Related Research Articles

Tinea corporis is a fungal infection of the body, similar to other forms of tinea. Specifically, it is a type of dermatophytosis that appears on the arms and legs, especially on glabrous skin; however, it may occur on any superficial part of the body.

Tinea capitis is a cutaneous fungal infection (dermatophytosis) of the scalp. The disease is primarily caused by dermatophytes in the genera Trichophyton and Microsporum that invade the hair shaft. The clinical presentation is typically single or multiple patches of hair loss, sometimes with a 'black dot' pattern, that may be accompanied by inflammation, scaling, pustules, and itching. Uncommon in adults, tinea capitis is predominantly seen in pre-pubertal children, more often boys than girls.

Fungal infection, also known as mycosis, is a disease caused by fungi. Different types are traditionally divided according to the part of the body affected; superficial, subcutaneous, and systemic. Superficial fungal infections include common tinea of the skin, such as tinea of the body, groin, hands, feet and beard, and yeast infections such as pityriasis versicolor. Subcutaneous types include eumycetoma and chromoblastomycosis, which generally affect tissues in and beneath the skin. Systemic fungal infections are more serious and include cryptococcosis, histoplasmosis, pneumocystis pneumonia, aspergillosis and mucormycosis. Signs and symptoms range widely. There is usually a rash with superficial infection. Fungal infection within the skin or under the skin may present with a lump and skin changes. Pneumonia-like symptoms or meningitis may occur with a deeper or systemic infection.

Eumycetoma, also known as Madura foot, is a persistent fungal infection of the skin and the tissues just under the skin, affecting most commonly the feet, although it can occur in hands and other body parts. It starts as a painless wet nodule, which may be present for years before ulceration, swelling, grainy discharge and weeping from sinuses and fistulae, followed by bone deformity.

Chromoblastomycosis is a long-term fungal infection of the skin and subcutaneous tissue.

Dermatophytosis, also known as ringworm, is a fungal infection of the skin (Dermatomycosis). Typically it results in a red, itchy, scaly, circular rash. Hair loss may occur in the area affected. Symptoms begin four to fourteen days after exposure. Multiple areas can be affected at a given time.

Setosphaeria rostrata is a heat tolerant fungus with an asexual reproductive form (anamorph) known as Exserohilum rostratum. This fungus is a common plant pathogen, causing leaf spots as well as crown rot and root rot in grasses. It is also found in soils and on textiles in subtropical and tropical regions. Exserohilum rostratum is one of the 35 Exserohilum species implicated uncommonly as opportunistic pathogens of humans where it is an etiologic agent of sinusitis, keratitis, skin lesions and an often fatal meningoencephalitis. Infections caused by this species are most often seen in regions with hot climates like Israel, India and the southern USA.
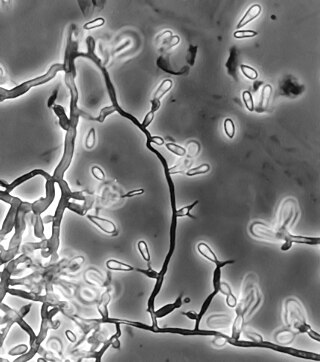
Exophiala jeanselmei is a saprotrophic fungus in the family Herpotrichiellaceae. Four varieties have been discovered: Exophiala jeanselmei var. heteromorpha, E. jeanselmei var. lecanii-corni, E. jeanselmei var. jeanselmei, and E. jeanselmei var. castellanii. Other species in the genus Exophiala such as E. dermatitidis and E. spinifera have been reported to have similar annellidic conidiogenesis and may therefore be difficult to differentiate.

