Related Research Articles

A nurse practitioner (NP) is an advanced practice registered nurse and a type of mid-level practitioner. NPs are trained to assess patient needs, order and interpret diagnostic and laboratory tests, diagnose disease, formulate and prescribe medications and treatment plans. NP training covers basic disease prevention, coordination of care, and health promotion, but does not provide the depth of expertise needed to recognize more complex conditions.

Taiwan's epidemic of HIV/AIDS began with the first case reported in December 1984. On 17 December 1990 the government promulgated the AIDS Prevention and Control Act. On 11 July 2007, the AIDS Prevention and Control Act was renamed the HIV Infection Control and Patient Rights Protection Act.

In response to the Millennium Development Goals' focus on maternal and child health, the Philippines began the National Demographic and Health Survey in 1968 to assess the effectiveness of public health programs in the country.

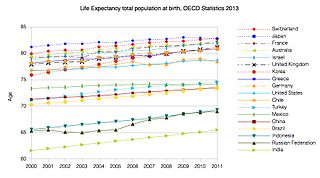
Healthcare in Taiwan is administered by the Ministry of Health and Welfare of the Executive Yuan. As with other developed economies, Taiwanese people are well-nourished but face such health problems as chronic obesity and heart disease. In 2002 Taiwan had nearly 1.6 physicians and 5.9 hospital beds per 1,000 population. In 2002, there were 36 hospitals and 2,601 clinics in the country. Per capita health expenditures totaled US$752 in 2000. Health expenditures constituted 5.8 percent of the gross domestic product (GDP) in 2001 ; 64.9 percent of the expenditures were from public funds. Overall life expectancy in 2019 was averaged at 81 years.
Healthcare in Finland consists of a highly decentralized three-level publicly funded healthcare system and a much smaller private sector. Although the Ministry of Social Affairs and Health has the highest decision-making authority, the municipalities are responsible for providing healthcare to their residents.

A hospital is a health care institution providing patient treatment with specialized health science and auxiliary healthcare staff and medical equipment. The best-known type of hospital is the general hospital, which typically has an emergency department to treat urgent health problems ranging from fire and accident victims to a sudden illness. A district hospital typically is the major health care facility in its region, with many beds for intensive care and additional beds for patients who need long-term care. Specialized hospitals include trauma centers, rehabilitation hospitals, children's hospitals, seniors' (geriatric) hospitals, and hospitals for dealing with specific medical needs such as psychiatric treatment and certain disease categories. Specialized hospitals can help reduce health care costs compared to general hospitals. Hospitals are classified as general, specialty, or government depending on the sources of income received.
Kenya's health care system is structured in a step-wise manner so that complicated cases are referred to a higher level. Gaps in the system are filled by private and church run units.
In South Africa, private and public health systems exist in parallel. The public system serves the vast majority of the population. Authority and service delivery are divided between the national Department of Health, provincial health departments, and municipal health departments.
Healthcare in Georgia is provided by a universal health care system under which the state funds medical treatment in a mainly privatized system of medical facilities. In 2013, the enactment of a universal health care program triggered universal coverage of government-sponsored medical care of the population and improving access to health care services. Responsibility for purchasing publicly financed health services lies with the Social Service Agency (SSA).
Healthcare in Denmark is largely provided by the local governments of the five regions, with coordination and regulation by central government, while nursing homes, home care, and school health services are the responsibility of the 98 municipalities. Some specialised hospital services are managed centrally.

Tanzania has a hierarchical health system which is in tandem with the political-administrative hierarchy. At the bottom, there are the dispensaries found in every village where the village leaders have a direct influence on its running. The health centers are found at ward level and the health center in charge is answerable to the ward leaders. At the district, there is a district hospital and at the regional level a regional referral hospital. The tertiary level is usually the zone hospitals and at a national level, there is the national hospital. There are also some specialized hospitals that do not fit directly into this hierarchy and therefore are directly linked to the ministry of health.
Healthcare in the United States is far outspent than any other nation, measured both in per capita spending and as a percentage of GDP. Despite this, the country has significantly worse healthcare outcomes when compared to peer nations. The US is the only developed nation without a system of universal healthcare, with a large proportion of its population not carrying health insurance, a substantial factor in the country's excess mortality.

North Korea has a life expectancy of 72 years as of 2020. While North Korea is classified as a low-income country, the structure of North Korea's causes of death (2013) is unlike that of other low-income countries. Instead, it is closer to the worldwide averages, with non-communicable diseases – such as cardiovascular disease – accounting for two-thirds of the total deaths.
In Norway, municipalities are in charge of providing basic healthcare. Since the money given to municipalities is not set aside for any particular purpose, each municipality is free to determine its own health budget. Municipalities coordinate primary healthcare services through agreements with independent physicians. In Norway, private healthcare providers are not compensated unless they have a contract with the public health service.

Healthcare in Belgium is composed of three parts. Firstly there is a primarily publicly funded healthcare and social security service run by the federal government, which organises and regulates healthcare; independent private/public practitioners, university/semi-private hospitals and care institutions. There are a few private hospitals. Secondly is the insurance coverage provided for patients. Finally, industry coverage; which covers the production and distribution of healthcare products for research and development. The primary aspect of this research is done in universities and hospitals.
This article provides a brief overview of the health care systems of the world, sorted by continent.

Lesotho's Human development index value for 2018 was 0.518—which put the country in the low human development category—positioning it at 164 out of 189 countries and territories. Health care services in Lesotho are delivered primarily by the government and the Christian Health Association of Lesotho. Access to health services is difficult for many people, especially in rural areas. The country's health system is challenged by the relentless increase of the burden of disease brought about by AIDS, and a lack of expertise and human resources. Serious emergencies are often referred to neighbouring South Africa. The largest contribution to mortality in Lesotho are communicable diseases, maternal, perinatal and nutritional conditions.

Healthcare in Belize is provided through both public and private healthcare systems. The Ministry of Health (MoH) is the government agency responsible for overseeing the entire health sector and is also the largest provider of public health services in Belize. The MoH offers affordable care to a majority of Belizeans with a strong focus on providing quality healthcare through a range of public programs and institutions.

Healthcare in Rwanda was historically of poor quality, but in recent decades has seen great improvement. Rwanda operates a universal health care system, and is considered to have one of the highest-quality health systems in Africa.
References
- ↑ "Healthcare in the Bahamas". InterNations. 2018. Retrieved 15 November 2018.
- ↑ "NHI Bahamas |" . Retrieved 2021-03-04.
- ↑ "Health". Lonely Planet. 2018. Retrieved 15 November 2018.
- ↑ "National Health Insurance A Shared Responsibility" (PDF). NHI Bahamas. 2018. Retrieved 15 November 2018.
- ↑ "NHI consultation period with stakeholders extended". EyeWiness News. 15 November 2018. Retrieved 15 November 2018.
- ↑ "Bahamas needs 528 nurses". Nassau Guardian. 27 February 2018. Retrieved 5 December 2018.