Ozone is an inorganic molecule with the chemical formula O
3. It is a pale blue gas with a distinctively pungent smell. It is an allotrope of oxygen that is much less stable than the diatomic allotrope O
2, breaking down in the lower atmosphere to O
2 (dioxygen). Ozone is formed from dioxygen by the action of ultraviolet (UV) light and electrical discharges within the Earth's atmosphere. It is present in very low concentrations throughout the atmosphere, with its highest concentration high in the ozone layer of the stratosphere, which absorbs most of the Sun's ultraviolet (UV) radiation.

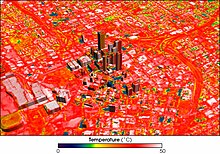
Urban areas usually experience the urban heat island (UHI) effect, that is, they are significantly warmer than surrounding rural areas. The temperature difference is usually larger at night than during the day, and is most apparent when winds are weak, under block conditions, noticeably during the summer and winter. The main cause of the UHI effect is from the modification of land surfaces while waste heat generated by energy usage is a secondary contributor. A study has shown that heat islands can be affected by proximity to different types of land cover, so that proximity to barren land causes urban land to become hotter and proximity to vegetation makes it cooler. As a population center grows, it tends to expand its area and increase its average temperature. The term heat island is also used; the term can be used to refer to any area that is relatively hotter than the surrounding, but generally refers to human-disturbed areas. Urban areas occupy about 0.5% of the Earth's land surface but host more than half of the world's population.

Extreme weather includes unexpected, unusual, severe, or unseasonal weather; weather at the extremes of the historical distribution—the range that has been seen in the past. Extreme events are based on a location's recorded weather history. They are defined as lying in the most unusual ten percent. The main types of extreme weather include heat waves, cold waves and heavy precipitation or storm events, such as tropical cyclones. The effects of extreme weather events are economic costs, loss of human lives, droughts, floods, landslides. Severe weather is a particular type of extreme weather which poses risks to life and property.

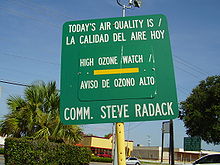
Ground-level ozone (O3), also known as surface-level ozone and tropospheric ozone, is a trace gas in the troposphere (the lowest level of the Earth's atmosphere), with an average concentration of 20–30 parts per billion by volume (ppbv), with close to 100 ppbv in polluted areas. Ozone is also an important constituent of the stratosphere, where the ozone layer (2 to 8 parts per million ozone) exists which is located between 10 and 50 kilometers above the Earth's surface. The troposphere extends from the ground up to a variable height of approximately 14 kilometers above sea level. Ozone is least concentrated in the ground layer (or planetary boundary layer) of the troposphere. Ground-level or tropospheric ozone is created by chemical reactions between NOx gases (oxides of nitrogen produced by combustion) and volatile organic compounds (VOCs). The combination of these chemicals in the presence of sunlight form ozone. Its concentration increases as height above sea level increases, with a maximum concentration at the tropopause. About 90% of total ozone in the atmosphere is in the stratosphere, and 10% is in the troposphere. Although tropospheric ozone is less concentrated than stratospheric ozone, it is of concern because of its health effects. Ozone in the troposphere is considered a greenhouse gas, and may contribute to global warming.

Indoor air quality (IAQ) is the air quality within buildings and structures. Poor indoor air quality due to indoor air pollution is known to affect the health, comfort, and well-being of building occupants. It has also been linked to sick building syndrome, respiratory issues, reduced productivity, and impaired learning in schools. Common pollutants of indoor air include: secondhand tobacco smoke, air pollutants from indoor combustion, radon, molds and other allergens, carbon monoxide, volatile organic compounds, legionella and other bacteria, asbestos fibers, carbon dioxide, ozone and particulates. Source control, filtration, and the use of ventilation to dilute contaminants are the primary methods for improving indoor air quality.

A heat wave, sometimes described as extreme heat, is a period of abnormally hot weather. Definitions vary but are similar. A heat wave is usually measured relative to the usual climate in the area and to normal temperatures for the season. Temperatures that humans from a hotter climate consider normal, can be regarded as a heat wave in a cooler area. This would be the case if the warm temperatures are outside the normal climate pattern for that area. High humidity often occurs during heat waves as well. This is especially the case in oceanic climate countries. Heat waves have become more frequent, and more intense over land, across almost every area on Earth since the 1950s. Heat waves occur from climate change.

Exhaust gas or flue gas is emitted as a result of the combustion of fuels such as natural gas, gasoline (petrol), diesel fuel, fuel oil, biodiesel blends, or coal. According to the type of engine, it is discharged into the atmosphere through an exhaust pipe, flue gas stack, or propelling nozzle. It often disperses downwind in a pattern called an exhaust plume.

