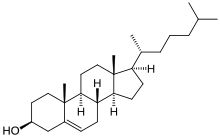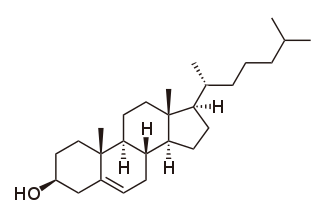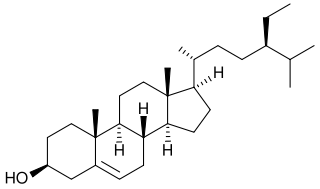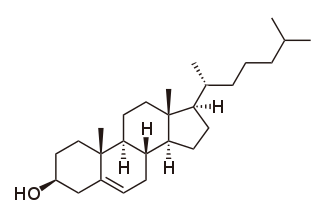
Cholesterol is the principal sterol of all higher animals, distributed in body tissues, especially the brain and spinal cord, and in animal fats and oils.
High-density lipoprotein (HDL) is one of the five major groups of lipoproteins. Lipoproteins are complex particles composed of multiple proteins which transport all fat molecules (lipids) around the body within the water outside cells. They are typically composed of 80–100 proteins per particle. HDL particles enlarge while circulating in the blood, aggregating more fat molecules and transporting up to hundreds of fat molecules per particle.

Low-density lipoprotein (LDL) is one of the five major groups of lipoprotein that transport all fat molecules around the body in extracellular water. These groups, from least dense to most dense, are chylomicrons, very low-density lipoprotein (VLDL), intermediate-density lipoprotein (IDL), low-density lipoprotein (LDL) and high-density lipoprotein (HDL). LDL delivers fat molecules to cells. LDL is involved in atherosclerosis, a process in which it is oxidized within the walls of arteries.

Atherosclerosis is a pattern of the disease arteriosclerosis, characterized by development of abnormalities called lesions in walls of arteries. These lesions may lead to narrowing of the arterial walls due to buildup of atheromatous plaques. At onset there are usually no symptoms, but if they develop, symptoms generally begin around middle age. In severe cases, it can result in coronary artery disease, stroke, peripheral artery disease, or kidney disorders, depending on which body part(s) the affected arteries are located in the body.

Statins are a class of medications that reduce illness and mortality in people who are at high risk of cardiovascular disease. They are the most commonly prescribed cholesterol-lowering drugs.
Lipid-lowering agents, also sometimes referred to as hypolipidemic agents, cholesterol-lowering drugs, or antihyperlipidemic agents are a diverse group of pharmaceuticals that are used to lower the level of lipids and lipoproteins such as cholesterol, in the blood (hyperlipidemia). The American Heart Association recommends the descriptor 'lipid lowering agent' be used for this class of drugs rather than the term 'hypolipidemic'.
Dyslipidemia is a metabolic disorder characterized by abnormally high or low amounts of any or all lipids or lipoproteins in the blood. Dyslipidemia is a risk factor for the development of atherosclerotic cardiovascular diseases (ASCVD), which include coronary artery disease, cerebrovascular disease, and peripheral artery disease. Although dyslipidemia is a risk factor for ASCVD, abnormal levels don't mean that lipid lowering agents need to be started. Other factors, such as comorbid conditions and lifestyle in addition to dyslipidemia, is considered in a cardiovascular risk assessment. In developed countries, most dyslipidemias are hyperlipidemias; that is, an elevation of lipids in the blood. This is often due to diet and lifestyle. Prolonged elevation of insulin resistance can also lead to dyslipidemia. Likewise, increased levels of O-GlcNAc transferase (OGT) may cause dyslipidemia.

Hypertriglyceridemia is the presence of high amounts of triglycerides in the blood. Triglycerides are the most abundant fatty molecule in most organisms. Hypertriglyceridemia occurs in various physiologic conditions and in various diseases, and high triglyceride levels are associated with atherosclerosis, even in the absence of hypercholesterolemia and predispose to cardiovascular disease.

Combined hyperlipidemia is a commonly occurring form of hypercholesterolemia characterised by increased LDL and triglyceride concentrations, often accompanied by decreased HDL. On lipoprotein electrophoresis it shows as a hyperlipoproteinemia type IIB. It is the most commonly inherited lipid disorder, occurring in around one in 200 persons. In fact, almost one in five individuals who develop coronary heart disease before the age of 60 have this disorder.

