Medical psychology or medico-psychology is the application of psychological principles to the practice of medicine, primarily drug-oriented, for both physical and mental disorders.

A pharmacist is a healthcare professional who specializes in the preparation, dispensing, and management of medications and who provides pharmaceutical advice and guidance. Pharmacists often serve as primary care providers in the community, and may offer other services such as health screenings and immunizations.

Pharmacy is the science and practice of discovering, producing, preparing, dispensing, reviewing and monitoring medications, aiming to ensure the safe, effective, and affordable use of medicines. It is a miscellaneous science as it links health sciences with pharmaceutical sciences and natural sciences. The professional practice is becoming more clinically oriented as most of the drugs are now manufactured by pharmaceutical industries. Based on the setting, pharmacy practice is either classified as community or institutional pharmacy. Providing direct patient care in the community of institutional pharmacies is considered clinical pharmacy.

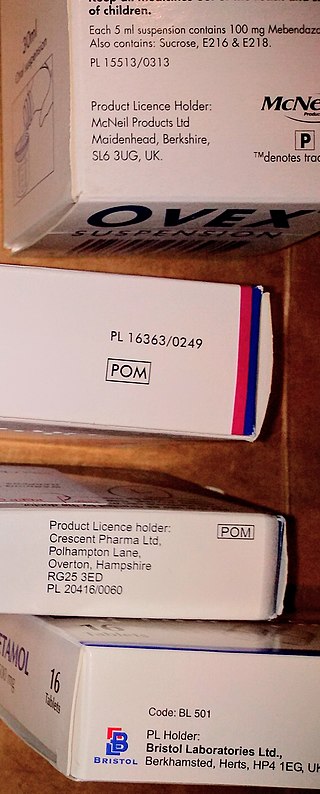
A prescription, often abbreviated ℞ or Rx, is a formal communication from a physician or other registered healthcare professional to a pharmacist, authorizing them to dispense a specific prescription drug for a specific patient. Historically, it was a physician's instruction to an apothecary listing the materials to be compounded into a treatment—the symbol ℞ comes from the first word of a medieval prescription, Latin recipere, that gave the list of the materials to be compounded.
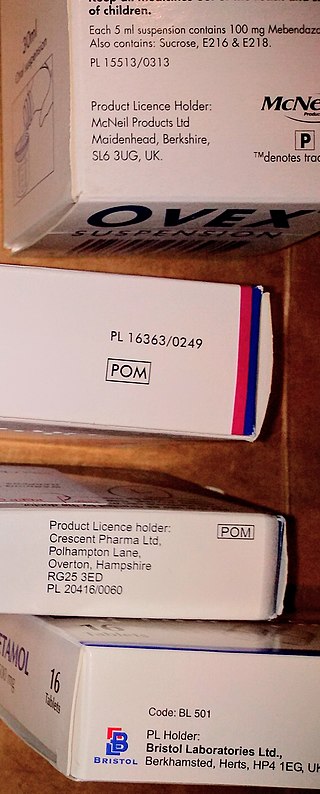
A prescription drug is a pharmaceutical drug that is permitted to be dispensed only to those with a medical prescription. In contrast, over-the-counter drugs can be obtained without a prescription. The reason for this difference in substance control is the potential scope of misuse, from drug abuse to practicing medicine without a license and without sufficient education. Different jurisdictions have different definitions of what constitutes a prescription drug.
Polypharmacy (polypragmasia) is an umbrella term to describe the simultaneous use of multiple medicines by a patient for their conditions. The term polypharmacy is often defined as regularly taking five or more medicines but there is no standard definition and the term has also been used in the context of when a person is prescribed 2 or more medications at the same time. Polypharmacy may be the consequence of having multiple long-term conditions, also known as multimorbidity and is more common in people who are older. In some cases, an excessive number of medications at the same time is worrisome, especially for people who are older with many chronic health conditions, because this increases the risk of an adverse event in that population. In many cases, polypharmacy cannot be avoided, but 'appropriate polypharmacy' practices are encouraged to decrease the risk of adverse effects. Appropriate polypharmacy is defined as the practice of prescribing for a person who has multiple conditions or complex health needs by ensuring that medications prescribed are optimized and follow 'best evidence' practices.
