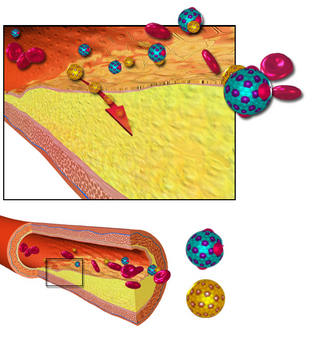
Arteriosclerosis is a vascular disorder characterized by abnormal thickening, hardening, and loss of elasticity of the walls of arteries; this process gradually restricts the blood flow to one's organs and tissues and can lead to severe health risks brought on by atherosclerosis, which is a specific form of arteriosclerosis caused by the buildup of fatty plaques, cholesterol, and some other substances in and on the artery walls.

Interventional radiology (IR) is a medical specialty that performs various minimally-invasive procedures using medical imaging guidance, such as x-ray fluoroscopy, computed tomography, magnetic resonance imaging, or ultrasound. IR performs both diagnostic and therapeutic procedures through very small incisions or body orifices. Diagnostic IR procedures are those intended to help make a diagnosis or guide further medical treatment, and include image-guided biopsy of a tumor or injection of an imaging contrast agent into a hollow structure, such as a blood vessel or a duct. By contrast, therapeutic IR procedures provide direct treatment—they include catheter-based medicine delivery, medical device placement, and angioplasty of narrowed structures.

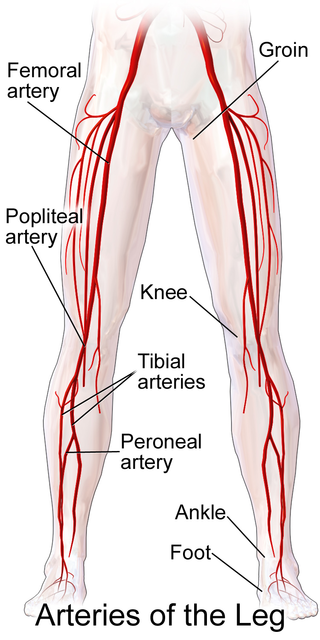
Peripheral artery disease (PAD) is a vascular disorder abnormal narrowing of arteries other than those that supply the heart or brain. PAD can happen in any blood vessel, but it is more common in the legs than the arms.

Ischemia or ischaemia is a restriction in blood supply to any tissue, muscle group, or organ of the body, causing a shortage of oxygen that is needed for cellular metabolism. Ischemia is generally caused by problems with blood vessels, with resultant damage to or dysfunction of tissue i.e. hypoxia and microvascular dysfunction. It also implies local hypoxia in a part of a body resulting from constriction. Ischemia causes not only insufficiency of oxygen, but also reduced availability of nutrients and inadequate removal of metabolic wastes. Ischemia can be partial or total blockage. The inadequate delivery of oxygenated blood to the organs must be resolved either by treating the cause of the inadequate delivery or reducing the oxygen demand of the system that needs it. For example, patients with myocardial ischemia have a decreased blood flow to the heart and are prescribed with medications that reduce chronotrophy and ionotrophy to meet the new level of blood delivery supplied by the stenosed vasculature so that it is adequate.

Stenosis is the abnormal narrowing of a blood vessel or other tubular organ or structure such as foramina and canals. It is also sometimes called a stricture.

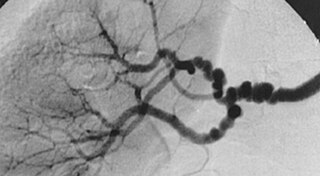
Thromboangiitis obliterans, also known as Buerger disease or Winiwarter-Buerger disease, is a recurring progressive inflammation and thrombosis (clotting) of small and medium arteries and veins of the hands and feet. It is strongly associated with use of tobacco products, primarily from smoking, but is also associated with smokeless tobacco.

In medicine, aortoiliac occlusive disease is a form of central artery disease involving the blockage of the abdominal aorta as it transitions into the common iliac arteries.
Claudication is a medical term usually referring to impairment in walking, or pain, discomfort, numbness, or tiredness in the legs that occurs during walking or standing and is relieved by rest. The perceived level of pain from claudication can be mild to extremely severe. Claudication is most common in the calves but it can also affect the feet, thighs, hips, buttocks, or arms. The word claudication comes from the Latin claudicare meaning 'to limp'.
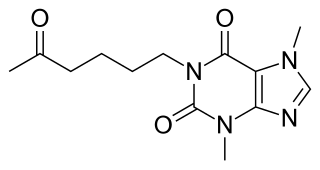
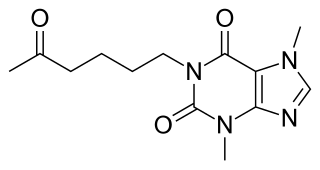
Pentoxifylline, also known as oxpentifylline, is a xanthine derivative used as a drug to treat muscle pain in people with peripheral artery disease. It is generic and sold under many brand names worldwide.
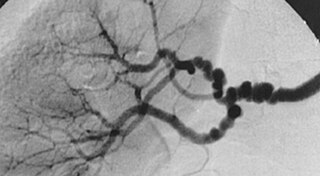
Fibromuscular dysplasia (FMD) is a non-atherosclerotic, non-inflammatory disease of the blood vessels that causes abnormal growth within the wall of an artery. FMD has been found in nearly every arterial bed in the body, although the most commonly affected are the renal and carotid arteries.

