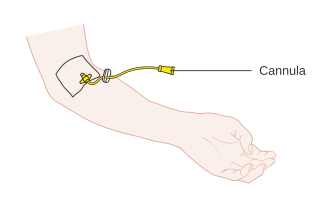
Phlebotomy is the process of making a puncture in a vein, usually in the arm, with a cannula for the purpose of drawing blood. The procedure itself is known as a venipuncture, which is also used for intravenous therapy. A person who performs a phlebotomy is called a phlebotomist, although most doctors, nurses, and other technicians can also carry out a phlebotomy. In contrast, phlebectomy is the removal of a vein.

A local anesthetic (LA) is a medication that causes absence of all sensation in a specific body part without loss of consciousness, as opposed to a general anesthetic, which eliminates all sensation in the entire body and causes unconsciousness. Local anesthetics are most commonly used to eliminate pain during or after surgery. When it is used on specific nerve pathways, paralysis also can be induced.

A vacutainer blood collection tube is a sterile glass or plastic test tube with a colored rubber stopper creating a vacuum seal inside of the tube, facilitating the drawing of a predetermined volume of liquid. Vacutainer tubes may contain additives designed to stabilize and preserve the specimen prior to analytical testing. Tubes are available with a safety-engineered stopper, with a variety of labeling options and draw volumes. The color of the top indicates the additives in the vial.

A hypodermic needle, one of a category of medical tools which enter the skin, called sharps, is a very thin, hollow tube with one sharp tip. It is commonly used with a syringe, a hand-operated device with a plunger, to inject substances into the body or extract fluids from the body. Large-bore hypodermic intervention is especially useful in catastrophic blood loss or treating shock.

Pleurisy, also known as pleuritis, is inflammation of the membranes that surround the lungs and line the chest cavity (pleurae). This can result in a sharp chest pain while breathing. Occasionally the pain may be a constant dull ache. Other symptoms may include shortness of breath, cough, fever, or weight loss, depending on the underlying cause. Pleurisy can be caused by a variety of conditions, including viral or bacterial infections, autoimmune disorders, and pulmonary embolism.
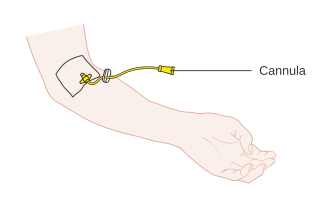
A cannula is a tube that can be inserted into the body, often for the delivery or removal of fluid or for the gathering of samples. In simple terms, a cannula can surround the inner or outer surfaces of a trocar needle thus extending the effective needle length by at least half the length of the original needle. Its size mainly ranges from 14 to 26 gauge. Different-sized cannula have different colours as coded.

A blood test is a laboratory analysis performed on a blood sample that is usually extracted from a vein in the arm using a hypodermic needle, or via fingerprick. Multiple tests for specific blood components, such as a glucose test or a cholesterol test, are often grouped together into one test panel called a blood panel or blood work. Blood tests are often used in health care to determine physiological and biochemical states, such as disease, mineral content, pharmaceutical drug effectiveness, and organ function. Typical clinical blood panels include a basic metabolic panel or a complete blood count. Blood tests are also used in drug tests to detect drug abuse.

Serum-separating tubes, also known as serum separator tubes or SSTs, are test tubes used in clinical chemistry tests requiring blood serum.

A blood culture is a medical laboratory test used to detect bacteria or fungi in a person's blood. Under normal conditions, the blood does not contain microorganisms: their presence can indicate a bloodstream infection such as bacteremia or fungemia, which in severe cases may result in sepsis. By culturing the blood, microbes can be identified and tested for resistance to antimicrobial drugs, which allows clinicians to provide an effective treatment.

Bone marrow examination refers to the pathologic analysis of samples of bone marrow obtained by bone marrow biopsy and bone marrow aspiration. Bone marrow examination is used in the diagnosis of a number of conditions, including leukemia, multiple myeloma, lymphoma, anemia, and pancytopenia. The bone marrow produces the cellular elements of the blood, including platelets, red blood cells and white blood cells. While much information can be gleaned by testing the blood itself, it is sometimes necessary to examine the source of the blood cells in the bone marrow to obtain more information on hematopoiesis; this is the role of bone marrow aspiration and biopsy.

Fear of needles, known in medical literature as needle phobia, is the extreme fear of medical procedures involving injections or hypodermic needles. This can lead to avoidance of medical care and vaccine hesitancy.
Infiltration is the diffusion or accumulation of foreign substances in amounts excess of the normal. The material collected in those tissues or cells is called infiltrate.

Radial artery puncture is a medical procedure performed to obtain a sample of arterial blood for gas analysis. A needle is inserted into the radial artery and spontaneously fills with blood. The syringe is either prepacked with a small amount of heparin to prevent coagulation, or must be heparinised, by drawing up a small amount of heparin and squirting it out again.. The available evidence suggests that the use of local anaesthesia, prior to arterial puncture, does not reduce the perceived pain of the procedure.
The Keidel vacuum tube was a type of blood collecting device, first manufactured by Hynson, Wescott and Dunning in around 1922. This vacuum was one of the first evacuated systems, predating the more well known Vacutainer. Its primary use was to test for syphilis and typhoid fever.

A winged infusion set—also known as "butterfly" or "scalp vein" set—is a device specialized for venipuncture: i.e. for accessing a superficial vein or artery for either intravenous injection or phlebotomy. It consists, from front to rear, of a hypodermic needle, two bilateral flexible "wings", flexible small-bore transparent tubing, and lastly a connector. This connector attaches to another device: e.g. syringe, vacuum tube holder/hub, or extension tubing from an infusion pump or gravity-fed infusion/transfusion bag/bottle.
Veterinary anesthesia is a specialization in the veterinary medicine field dedicated to the proper administration of anesthetic agents to non-human animals to control their consciousness during procedures. A veterinarian or a Registered Veterinary Technician administers these drugs to minimize stress, destructive behavior, and the threat of injury to both the patient and the doctor. The duration of the anesthesia process goes from the time before an animal leaves for the visit to the time after the animal reaches home after the visit, meaning it includes care from both the owner and the veterinary staff. Generally, anesthesia is used for a wider range of circumstances in animals than in people not only due to their inability to cooperate with certain diagnostic or therapeutic procedures, but also due to their species, breed, size, and corresponding anatomy. Veterinary anesthesia includes anesthesia of the major species: dogs, cats, horses, cattle, sheep, goats, and pigs, as well as all other animals requiring veterinary care such as birds, pocket pets, and wildlife.
Dental anesthesia is the application of anesthesia to dentistry. It includes local anesthetics, sedation, and general anesthesia.
While needle phobia is not age-specific, it is more common in children than in adults. The latest research from all fields indicates that needle-fear is predominant among children fears with some research claiming that up to 93% of children experience [needle-related] stress." Many studies have been performed investigating psychosocial methods of helping children cope with their fear. Current research in this area has investigated several types of non-invasive treatments to aid children in their needle phobia. These can be categorized into distraction techniques and other methods. These techniques offer safer, cheaper alternatives to drug or anesthetic treatments.

In medicine, sampling is gathering of matter from the body to aid in the process of a medical diagnosis and/or evaluation of an indication for treatment, further medical tests or other procedures. In this sense, the sample is the gathered matter, and the sampling tool or sampler is the person or material to collect the sample.
Suprapubic aspiration is a procedure to take a urine sample. It involves putting a needle through the skin just above the pubic bone into the bladder. It is typically used as a method to collect urine in child less than 2 years of age who is not yet toilet trained in an effort to diagnose a urinary tract infection.