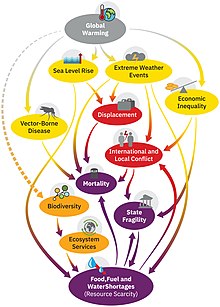
Human impact on the environment refers to changes to biophysical environments and to ecosystems, biodiversity, and natural resources caused directly or indirectly by humans. Modifying the environment to fit the needs of society is causing severe effects including global warming, environmental degradation, mass extinction and biodiversity loss, ecological crisis, and ecological collapse. Some human activities that cause damage to the environment on a global scale include population growth, neoliberal economic policies and rapid economic growth, overconsumption, overexploitation, pollution, and deforestation. Some of the problems, including global warming and biodiversity loss, have been proposed as representing catastrophic risks to the survival of the human species.

Effects of climate change are well documented and growing for Earth's natural environment and human societies. Changes to the climate system include an overall warming trend, changes to precipitation patterns, and more extreme weather. As the climate changes it impacts the natural environment with effects such as more intense forest fires, thawing permafrost, and desertification. These changes impact ecosystems and societies, and can become irreversible once tipping points are crossed.

African environmental issues are caused by human impacts on the natural environment and affect humans and nearly all forms of life. Issues include deforestation, soil degradation, air pollution, water pollution, garbage pollution, climate change and water scarcity. These issues result in environmental conflict and are connected to broader social struggles for democracy and sovereignty.

Air pollution is the contamination of air due to the presence of substances called pollutants in the atmosphere that are harmful to the health of humans and other living beings, or cause damage to the climate or to materials. It is also the contamination of the indoor or outdoor environment either by chemical, physical, or biological agents that alters the natural features of the atmosphere. There are many different types of air pollutants, such as gases, particulates, and biological molecules. Air pollution can cause diseases, allergies, and even death to humans; it can also cause harm to other living organisms such as animals and crops, and may damage the natural environment or built environment. Air pollution can be caused by both human activities and natural phenomena.

Climate change in California has resulted in higher than average temperatures, leading to increased occurrences of drought and wildfires. During the next few decades in California, climate change is likely to further reduce water availability, increase wildfire risk, decrease agricultural productivity, and threaten coastal ecosystems. The state will also be impacted economically due to the rising cost of providing water to its residents along with revenue and job loss in the agricultural sector. California has taken a number of steps to mitigate impacts of climate change in the state.

Particulates or atmospheric particulate matter are microscopic particles of solid or liquid matter suspended in the air. The term aerosol commonly refers to the particulate/air mixture, as opposed to the particulate matter alone. Sources of particulate matter can be natural or anthropogenic. They have impacts on climate and precipitation that adversely affect human health, in ways additional to direct inhalation.

There are numerous effects of climate change on agriculture, many of which are making it harder for agricultural activities to provide global food security. Rising temperatures and changing weather patterns often result in lower crop yields due to water scarcity caused by drought, heat waves and flooding. These effects of climate change can also increase the risk of several regions suffering simultaneous crop failures. Currently this risk is regarded as rare but if these simultaneous crop failures did happen they would have significant consequences for the global food supply. Many pests and plant diseases are also expected to either become more prevalent or to spread to new regions. The world's livestock are also expected to be affected by many of the same issues, from greater heat stress to animal feed shortfalls and the spread of parasites and vector-borne diseases.

The effects of climate change on mental health and wellbeing are documented. This is especially the case for vulnerable populations and those with pre-existing serious mental illness. There are three broad pathways by which these effects can take place: directly, indirectly or via awareness. The direct pathway includes stress-related conditions caused by exposure to extreme weather events. These include post-traumatic stress disorder (PTSD). Scientific studies have linked mental health to several climate-related exposures. These include heat, humidity, rainfall, drought, wildfires and floods. The indirect pathway can be disruption to economic and social activities. An example is when an area of farmland is less able to produce food. The third pathway can be of mere awareness of the climate change threat, even by individuals who are not otherwise affected by it.
Environmental health policy is governmental action intended to prevent exposure to environmental hazards or "eliminate the effects of exposure to environmental hazards".

Global climate change has increased the occurrence of some infectious diseases. Infectious diseases whose transmission is impacted by climate change include, for example, vector-borne diseases like dengue fever, malaria, tick-borne diseases, leishmaniasis, zika fever, chikungunya and Ebola. One mechanism contributing to increased disease transmission is that climate change is altering the geographic range and seasonality of the insects that can carry the diseases. Scientists stated a clear observation in 2022: "the occurrence of climate-related food-borne and waterborne diseases has increased ."

Children are more vulnerable to the effects of climate change than adults. The World Health Organization estimated that 88% of the existing global burden of disease caused by climate change affects children under five years of age. A Lancet review on health and climate change lists children as the worst-affected category by climate change. Children under 14 are 44 percent more likely to die from environmental factors, and those in urban areas are disproportionately impacted by lower air quality and overcrowding.

Triple Planetary Crisis is a term and framework adopted by the United Nations system to describe the three intersecting global environmental crises of pollution, climate crisis, biodiversity loss and/or ecological crises. This term underscores the interdependence of these issues and their collective impact on the planet's ecosystems, societies, and economies.