Vaccination is the administration of a vaccine to help the immune system develop immunity from a disease. Vaccines contain a microorganism or virus in a weakened, live or killed state, or proteins or toxins from the organism. In stimulating the body's adaptive immunity, they help prevent sickness from an infectious disease. When a sufficiently large percentage of a population has been vaccinated, herd immunity results. Herd immunity protects those who may be immunocompromised and cannot get a vaccine because even a weakened version would harm them. The effectiveness of vaccination has been widely studied and verified. Vaccination is the most effective method of preventing infectious diseases; widespread immunity due to vaccination is largely responsible for the worldwide eradication of smallpox and the elimination of diseases such as polio and tetanus from much of the world. However, some diseases, such as measles outbreaks in America, have seen rising cases due to relatively low vaccination rates in the 2010s – attributed, in part, to vaccine hesitancy. According to the World Health Organization, vaccination prevents 3.5–5 million deaths per year.

Measles is a highly contagious, vaccine-preventable infectious disease caused by measles virus. Symptoms usually develop 10–12 days after exposure to an infected person and last 7–10 days. Initial symptoms typically include fever, often greater than 40 °C (104 °F), cough, runny nose, and inflamed eyes. Small white spots known as Koplik's spots may form inside the mouth two or three days after the start of symptoms. A red, flat rash which usually starts on the face and then spreads to the rest of the body typically begins three to five days after the start of symptoms. Common complications include diarrhea, middle ear infection (7%), and pneumonia (6%). These occur in part due to measles-induced immunosuppression. Less commonly seizures, blindness, or inflammation of the brain may occur. Other names include morbilli, rubeola, red measles, and English measles. Both rubella, also known as German measles, and roseola are different diseases caused by unrelated viruses.

Diphtheria is an infection caused by the bacterium Corynebacterium diphtheriae. Most infections are asymptomatic or have a mild clinical course, but in some outbreaks, the mortality rate approaches 10%. Signs and symptoms may vary from mild to severe, and usually start two to five days after exposure. Symptoms often develop gradually, beginning with a sore throat and fever. In severe cases, a grey or white patch develops in the throat, which can block the airway, and create a barking cough similar to what is observed in croup. The neck may also swell in part due to the enlargement of the facial lymph nodes. Diphtheria can also involve the skin, eyes, or genitals, and can cause complications, including myocarditis, inflammation of nerves, kidney problems, and bleeding problems due to low levels of platelets.

The MMR vaccine is a vaccine against measles, mumps, and rubella, abbreviated as MMR. The first dose is generally given to children around 9 months to 15 months of age, with a second dose at 15 months to 6 years of age, with at least four weeks between the doses. After two doses, 97% of people are protected against measles, 88% against mumps, and at least 97% against rubella. The vaccine is also recommended for those who do not have evidence of immunity, those with well-controlled HIV/AIDS, and within 72 hours of exposure to measles among those who are incompletely immunized. It is given by injection.

Whooping cough, also known as pertussis or the 100-day cough, is a highly contagious, vaccine-preventable bacterial disease. Initial symptoms are usually similar to those of the common cold with a runny nose, fever, and mild cough, but these are followed by two or three months of severe coughing fits. Following a fit of coughing, a high-pitched whoop sound or gasp may occur as the person breathes in. The violent coughing may last for 10 or more weeks, hence the phrase "100-day cough". The cough may be so hard that it causes vomiting, rib fractures, and fatigue. Children less than one year old may have little or no cough and instead have periods where they cannot breathe. The incubation period is usually seven to ten days. Disease may occur in those who have been vaccinated, but symptoms are typically milder.

Vaccine hesitancy is a delay in acceptance, or refusal, of vaccines despite the availability of vaccine services and supporting evidence. The term covers refusals to vaccinate, delaying vaccines, accepting vaccines but remaining uncertain about their use, or using certain vaccines but not others. The scientific consensus that vaccines are generally safe and effective is overwhelming. Vaccine hesitancy often results in disease outbreaks and deaths from vaccine-preventable diseases. Therefore, the World Health Organization characterizes vaccine hesitancy as one of the top ten global health threats.

Flu season is an annually recurring time period characterized by the prevalence of an outbreak of influenza (flu). The season occurs during the cold half of the year in each hemisphere. It takes approximately two days to show symptoms. Influenza activity can sometimes be predicted and even tracked geographically. While the beginning of major flu activity in each season varies by location, in any specific location these minor epidemics usually take about three weeks to reach its pinnacle, and another three weeks to significantly diminish.