Ezetimibe is a medication used to treat high blood cholesterol and certain other lipid abnormalities. Generally it is used together with dietary changes and a statin. Alone, it is less preferred than a statin. It is taken by mouth. It is also available in the fixed combinations ezetimibe/simvastatin, ezetimibe/atorvastatin, ezetimibe/rosuvastatin, and ezetimibe/bempedoic acid.
Hyperlipidemia is abnormally high levels of any or all lipids or lipoproteins in the blood. The term hyperlipidemia refers to the laboratory finding itself and is also used as an umbrella term covering any of various acquired or genetic disorders that result in that finding. Hyperlipidemia represents a subset of dyslipidemia and a superset of hypercholesterolemia. Hyperlipidemia is usually chronic and requires ongoing medication to control blood lipid levels.
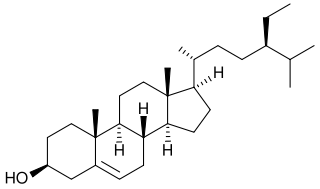
Phytosterols are phytosteroids, similar to cholesterol, that serve as structural components of biological membranes of plants. They encompass plant sterols and stanols. More than 250 sterols and related compounds have been identified. Free phytosterols extracted from oils are insoluble in water, relatively insoluble in oil, and soluble in alcohols.

The low-density lipoprotein receptor (LDL-R) is a mosaic protein of 839 amino acids that mediates the endocytosis of cholesterol-rich low-density lipoprotein (LDL). It is a cell-surface receptor that recognizes apolipoprotein B100 (ApoB100), which is embedded in the outer phospholipid layer of very low-density lipoprotein (VLDL), their remnants—i.e. intermediate-density lipoprotein (IDL), and LDL particles. The receptor also recognizes apolipoprotein E (ApoE) which is found in chylomicron remnants and IDL. In humans, the LDL receptor protein is encoded by the LDLR gene on chromosome 19. It belongs to the low density lipoprotein receptor gene family. It is most significantly expressed in bronchial epithelial cells and adrenal gland and cortex tissue.
The lipid hypothesis is a medical theory postulating a link between blood cholesterol levels and the occurrence of cardiovascular disease. A summary from 1976 described it as: "measures used to lower the plasma lipids in patients with hyperlipidemia will lead to reductions in new events of coronary heart disease". It states, more concisely, that "decreasing blood cholesterol [...] significantly reduces coronary heart disease".

Familial hypercholesterolemia (FH) is a genetic disorder characterized by high cholesterol levels, specifically very high levels of low-density lipoprotein cholesterol, in the blood and early cardiovascular diseases. The most common mutations diminish the number of functional LDL receptors in the liver or produce abnormal LDL receptors that never go to the cell surface to function properly. Since the underlying body biochemistry is slightly different in individuals with FH, their high cholesterol levels are less responsive to the kinds of cholesterol control methods which are usually more effective in people without FH. Nevertheless, treatment is usually effective.

Proprotein convertase subtilisin/kexin type 9 (PCSK9) is an enzyme encoded by the PCSK9 gene in humans on chromosome 1. It is the 9th member of the proprotein convertase family of proteins that activate other proteins. Similar genes (orthologs) are found across many species. As with many proteins, PCSK9 is inactive when first synthesized, because a section of peptide chains blocks their activity; proprotein convertases remove that section to activate the enzyme. The PCSK9 gene also contains one of 27 loci associated with increased risk of coronary artery disease.
The chronic endothelial injury hypothesis is one of two major mechanisms postulated to explain the underlying cause of atherosclerosis and coronary heart disease (CHD), the other being the lipid hypothesis. Although an ongoing debate involving connection between dietary lipids and CHD sometimes portrays the two hypotheses as being opposed, they are in no way mutually exclusive. Moreover, since the discovery of the role of LDL cholesterol (LDL-C) in the pathogenesis of atherosclerosis, the two hypotheses have become tightly linked by a number of molecular and cellular processes.
A lipid profile or lipid panel is a panel of blood tests used to find abnormalities in blood lipid concentrations. The results of this test can identify certain genetic diseases and can determine approximate risks for cardiovascular disease, certain forms of pancreatitis, and other diseases.
The Portfolio Diet is a therapeutic plant-based diet created by British researcher David J. Jenkins in 2003 to lower blood cholesterol. The diet emphasizes using a portfolio of foods or food components that have been found to associate with cholesterol lowering to enhance this effect. Soluble fiber, soy protein, plant sterols, and nuts are the four essential components of Portfolio diet. The diet is low in saturated fat, high in fibre. Researchers have found it has comparable blood cholesterol effect to statin treatment.
Therapeutic Lifestyle Changes, also known as the TLC Diet, is a dietary pattern recommended by the National Cholesterol Education Program, part of the National Institutes of Health, to control hypercholesterolemia. This pattern focuses on saturated fats and cholesterol, dietary options to enhance LDL cholesterol lowering, weight control, and physical activity.