Pharmacotherapy, also known as pharmacological therapy or drug therapy, is defined as medical treatment that utilizes one or more pharmaceutical drugs to improve on-going symptoms, treat the underlying condition, or act as a prevention for other diseases (prophylaxis).
Pharmaceutical policy is a branch of health policy that deals with the development, provision and use of medications within a health care system. It embraces drugs, biologics, vaccines and natural health products.
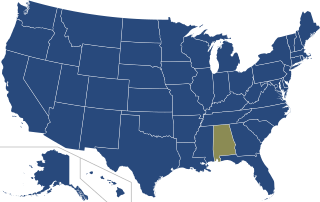
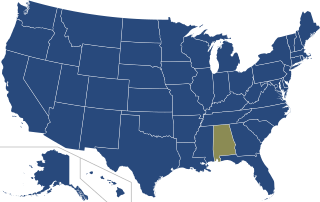
The prescriptive authority for psychologists (RxP) movement is a movement in the United States of America among certain psychologists to give prescriptive authority to psychologists with predoctoral or postdoctoral graduate-level training in clinical psychopharmacology; successful passage of a standardized, national examination ; supervised clinical experience; or a certificate from the Department of Defense Psychopharmacology Demonstration Project; or a diploma from the Prescribing Psychologists Register to enable them, according to state law, to prescribe psychotropic medications to treat mental disorders. This approach is non-traditional medical training focused on the specialized training to prescribe for mental health disorders by a psychologist. It includes rigorous didactics and supervised clinical experience. Legislation pertaining to prescriptive authority for psychologists has been introduced over 180 times in over half of the United States. It has passed in six states, due largely to substantial lobbying efforts by the American Psychological Association (APA), the largest professional organization of psychologists in the world with over 146,000 members. Prior to RxP legislation and in American states where it has not been passed, this role has been played by psychiatrists, who possess a medical degree and thus the authority to prescribe medication, but more frequently by primary care providers who can prescribe psychotropics, but lack extensive training in psychotropic drugs and in diagnosing and treating psychological disorders. According to the APA, the movement is a reaction to the growing public need for mental health services, particularly in under-resourced areas where patients have little or no access to psychiatrists.
Pharmacy residency is education a pharmacist can pursue beyond the degree required for licensing as a pharmacist. A pharmacy residency program allows for the implementation of skill set and knowledge acquired in pharmacy school through interaction with the public either in a hospital setting or community practice. The program is done over a span of about 2yrs after graduation from pharmacy school and licensure as a pharmacist. Pharmacy residency helps improve the resume of a pharmacist so as to increase chances of obtaining employment outside community practice. A 2022 review suggested that there is sufficient evidence that residency develops key competencies for junior pharmacists.
Pharmacy in China involves the activities engaged in the preparation, standardization and dispensing of drugs, and its scope includes the cultivation of plants that are used as drugs, the synthesis of chemical compounds of medicinal value, and the analysis of medicinal agents. Pharmacists in China are responsible for the preparation of the dosage forms of drugs, such as tablets, capsules, and sterile solutions for injection. They compound physicians', dentists', and veterinarians' prescriptions for drugs. Pharmacological activities are also closely related to pharmacy in China.

A pharmacy is a retail shop which provides pharmaceutical drugs, among other products. At the pharmacy, a pharmacist oversees the fulfillment of medical prescriptions and is available to counsel patients about prescription and over-the-counter drugs or about health problems and wellness issues. A typical pharmacy would be in the commercial area of a community.
