Kocher–Debré–Semelaigne syndrome(KDSS) is hypothyroidism in infancy or childhood characterised by lower extremity or generalized muscular hypertrophy (Herculean appearance), myxoedema, short stature, and cognitive impairment.

Tachycardia, also called tachyarrhythmia, is a heart rate that exceeds the normal resting rate. In general, a resting heart rate over 100 beats per minute is accepted as tachycardia in adults. Heart rates above the resting rate may be normal or abnormal.

Glycogen storage disease type V, also known as McArdle's disease, is a metabolic disorder, one of the metabolic myopathies, more specifically a muscle glycogen storage disease, caused by a deficiency of myophosphorylase. Its incidence is reported as one in 100,000, roughly the same as glycogen storage disease type I.

A glycogen storage disease is a metabolic disorder caused by a deficiency of an enzyme or transport protein affecting glycogen synthesis, glycogen breakdown, or glucose breakdown, typically in muscles and/or liver cells.

Palpitations are perceived abnormalities of the heartbeat characterized by awareness of cardiac muscle contractions in the chest, which is further characterized by the hard, fast and/or irregular beatings of the heart.
Alkalosis is the result of a process reducing hydrogen ion concentration of arterial blood plasma (alkalemia). In contrast to acidemia, alkalemia occurs when the serum pH is higher than normal. Alkalosis is usually divided into the categories of respiratory alkalosis and metabolic alkalosis or a combined respiratory/metabolic alkalosis.

Phosphoglucomutase is an enzyme that transfers a phosphate group on an α-D-glucose monomer from the 1 to the 6 position in the forward direction or the 6 to the 1 position in the reverse direction.
Muscle fatigue is when muscles that were initially generating a normal amount of force, then experience a declining ability to generate force. It can be a result of vigorous exercise, but abnormal fatigue may be caused by barriers to or interference with the different stages of muscle contraction. There are two main causes of muscle fatigue: the limitations of a nerve’s ability to generate a sustained signal ; and the reduced ability of the muscle fiber to contract.

Glycogen phosphorylase is one of the phosphorylase enzymes. Glycogen phosphorylase catalyzes the rate-limiting step in glycogenolysis in animals by releasing glucose-1-phosphate from the terminal alpha-1,4-glycosidic bond. Glycogen phosphorylase is also studied as a model protein regulated by both reversible phosphorylation and allosteric effects.

Exercise intolerance is a condition of inability or decreased ability to perform physical exercise at the normally expected level or duration for people of that age, size, sex, and muscle mass. It also includes experiences of unusually severe post-exercise pain, fatigue, nausea, vomiting or other negative effects. Exercise intolerance is not a disease or syndrome in and of itself, but can result from various disorders.

In endurance sports such as road cycling and long-distance running, hitting the wall or the bonk is a condition of sudden fatigue and loss of energy which is caused by the depletion of glycogen stores in the liver and muscles. Milder instances can be remedied by brief rest and the ingestion of food or drinks containing carbohydrates. Otherwise, it can remedied by attaining second wind by either resting for approximately 10 minutes or by slowing down considerably and increasing speed slowly over a period of 10 minutes. Ten minutes is approximately the time that it takes for free fatty acids to sufficiently produce ATP in response to increased demand.

Inappropriate sinus tachycardia (IST) is defined as sinus tachycardia that is not caused by identifiable medical ailments, a physiological reaction, or pharmaceuticals (a diagnosis of exclusion) and is accompanied by symptoms, frequently invalidating and affecting quality of life. IST symptoms include palpitations, chest discomfort, exhaustion, shortness of breath, presyncope, and syncope.
Ivabradine, sold under the brand name Procoralan among others, is a medication, which is a pacemaker current (If) inhibitor, used for the symptomatic management of heart-related chest pain and heart failure. Patients who qualify for use of Ivabradine for coronary heart failure are patients who have symptomatic heart failure, with reduced ejection volume, and heart rate at least 70 bpm, and the condition not able to be fully managed by beta blockers.

Multifocal atrial tachycardia (MAT) is an abnormal heart rhythm, specifically a type of supraventricular tachycardia, that is particularly common in older people and is associated with exacerbations of chronic obstructive pulmonary disease (COPD). Normally, the heart rate is controlled by a cluster of cells called the sinoatrial node. When a number of different clusters of cells outside the SA node take over control of the heart rate, and the rate exceeds 100 beats per minute, this is called multifocal atrial tachycardia.

Myophosphorylase or glycogen phosphorylase, muscle associated (PYGM) is the muscle isoform of the enzyme glycogen phosphorylase and is encoded by the PYGM gene. This enzyme helps break down glycogen into glucose-1-phosphate, so it can be used within the muscle cell. Mutations in this gene are associated with McArdle disease, a glycogen storage disease of muscle.
Second wind is a phenomenon in endurance sports, such as marathons or road running, whereby an athlete who is out of breath and too tired to continue, finds the strength to press on at top performance with less exertion. The feeling may be similar to that of a "runner's high", the most obvious difference being that the runner's high occurs after the race is over. In muscle glycogenoses, an inborn error of carbohydrate metabolism impairs either the formation or utilization of muscle glycogen. As such, those with muscle glycogenoses do not need to do prolonged exercise to experience "hitting the wall". Instead, signs of exercise intolerance, such as an inappropriate rapid heart rate response to exercise, are experienced from the beginning of an activity, and some muscle GSDs can achieve second wind within about 10 minutes from the beginning of the aerobic activity, such as walking. (See below in pathology).

Inborn errors of carbohydrate metabolism are inborn error of metabolism that affect the catabolism and anabolism of carbohydrates.

Syncope, commonly known as fainting or passing out, is a loss of consciousness and muscle strength characterized by a fast onset, short duration, and spontaneous recovery. It is caused by a decrease in blood flow to the brain, typically from low blood pressure. There are sometimes symptoms before the loss of consciousness such as lightheadedness, sweating, pale skin, blurred vision, nausea, vomiting, or feeling warm. Syncope may also be associated with a short episode of muscle twitching. Psychiatric causes can also be determined when a patient experiences fear, anxiety, or panic; particularly before a stressful event, usually medical in nature. When consciousness and muscle strength are not completely lost, it is called presyncope. It is recommended that presyncope be treated the same as syncope.

Metabolic myopathies are myopathies that result from defects in biochemical metabolism that primarily affect muscle. They are generally genetic defects that interfere with the ability to create energy, causing a low ATP reservoir within the muscle cell.
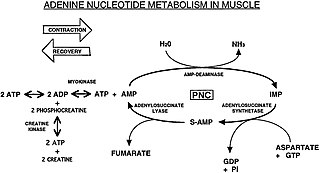
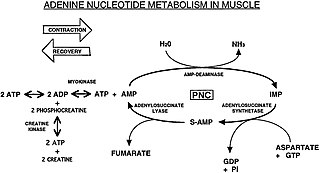
The Purine Nucleotide Cycle is a metabolic pathway in protein metabolism requiring the amino acids aspartate and glutamate. The cycle is used to regulate the levels of adenine nucleotides, in which ammonia and fumarate are generated. AMP converts into IMP and the byproduct ammonia. IMP converts to S-AMP (adenylosuccinate), which then converts to AMP and the byproduct fumarate. The fumarate goes on to produce ATP (energy) via oxidative phosphorylation as it enters the Krebs cycle and then the electron transport chain. Lowenstein first described this pathway and outlined its importance in processes including amino acid catabolism and regulation of flux through glycolysis and the Krebs cycle.