Vascular disease is a class of diseases of the vessels of the circulatory system in the body, including blood vessels – the arteries and veins, and the lymphatic vessels. Vascular disease is a subgroup of cardiovascular disease. Disorders in this vast network of blood and lymph vessels can cause a range of health problems that can sometimes become severe, and fatal. Coronary heart disease for example, is the leading cause of death for men and women in the United States.
Abdominal angina is abdominal pain after eating that occurs in individuals with ongoing poor blood supply to their small intestines known as chronic mesenteric ischemia. Although the term angina alone usually denotes angina pectoris, angina by itself can also mean "any spasmodic, choking, or suffocative pain", with an anatomic adjective defining its focus; so, in this case, spasmodic pain in the abdomen. Stedman's Medical Dictionary Online defines abdominal angina as "intermittent abdominal pain, frequently occurring at a fixed time after eating, caused by inadequacy of the mesenteric circulation resulting from arteriosclerosis or other arterial disease. Synonym: intestinal angina."
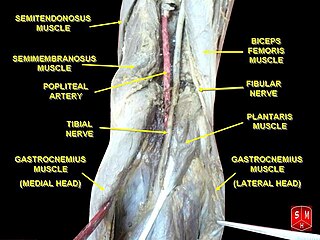
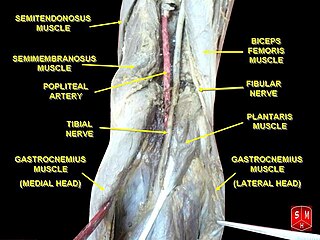
The popliteal artery entrapment syndrome (PAES) is an uncommon pathology that occurs when the popliteal artery is compressed by the surrounding popliteal fossa myofascial structures. This results in claudication and chronic leg ischemia. This condition mainly occurs more in young athletes than in the elderlies. Elderlies, who present with similar symptoms, are more likely to be diagnosed with peripheral artery disease with associated atherosclerosis. Patients with PAES mainly present with intermittent feet and calf pain associated with exercises and relieved with rest. PAES can be diagnosed with a combination of medical history, physical examination, and advanced imaging modalities such as duplex ultrasound, computer tomography, or magnetic resonance angiography. Management can range from non-intervention to open surgical decompression with a generally good prognosis. Complications of untreated PAES can include stenotic artery degeneration, complete popliteal artery occlusion, distal arterial thromboembolism, or even formation of an aneurysm.

Acute limb ischaemia (ALI) occurs when there is a sudden lack of blood flow to a limb, within 14 days of symptoms onset. It is different from another condition which is more chronic called critical limb ischemia (CLD). CLD is the end stage of peripheral vascular disease where there is still some collateral circulation (alternate circulation pathways} that bring some blood to the distal parts of the limbs. While limbs in both acute and chronic limb ischemia may be pulseless, a chronically ischemic limb is typically warm and pink due to a well-developed collateral artery network and does not need emergency intervention to avoid limb loss.
Percutaneous intentional extraluminal revascularization is a percutaneous technique used in interventional radiology for limb salvage in patients with lower limb ischemia due to long superficial femoral artery occlusions. This method is intended for those patients who make poor candidates for infrainguinal arterial bypass surgery. A guide wire is intentionally introduced in the subintimal space, after which balloon dilatation is performed to create a new lumen for the blood to flow through. The technique is not without complications but may serve as a "temporary bypass" to provide wound healing and limb salvage.
Chronic limb threatening ischemia (CLTI), also known as critical limb ischemia (CLI), is an advanced stage of peripheral artery disease (PAD). It is defined as ischemic rest pain, arterial insufficiency ulcers, and gangrene. The latter two conditions are jointly referred to as tissue loss, reflecting the development of surface damage to the limb tissue due to the most severe stage of ischemia. Compared to the other manifestation of PAD, intermittent claudication, CLI has a negative prognosis within a year after the initial diagnosis, with 1-year amputation rates of approximately 12% and mortality of 50% at 5 years and 70% at 10 years.
Blood vessel disorder generally refers to the narrowing, hardening or enlargement of arteries and veins. It is often due to the build-up of fatty deposits in the lumen of blood vessels or infection of the vessel wall. This can occur in various locations such as coronary blood vessels, peripheral arteries and veins. The narrowed arteries would block the blood supply to different organs and tissues. In severe conditions, it may develop into more critical health problems like myocardial infarction, stroke or heart failure, which are some of the major reasons of death.
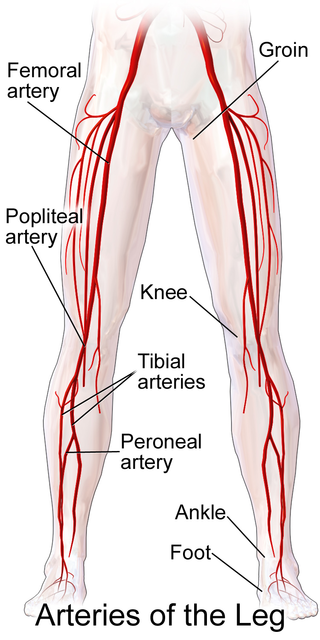
Popliteal bypass surgery, more commonly known as femoropopliteal bypass or more generally as lower extremity bypass surgery, is a surgical procedure used to treat diseased leg arteries above or below the knee. It is used as a medical intervention to salvage limbs that are at risk of amputation and to improve walking ability in people with severe intermittent claudication and ischemic rest pain.

Arterial occlusion is a condition involving partial or complete blockage of blood flow through an artery. Arteries are blood vessels that carry oxygenated blood to body tissues. An occlusion of arteries disrupts oxygen and blood supply to tissues, leading to ischemia. Depending on the extent of ischemia, symptoms of arterial occlusion range from simple soreness and pain that can be relieved with rest, to a lack of sensation or paralysis that could require amputation.