Exophiala dermatitidis is a thermophilic black yeast, and a member of the Herpotrichiellaceae. While the species is only found at low abundance in nature, metabolically active strains are commonly isolated in saunas, steam baths, and dish washers. Exophiala dermatitidis only rarely causes infection in humans, however cases have been reported around the world. In East Asia, the species has caused lethal brain infections in young and otherwise healthy individuals. The fungus has been known to cause cutaneous and subcutaneous phaeohyphomycosis, and as a lung colonist in people with cystic fibrosis in Europe. In 2002, an outbreak of systemic E. dermatitidis infection occurred in women who had received contaminated steroid injections at North Carolina hospitals.
Sagenomella is a genus of filamentous Ascomycota fungus that has reported to cause systemic illness in animals. The genus was circumscribed by Walter Gams in 1978.
Ochroconis gallopava, also called Dactylaria gallopava or Dactylaria constricta var. gallopava, is a member of genus Dactylaria. Ochroconis gallopava is a thermotolerant, darkly pigmented fungus that causes various infections in fowls, turkeys, poults, and immunocompromised humans first reported in 1986. Since then, the fungus has been increasingly reported as an agent of human disease especially in recipients of solid organ transplants. Ochroconis gallopava infection has a long onset and can involve a variety of body sites. Treatment of infection often involves a combination of antifungal drug therapy and surgical excision.

Apophysomyces variabilis is an emerging fungal pathogen that can cause serious and sometimes fatal infection in humans. This fungus is a soil-dwelling saprobe with tropical to subtropical distribution. It is a zygomycete that causes mucormycosis, an infection in humans brought about by fungi in the order Mucorales. Infectious cases have been reported globally in locations including the Americas, Southeast Asia, India, and Australia. Apophysomyces variabilis infections are not transmissible from person to person.

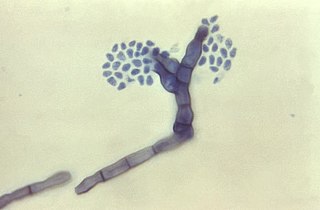
Cladophialophora bantiana is a melanin producing mold known to cause brain abscesses in humans. It is one of the most common causes of systemic phaeohyphomycosis in mammals. Cladophialophora bantiana is a member of the ascomycota and has been isolated from soil samples from around the world.
Thielavia subthermophila is a ubiquitous, filamentous fungus that is a member of the phylum Ascomycota and order Sordariales. Known to be found on plants of arid environments, it is an endophyte with thermophilic properties, and possesses dense, pigmented mycelium. Thielavia subthermophila has rarely been identified as a human pathogen, with a small number of clinical cases including ocular and brain infections. For treatment, antifungal drugs such as amphotericin B have been used topically or intravenously, depending upon the condition.
Scedosporiosis is the general name for any mycosis – i.e., fungal infection – caused by a fungus from the genus Scedosporium. Current population-based studies suggest Scedosporium prolificans and Scedosporium apiospermum to be among the most common infecting agents from the genus, although infections caused by other members thereof are not unheard of. The latter is an asexual form (anamorph) of another fungus, Pseudallescheria boydii. The former is a "black yeast", currently not characterized as well, although both of them have been described as saprophytes.
Fonsecaea compacta is a saprophytic fungal species found in the family Herpotrichiellaceae. It is a rare etiological agent of chromoblastomycosis, with low rates of correspondence observed from reports. The main active components of F. compacta are glycolipids, yet very little is known about its composition. F. compacta is widely regarded as a dysplastic variety of Fonsecaea pedrosoi, its morphological precursor. The genus Fonsecaea presently contains two species, F. pedrosoi and F. compacta. Over 100 strains of F. pedrosoi have been isolated but only two of F. compacta.