Electronic prescription is the computer-based electronic generation, transmission, and filling of a medical prescription, taking the place of paper and faxed prescriptions. E-prescribing allows a physician, physician assistant, pharmacist, or nurse practitioner to use digital prescription software to electronically transmit a new prescription or renewal authorization to a community or mail-order pharmacy. It outlines the ability to send error-free, accurate, and understandable prescriptions electronically from the healthcare provider to the pharmacy. E-prescribing is meant to reduce the risks associated with traditional prescription script writing. It is also one of the major reasons for the push for electronic medical records. By sharing medical prescription information, e-prescribing seeks to connect the patient's team of healthcare providers to facilitate knowledgeable decision making.
Medication therapy management, generally called medicine use review in the United Kingdom, is a service provided typically by pharmacists, medical affairs, and RWE scientists that aims to improve outcomes by helping people to better understand their health conditions and the medications used to manage them. This includes providing education on the disease state and medications used to treat the disease state, ensuring that medicines are taken correctly, reducing waste due to unused medicines, looking for any side effects, and providing education on how to manage any side effects. The process that can be broken down into five steps: medication therapy review, personal medication record, medication-related action plan, intervention and or referral, and documentation and follow-up.
Drug therapy problems (DTPs) represent the categorization and definition of clinical problems related to the use of medications or "drugs" in the field of pharmaceutical care. In the course of clinical practice, DTPs are often identified, prevented, and/or resolved by pharmacists in the course of medication therapy management, as experts on the safety and efficacy of medications, but other healthcare professionals may also manage DTPs.
Psychiatric pharmacy, also known as mental health pharmacy, is the area of clinical pharmacy specializing in the treatment of people with psychiatric illnesses through the use of psychotropic medications. It is a branch of neuropsychiatric pharmacy, which includes neurologic pharmacy. Areas where psychiatric pharmacists are found most abundantly are in chemical dependency, developmental disabilities, long-term care facilities, adherence clinics, mental health clinics, and within the prison system. However, psychiatry and neurology are not the only areas where psychiatric pharmacists require comprehensive knowledge. They must also be proficient in clinical problem solving, interprofessionalism, and communication with understanding and empathy for the patient population they serve, as they are a sensitive group.
Advanced Practice Registered Nurse (APRN) refers to a nurse with advanced education, typically at least a master's degree, and certification by a national certifying program. The APRN provides specialized and multifaceted care and are able to do 60 to 80 percent of preventative and primary care done by physicians. Minnesota Statutes section 148.171, subd. 3 states that in Minnesota, APRN "means an individual licensed as a registered nurse by the board, and certified by a national nurse certification organization acceptable to the board to practice as a clinical nurse specialist, nurse anesthetist, nurse midwife, or nurse practitionerr".
A collaborative practice agreement (CPA) is a legal document in the United States that establishes a legal relationship between clinical pharmacists and collaborating physicians that allows for pharmacists to participate in collaborative drug therapy management (CDTM).
Travel health nursing is a nursing specialty which promotes the health and safety of national and international travelers. Similar to travel medicine, it is an interdisciplinary practice which draws from the knowledge bases of vaccines, epidemiology, tropical medicine, public health, and health education. Travel nursing has experienced an increase in global demand due to the evolution of travel medicine. Travel health nursing was recognized during the 1980s as an emerging occupation to meet the needs of the traveling public, and additional education and training was established. Travel health nurses typically work in "private practice, hospital outpatient units, universities, the government, and the military", and have more opportunities and leadership roles as travel has become more common. However, they also experience organizational and support-related conflicts with general practitioners and patients in healthcare settings.
Comprehensive medication management (CMM) is the process of delivering clinical services aimed at ensuring a patient's medications (including prescribed, over-the-counter, vitamins, supplements and alternative) are individually assessed to determine that they have an appropriate reason for use, are efficacious for treating their respective medical condition or helping meet defined patient or clinical goals, are safe considering comorbidities and other medications being taken, and are able to be taken by the patient as intended without difficulty.