Coronary artery disease (CAD), also called coronary heart disease (CHD), ischemic heart disease (IHD), or simply heart disease, involves the reduction of blood flow to the heart muscle due to build-up of plaque (atherosclerosis) in the arteries of the heart. It is the most common of the cardiovascular diseases. Types include stable angina, unstable angina, myocardial infarction, and sudden cardiac death. A common symptom is chest pain or discomfort which may travel into the shoulder, arm, back, neck, or jaw. Occasionally it may feel like heartburn. Usually symptoms occur with exercise or emotional stress, last less than a few minutes, and improve with rest. Shortness of breath may also occur and sometimes no symptoms are present. In many cases, the first sign is a heart attack. Other complications include heart failure or an abnormal heartbeat.

Angina, also known as angina pectoris, is chest pain or pressure, usually due to insufficient blood flow to the heart muscle (myocardium).

The Heart Protection Study was a randomized controlled trial run by the Clinical Trial Service Unit, and funded by the Medical Research Council (MRC) and the British Heart Foundation (BHF) in the United Kingdom. It studied the use of the cholesterol lowering drug, simvastatin 40 mg and vitamin supplementation in people who were at risk of cardiovascular disease. It was led by Jane Armitage, an epidemiologist at the Clinical Trial Service Unit.

Atorvastatin, sold under the brand name Lipitor among others, is a statin medication used to prevent cardiovascular disease in those at high risk and to treat abnormal lipid levels. For the prevention of cardiovascular disease, statins are a first-line treatment. It is taken by mouth.
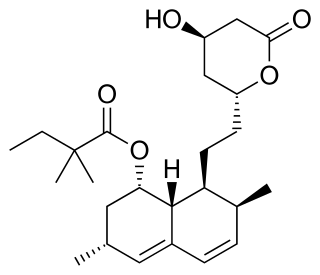
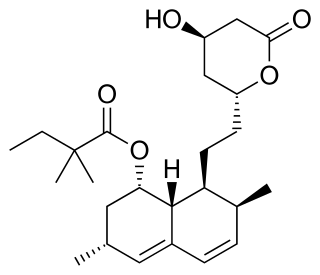
Simvastatin, sold under the brand name Zocor among others, is a lipid-lowering medication. It is used along with exercise, diet, and weight loss to decrease elevated lipid levels. It is also used to decrease the risk of heart problems in those at high risk. It is taken by mouth.

Fluvastatin is a member of the statin drug class, used to treat hypercholesterolemia and to prevent cardiovascular disease.

Coronary thrombosis is defined as the formation of a blood clot inside a blood vessel of the heart. This blood clot may then restrict blood flow within the heart, leading to heart tissue damage, or a myocardial infarction, also known as a heart attack.

Acute coronary syndrome (ACS) is a syndrome due to decreased blood flow in the coronary arteries such that part of the heart muscle is unable to function properly or dies. The most common symptom is centrally located chest pain, often radiating to the left shoulder or angle of the jaw, crushing, central and associated with nausea and sweating. Many people with acute coronary syndromes present with symptoms other than chest pain, particularly women, older patients, and patients with diabetes mellitus.

Percutaneous coronary intervention (PCI) is a non-surgical procedure used to treat narrowing of the coronary arteries of the heart found in coronary artery disease. The process involves combining coronary angioplasty with stenting, which is the insertion of a permanent wire-meshed tube that is either drug eluting (DES) or composed of bare metal (BMS). The stent delivery balloon from the angioplasty catheter is inflated with media to force contact between the struts of the stent and the vessel wall, thus widening the blood vessel diameter. After accessing the blood stream through the femoral or radial artery, the procedure uses coronary catheterization to visualise the blood vessels on X-ray imaging. After this, an interventional cardiologist can perform a coronary angioplasty, using a balloon catheter in which a deflated balloon is advanced into the obstructed artery and inflated to relieve the narrowing; certain devices such as stents can be deployed to keep the blood vessel open. Various other procedures can also be performed.
The Thrombolysis In Myocardial Infarction, or TIMI Study Group, is an Academic Research Organization (ARO) affiliated with Brigham and Women's Hospital and Harvard Medical School dedicated to advancing the knowledge and care of patients suffering from cardiovascular disease. The TIMI Study Group provides robust expertise in the key aspects of a clinical trial, including academic leadership, global trial management, biostatistics, clinical event adjudication, safety desk, medical hotline, and core laboratories. The group has its headquarters in Boston, Massachusetts.

A myocardial infarction (MI), commonly known as a heart attack, occurs when blood flow decreases or stops to a part of the heart, causing damage to the heart muscle. The most common symptom is chest pain or discomfort which may travel into the shoulder, arm, back, neck or jaw. Often it occurs in the center or left side of the chest and lasts for more than a few minutes. The discomfort may occasionally feel like heartburn. Other symptoms may include shortness of breath, nausea, feeling faint, a cold sweat or feeling tired. About 30% of people have atypical symptoms. Women more often present without chest pain and instead have neck pain, arm pain or feel tired. Among those over 75 years old, about 5% have had an MI with little or no history of symptoms. An MI may cause heart failure, an irregular heartbeat, cardiogenic shock or cardiac arrest.