Rhinocladiella mackenziei is a deeply pigmented mold that is a common cause of human cerebral phaeohyphomycosis. Rhinocladiella mackenziei was believed to be endemic solely to the Middle East, due to the first cases of infection being limited to the region. However, cases of R. mackenziei infection are increasingly reported from regions outside the Middle East. This pathogen is unique in that the majority of cases have been reported from immunologically normal people.
Exophiala pisciphila is a mesophilic black yeast and member of the dark septate endophytes. This saprotrophic fungus is found commonly in marine and soil environments. It is abundant in harsh environments like soil contaminated with heavy metals. E. pisciphila forms symbiotic relationships with various plants by colonizing on roots, conferring resistance to drought and heavy metal stress. It is an opportunistic pathogen that commonly causes infections in captive fish and amphibians, while rarely causing disease in humans. Secondary metabolites produced by this species have potential clinical antibiotic and antiretroviral applications.
Arthrographis kalrae is an ascomycetous fungus responsible for human nail infections described in 1938 by Cochet as A. langeronii. A. kalrae is considered a weak pathogen of animals including human restricted to the outermost keratinized layers of tissue. Infections caused by this species are normally responsive to commonly used antifungal drugs with only very rare exceptions.
Cladophialophora arxii is a black yeast shaped dematiaceous fungus that is able to cause serious phaeohyphomycotic infections. C. arxii was first discovered in 1995 in Germany from a 22-year-old female patient suffering multiple granulomatous tracheal tumours. It is a clinical strain that is typically found in humans and is also capable of acting as an opportunistic fungus of other vertebrates Human cases caused by C. arxii have been reported from all parts of the world such as Germany and Australia.
References
- ↑ "ICD-11 - ICD-11 for Mortality and Morbidity Statistics". icd.who.int. Retrieved 30 June 2021.
- ↑ Johnstone, Ronald B. (2017). "25. Mycoses and Algal infections". Weedon's Skin Pathology Essentials (2nd ed.). Elsevier. p. 454. ISBN 978-0-7020-6830-0.
- 1 2 3 4 5 Milner, Dan A.; Solomon, Isaac (2020). "Phaeohyphomycosis". In Milner, Danny A. (ed.). Diagnostic Pathology: Infectious Diseases. Elsevier. p. 308. ISBN 978-0-323-61138-1.
- ↑ Arcobello, Jonathan T.; Revankar, Sanjay G. (February 2020). "Phaeohyphomycosis" . Seminars in Respiratory and Critical Care Medicine. 41 (1): 131–140. doi:10.1055/s-0039-3400957. ISSN 1098-9048. PMID 32000289. S2CID 210983369.
- ↑ Chander, Jagdish (2018). "14. Phaeohyphomycosis". Textbook of Medical Mycology (4th ed.). New Delhi: Jaypee Brothers Medical Publishers Ltd. pp. 269–296. ISBN 978-93-86261-83-0.
- ↑ Naggie S, Perfect JR (June 2009). "Molds: hyalohyphomycosis, phaeohyphomycosis, and zygomycosis". Clin. Chest Med. 30 (2): 337–53, vii–viii. doi:10.1016/j.ccm.2009.02.009. PMID 19375639.
- ↑ James, William D.; Berger, Timothy G.; et al. (2006). Andrews' Diseases of the Skin: clinical Dermatology. Saunders Elsevier. p. 324. ISBN 978-0-7216-2921-6.
- ↑ Boyce RD, Deziel PJ, Otley CC, et al. (December 2009). "Phaeohyphomycosis due to Alternaria species in transplant recipients". Transpl Infect Dis. 12 (3): 242–250. doi:10.1111/j.1399-3062.2009.00482.x. PMID 20002611. S2CID 23751797.