Meningococcal disease describes infections caused by the bacterium Neisseria meningitidis. It has a high mortality rate if untreated but is vaccine-preventable. While best known as a cause of meningitis, it can also result in sepsis, which is an even more damaging and dangerous condition. Meningitis and meningococcemia are major causes of illness, death, and disability in both developed and under-developed countries.
Vaccination and religion have interrelations of varying kinds. No major religion prohibits vaccinations, and some consider it an obligation because of the potential to save lives. However, some people cite religious adherence as a basis for opting to forego vaccinating themselves or their children. Many such objections are pretextual: in Australia, anti-vaccinationists founded the Church of Conscious Living, a "fake church", leading to religious exemptions being removed in that country, and one US pastor was reported to offer vaccine exemptions in exchange for online membership of his church.
The National Center for Immunization and Respiratory Diseases (NCIRD), formerly known as the National Immunization Program until April 2006, is charged with responsibility for the planning, coordination, and conduct of immunization activities in the United States. NCIRD is a part of the Centers for Disease Control and Prevention, located in Atlanta, Georgia, and housed in the CDC's Coordinating Center for Infectious Diseases (CCID). The National Center for Immunization provides consultation, training, statistical, promotional, educational, epidemiological, and technical services to assist state and local health departments across the US in planning, developing, contracting and implementing immunization programs.
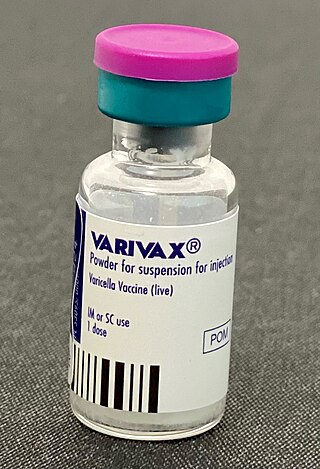
Varicella vaccine, also known as chickenpox vaccine, is a vaccine that protects against chickenpox. One dose of vaccine prevents 95% of moderate disease and 100% of severe disease. Two doses of vaccine are more effective than one. If given to those who are not immune within five days of exposure to chickenpox it prevents most cases of disease. Vaccinating a large portion of the population also protects those who are not vaccinated. It is given by injection just under the skin. Another vaccine, known as zoster vaccine, is used to prevent diseases caused by the same virus – the varicella zoster virus.
A vaccination policy is a health policy adopted in order to prevent the spread of infectious disease. These policies are generally put into place by State or local governments, but may also be set by private facilities, such as workplaces or schools. Many policies have been developed and implemented since vaccines were first made widely available.

Measles vaccine protects against becoming infected with measles. Nearly all of those who do not develop immunity after a single dose develop it after a second dose. When the rate of vaccination within a population is greater than 92%, outbreaks of measles typically no longer occur; however, they may occur again if the rate of vaccination decreases. The vaccine's effectiveness lasts many years. It is unclear if it becomes less effective over time. The vaccine may also protect against measles if given within a couple of days after exposure to measles.

Yellow fever vaccine is a vaccine that protects against yellow fever. Yellow fever is a viral infection that occurs in Africa and South America. Most people begin to develop immunity within ten days of vaccination and 99% are protected within one month, and this appears to be lifelong. The vaccine can be used to control outbreaks of disease. It is given either by injection into a muscle or just under the skin.

In 1976, an outbreak of the swine flu, influenza A virus subtype H1N1 at Fort Dix, New Jersey caused one death, hospitalized 13, and led to a mass immunization program. After the program began, the vaccine was associated with an increase in reports of Guillain–Barré syndrome (GBS), which can cause paralysis, respiratory arrest, and death. The immunization program was ended after approximately 43 millions United States citizens had been administered the vaccine.

The Vaccines for Children Program (VFC) is a federally funded program in the United States providing no-cost vaccines to children who lack health insurance or who otherwise cannot afford the cost of the vaccination. The VFC program was created by the Omnibus Budget Reconciliation Act of 1993 and is required to be a new entitlement of each state's Medicaid plan under section 1928 of the Social Security Act. The program was officially implemented in October 1994 and serves eligible children in all U.S. states, as well as the Commonwealth of Puerto Rico, the U.S. Virgin Islands, American Samoa, Guam, and the Commonwealth of the Northern Mariana Islands.
California Senate Bill 277 (SB277) is a California law that removed personal belief as a reason for an exemption from the vaccination requirements for entry to private or public elementary or secondary schools in California, as well as day care centers. The final version of the bill was enacted by the California Legislature in 2015 and was signed into law by Governor Jerry Brown on June 30, 2015.
In early months of 2019, a measles outbreak occurred in the Portland metropolitan area, including the Clark County, Washington suburbs, in the United States. At the time, the outbreak was the largest outbreak in more than two decades; outbreaks in 2019 in areas including Brooklyn and Rockland County, New York have since seen far greater numbers of cases.

Measles was declared eliminated from the United States in 2000 by the World Health Organization due to the success of vaccination efforts. However, it continues to be reintroduced by international travelers, and in recent years, anti-vaccination sentiment has allowed for the reemergence of measles outbreaks.

Vaccination policy of the United States is the subset of U.S. federal health policy that deals with immunization against infectious disease. It is decided at various levels of the government, including the individual states. This policy has been developed over the approximately two centuries since the invention of vaccination with the purpose of eradicating disease from the U.S. population, or creating a herd immunity. Policies intended to encourage vaccination impact numerous areas of law, including regulation of vaccine safety, funding of vaccination programs, vaccine mandates, adverse event reporting requirements, and compensation for injuries asserted to be associated with vaccination.