Primary ventricular fibrillation (PVF) is an unpredictable and potentially fatal arrhythmia occurring during the acute phase of a myocardial infarction leading to immediate collapse and, if left untreated, leads to sudden cardiac death within minutes. In developed countries, PVF is a leading cause of death. Worldwide, the annual number of deaths caused by PVF is comparable to the number of deaths caused by road traffic accidents. A substantial portion of these deaths could be avoided by seeking immediate medical attention when symptoms are noticed.

Reperfusion therapy is a medical treatment to restore blood flow, either through or around, blocked arteries, typically after a heart attack. Reperfusion therapy includes drugs and surgery. The drugs are thrombolytics and fibrinolytics used in a process called thrombolysis. Surgeries performed may be minimally-invasive endovascular procedures such as a percutaneous coronary intervention (PCI), followed by a coronary angioplasty. The angioplasty uses the insertion of a balloon to open up the artery, with the possible additional use of one or more stents. Other surgeries performed are the more invasive bypass surgeries that graft arteries around blockages.

Management of acute coronary syndrome is targeted against the effects of reduced blood flow to the afflicted area of the heart muscle, usually because of a blood clot in one of the coronary arteries, the vessels that supply oxygenated blood to the myocardium. This is achieved with urgent hospitalization and medical therapy, including drugs that relieve chest pain and reduce the size of the infarct, and drugs that inhibit clot formation; for a subset of patients invasive measures are also employed. Basic principles of management are the same for all types of acute coronary syndrome. However, some important aspects of treatment depend on the presence or absence of elevation of the ST segment on the electrocardiogram, which classifies cases upon presentation to either ST segment elevation myocardial infarction (STEMI) or non-ST elevation acute coronary syndrome (NST-ACS); the latter includes unstable angina and non-ST elevation myocardial infarction (NSTEMI). Treatment is generally more aggressive for STEMI patients, and reperfusion therapy is more often reserved for them. Long-term therapy is necessary for prevention of recurrent events and complications.
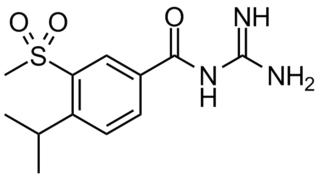
Cariporide is a selective Na+/H+ exchange inhibitor. Cariporide has been shown to actively suppress the cell death caused by oxidative stress.

Ischemic cardiomyopathy is a type of cardiomyopathy caused by a narrowing of the coronary arteries which supply blood to the heart. Typically, patients with ischemic cardiomyopathy have a history of acute myocardial infarction, however, it may occur in patients with coronary artery disease, but without a past history of acute myocardial infarction. This cardiomyopathy is one of the leading causes of sudden cardiac death. The adjective ischemic means characteristic of, or accompanied by, ischemia — local anemia due to mechanical obstruction of the blood supply.
The HDL-Atherosclerosis Treatment Study, also known as HATS, was a three-year double-blind trial involving 160 people with coronary heart disease (CHD) who had a low HDL and near normal LDL. The study compared a combination of simvastatin and niacin with antioxidant vitamin therapy. Using angiography, coronary artery stenosis progressed when using placebo or antioxidant alone, and regressed with the combination of simvastatin and niacin. The study demonstrated a 90% reduction in CHD death, nonfatal heart attacks, stroke, or revascularization for worsening angina. It was published in 2001.
The West of Scotland Coronary Prevention Study, also known as WOSCOPS, was a randomized, double-blind, placebo-controlled clinical trial, published in 1995. It compared 40mg of the lipid-lowering drug pravastatin to placebo in 6, 595 men who had a mean cholesterol of 7 mmol/L but no previous history of a heart attack. The study concluded that statin treatment for primary prevention reduced coronary heart disease (CHD) events by 31% after nearly five years of treatment.
The Pravastatin or atorvastatin evaluation and infection therapy - thrombolysis in myocardial infarction 22, also known as PROVE-IT TIMI 22, was a randomized, double-blind, clinical trial that recruited 4,162 people admitted within 10 days of an acute coronary event and randomised them to the lipid-lowering drugs pravastatin (40mg) or atorvastatin (80mg) and a 10 day course of the antibiotic gatifloxacin or placebo. The participants enrolled at 349 sites across Australia, Europe, and North America between November 2000 and December 2001, and the study concluded that statin treatment for secondary prevention reduced coronary heart disease (CHD) events and that atorvastatin had a more marked effect than pravastatin. The study was published in The New England Journal of Medicine and reported at the American College of Cardiology Annual Scientific Session in 2004.