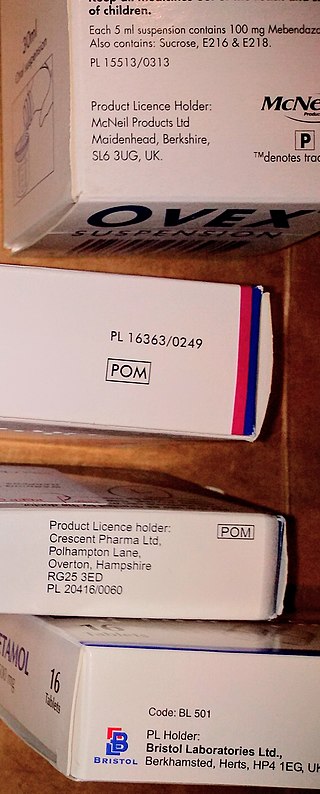
Over-the-counter (OTC) drugs are medicines sold directly to a consumer without a requirement for a prescription from a healthcare professional, as opposed to prescription drugs, which may be supplied only to consumers possessing a valid prescription. In many countries, OTC drugs are selected by a regulatory agency to ensure that they contain ingredients that are safe and effective when used without a physician's care. OTC drugs are usually regulated according to their active pharmaceutical ingredient (API) rather than final products. By regulating APIs instead of specific drug formulations, governments allow manufacturers the freedom to formulate ingredients, or combinations of ingredients, into proprietary mixtures.

A pharmacist, also known as a chemist or a druggist, is a healthcare professional who specializes in the preparation, dispensing, and management of medications to ensure safe and effective use, while also providing medication counseling and guidance to patients and healthcare providers. Also, pharmacists often serve as primary care providers in the community, and may offer other services such as health screenings and immunizations.

Pharmacy is the science and practice of discovering, producing, preparing, dispensing, reviewing and monitoring medications, aiming to ensure the safe, effective, and affordable use of medicines. It is a miscellaneous science as it links health sciences with pharmaceutical sciences and natural sciences. The professional practice is becoming more clinically oriented as most of the drugs are now manufactured by pharmaceutical industries. Based on the setting, pharmacy practice is either classified as community or institutional pharmacy. Providing direct patient care in the community of institutional pharmacies is considered clinical pharmacy.

A prescription, often abbreviated ℞ or Rx, is a formal communication from a physician or other registered healthcare professional to a pharmacist, authorizing them to dispense a specific prescription drug for a specific patient. Historically, it was a physician's instruction to an apothecary listing the materials to be compounded into a treatment—the symbol ℞ comes from the first word of a medieval prescription, Latin recipere, that gave the list of the materials to be compounded.
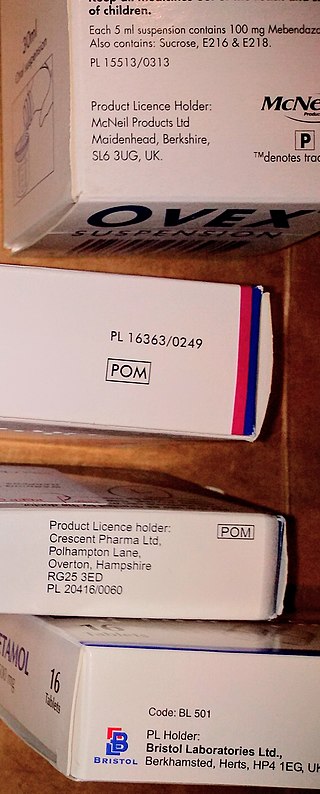
A prescription drug is a pharmaceutical drug that is permitted to be dispensed only to those with a medical prescription. In contrast, over-the-counter drugs can be obtained without a prescription. The reason for this difference in substance control is the potential scope of misuse, from drug abuse to practicing medicine without a license and without sufficient education. Different jurisdictions have different definitions of what constitutes a prescription drug.
The Pharmaceutical Benefits Scheme (PBS) is a program of the Australian Government that subsidises prescription medication for Australian citizens and permanent residents, as well as international visitors covered by a reciprocal health care agreement. The PBS is separate to the Medicare Benefits Schedule, a list of health care services that can be claimed under Medicare, Australia's universal health care insurance scheme.
An independent pharmacy is a retail pharmacy that is not directly affiliated with any chain of pharmacies and is not owned by a publicly traded company. Independent pharmacies are pharmacist-owned, privately held businesses in varying practice settings. They include single-store operations, pharmacist-owned multiple store locations, franchise, compounding, long-term care (LTC), specialty, and supermarket pharmacy operation. Independent pharmacy owners generally have more flexibility to build personalized customer relationships and they strive to differentiate their services from big-chain corporations.
An online pharmacy, internet pharmacy, or mail-order pharmacy is a pharmacy that operates over the Internet and sends orders to customers through mail, shipping companies, or online pharmacy web portal.