- ↑ Umemoto N, Demitsu T, Kakurai M, et al. (October 2009). "Two cases of cutaneous phaeohyphomycosis due to Exophiala jeanselmei: diagnostic significance of direct microscopical examination of the purulent discharge". Clin. Exp. Dermatol. 34 (7): e351–3. doi:10.1111/j.1365-2230.2009.03304.x. PMID 19456770. S2CID 40160899.
- ↑ Taj-Aldeen, Saad J.; Almaslamani, Muna; Alkhalf, Abdullatif; Al Bozom, Issam; Romanelli, Anna M.; Wickes, Brian L.; Fothergill, Annette W.; Sutton, Deanna A. (2010-05-01). "Cerebral phaeohyphomycosis due to Rhinocladiella mackenziei (formerly Ramichloridium mackenziei): a taxonomic update and review of the literature". Medical Mycology. 48 (3): 546–556. doi: 10.3109/13693780903383914 . ISSN 1369-3786. PMID 19886775.
- ↑ Ajello L, Georg LK, Steigbigel RT, Wang CJ (1974). "A case of phaeophyphomycosis caused by a new species of Philaphora". Mycologia. 66 (3): 490–498. doi:10.1080/00275514.1974.12019630. PMID 4601425. S2CID 34885774.
- 1 2 Revankar SG, Patterson JE, Sutton DA, Pullen R, Rinaldi MG (2002). "Disseminated phaeohyphomycosis: review of an emerging mycosis". Clinical Infectious Disease. 34 (4): 467–476. doi: 10.1086/338636 . PMID 11797173.
- 1 2 3 4 5 6 7 Seyedmousavi S, Guillot J, de Hoog GS (2013). "Phaeohyphomycoses, emerging opportunistic diseases in animals". Clinical Microbiology Reviews. 26 (1): 19–35. doi: 10.1128/CMR.00065-12 . PMC 3553675 . PMID 23297257.
- ↑ "Phaeohyphomycosis". The Merck Veterinary Manual. Retrieved 2019-06-17.
- ↑ Hasei M, Takeda K, Anazawa K, Nishibu A, Tanabe H, Mochizuki T (2013). "Case of phaeohyphomycosis producing sporotrichoid lesions". Journal of Dermatology. 40 (8): 638–640. doi:10.1111/1346-8138.12193. PMID 23734832.
- 1 2 Cai Q, Lv GX, Jiang YQ, Mei H, Hu SQ, Xu HB, Wu XF, Shen YN, Liu WD (2013). "The first case of phaeohyphomycosis caused by Rhinocladiella basitona in an immunocompetent child in China". Mycopathologia. 176: 101–105. doi:10.1007/s11046-013-9645-0. PMID 23591621.
- ↑ Bossler AD, Richter SS, Chavez AJ, Vogelgesang SA, Sutton DA, Grooters AM, Rinaldi MG, de Hoog GS, Pfaller MA (2003). "Exophiala oligosperma causing olecranon bursitis". Journal of Clinical Microbiology. 41 (10): 4779–4782. doi: 10.1128/JCM.41.10.4779-4782.2003 . PMC 254319 . PMID 14532219.
- ↑ Joyner PH, Shreve AA, Spahr J, Fountain AL, Sleeman JM (2006). "Phaeohyphomycosis in a free-living eastern box turtle (Terrapene carolina carolina)". Journal of Wildlife Diseases. 42 (4): 883–888. doi: 10.7589/0090-3558-42.4.883 . PMID 17255461.
- ↑ Bently RT, Faissler D, Sutherland-Smith J (2011). "Successful management of an intracranial phaeohypomycotic fungal granuloma in a dog". Journal of the American Veterinary Medical Association. 239 (4): 480–485. doi: 10.2460/javma.239.4.480 . PMID 21838585.
- ↑ Janovsky M, Gröne A, Ciardo D, Völlm J, Burnens A, Fatzer R, Bacciarini LN (2006). "Phaeohyphomycisis in a snow leopard (Uncia uncia) due to Cladophialophora bantiana". Journal of Comparative Pathology. 134 (2–3): 245–248. doi:10.1016/j.jcpa.2005.09.006. PMID 16542676.
- ↑ Frank C, Vemulapalli R, Lin T (2011). "Cerebral phaeohyphomycosis due to Cladophialophora bantiana in a Huacaya alpaca (Vicugna pacos)". Journal of Comparative Pathology. 145 (4): 410–413. doi:10.1016/j.jcpa.2011.02.003. PMID 21511274.