In the field of pharmacy, compounding is preparation of a custom medication to fit a unique need of a patient that cannot be met with commercially available products. This may be done for medical reasons, such as administration in a different format, to avoid a non-active ingredient the patient is allergic to, or to provide an exact dose that isn't commercially available. Patient-specific compounding according to a prescriber's specifications is referred to as "traditional" compounding. The nature of patient need for such customization can range from absolute necessity to individual optimality to even preference.
Pharmaceutical policy is a branch of health policy that deals with the development, provision and use of medications within a health care system. It embraces drugs, biologics, vaccines and natural health products.
A veterinary pharmacist is a specially trained pharmacist who dispenses veterinary drugs and supplies or products and advice to owners of companion animals and livestock. In addition, they advise the regulatory bodies and are involved in the formulation of veterinary drugs. Veterinary pharmacy is a field of pharmacy practice, in which veterinary pharmacists may compound medications, fill prescriptions, and manage drug therapies for animals. Veterinary pharmacists are licensed pharmacists who specialize in the distribution of medications for animals.

Clinical pharmacy is the branch of pharmacy in which clinical pharmacists provide direct patient care that optimizes the use of medication and promotes health, wellness, and disease prevention. Clinical pharmacists care for patients in all health care settings but the clinical pharmacy movement initially began inside hospitals and clinics. Clinical pharmacists often work in collaboration with physicians, physician assistants, nurse practitioners, and other healthcare professionals. Clinical pharmacists can enter into a formal collaborative practice agreement with another healthcare provider, generally one or more physicians, that allows pharmacists to prescribe medications and order laboratory tests.

A pharmacy is a retail shop which provides pharmaceutical drugs, among other products. At the pharmacy, a pharmacist oversees the fulfillment of medical prescriptions and is available to counsel patients about prescription and over-the-counter drugs or about health problems and wellness issues. A typical pharmacy would be in the commercial area of a community.
Electronic prescription is the computer-based electronic generation, transmission, and filling of a medical prescription, taking the place of paper and faxed prescriptions. E-prescribing allows a physician, physician assistant, pharmacist, or nurse practitioner to use digital prescription software to electronically transmit a new prescription or renewal authorization to a community or mail-order pharmacy. It outlines the ability to send error-free, accurate, and understandable prescriptions electronically from the healthcare provider to the pharmacy. E-prescribing is meant to reduce the risks associated with traditional prescription script writing. It is also one of the major reasons for the push for electronic medical records. By sharing medical prescription information, e-prescribing seeks to connect the patient's team of healthcare providers to facilitate knowledgeable decision making.
Automatic Generic Substitution is a proposal by the Department of Health (DH) whereby in January 2010 pharmacists could be obliged to substitute a generic version of a medication even if the prescriber had written the prescription for a specific brand, as part of a new deal on drug pricing.
KwikMed is an approved online pharmacy in the United States which has been granted regulatory approval to operate and sell medications online. Based in Salt Lake City, Utah, KwikMed's parent company, Phoenix Capital Management, is located in Scottsdale, Arizona. Specifically, KwikMed has been granted regulatory approval to prescribe medications for erectile dysfunction, male pattern hair loss and smoking cessation provided specific operating procedures are followed.
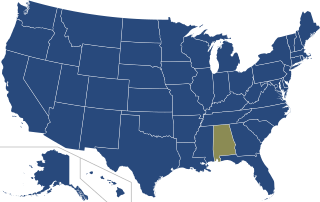
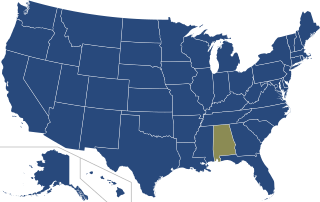
In the United States, prescription monitoring programs (PMPs) or prescription drug monitoring programs (PDMPs) are state-run programs which collect and distribute data about the prescription and dispensation of federally controlled substances and, depending on state requirements, other potentially abusable prescription drugs. PMPs are meant to help prevent adverse drug-related events such as opioid overdoses, drug diversion, and substance abuse by decreasing the amount and/or frequency of opioid prescribing, and by identifying those patients who are obtaining prescriptions from multiple providers or those physicians overprescribing opioids.

Telepharmacy is the delivery of pharmaceutical care via telecommunications to patients in locations where they may not have direct contact with a pharmacist. It is an instance of the wider phenomenon of telemedicine, as implemented in the field of pharmacy. Telepharmacy services include drug therapy monitoring, patient counseling, prior authorization and refill authorization for prescription drugs, and monitoring of formulary compliance with the aid of teleconferencing or videoconferencing. Remote dispensing of medications by automated packaging and labeling systems can also be thought of as an instance of telepharmacy. Telepharmacy services can be delivered at retail pharmacy sites or through hospitals, nursing homes, or other medical care facilities.
Pharmacy in the United Kingdom has been an integral part of the National Health Service since it was established in 1948. Unlike the rest of the NHS, pharmacies are largely privately provided apart from those in hospitals, and even these are now often privately run.
A collaborative practice agreement (CPA) is a legal document in the United States that establishes a legal relationship between clinical pharmacists and collaborating physicians that allows for pharmacists to participate in collaborative drug therapy management (CDTM).