Neurological deficits

Alcoholics can typically be divided into two categories, uncomplicated and complicated. [3] Uncomplicated alcoholics do not have nutritional deficiency states or liver disease, but have a reduction in overall brain volume due to white matter cerebral atrophy. The severity of atrophy sustained from alcohol consumption is proportional to the rate and amount of alcohol consumed during a person's life. [7] Complicated alcoholics may have liver damage that impacts brain structure and function and nutritional deficiencies "that can cause severe brain damage and dysfunction". [3] [7]
Pathophysiology
Adolescents are much more vulnerable to alcohol-related brain damage in the form of persistent changes in neuroimmune signalling from binge drinking. [8] The endocrine system includes the hypothalamic–pituitary–adrenal axis, the hypothalamic–pituitary–gonadal axis, the hypothalamic–pituitary–thyroid axis, the hypothalamic–pituitary–growth hormone/insulin-like growth factor-1 axis, and the hypothalamic–posterior pituitary axis, as well as other sources of hormones, such as the endocrine pancreas and endocrine adipose tissue. Alcohol abuse disrupts all of these systems and causes hormonal disturbances that may result in various disorders, such as stress intolerance, reproductive dysfunction, thyroid problems, immune abnormalities, and psychological and behavioral disorders. [9]
The cerebral atrophy that alcoholics often present with is due to alcohol induced neurotoxicity. [6] [10] Evidence of neurodegeneration can be supported by an increased microglia density and expression of proinflammatory cytokines in the brain. Animal studies find that heavy and regular binge drinking causes neurodegeneration in corticolimbic brain regions areas which are involved in learning and spatial memory. The corticolimbic brain regions affected include the olfactory bulb, piriform cortex, perirhinal cortex, entorhinal cortex, and the hippocampal dentate gyrus. It was found that a heavy two-day drinking binge caused extensive neurodegeneration in the entorhinal cortex with resultant learning deficits in rats. [5]
It is unclear how the frequency and length of these binge drinking sessions impacts brain damage in humans. Humans who drank at least 100 drinks (male) or 80 drinks (female) per month (concentrated to 21 occasions or less per month) throughout a three-year period had impaired decision-making skills compared to non-binge drinkers. [5] An MRI brain scan found that levels of N-acetylaspartate (NAA), a metabolite biomarker for neural integrity, was lower in binge drinkers. Additionally, abnormal brain metabolism, a loss of white brain matter in the frontal lobe, and higher parietal gray matter NAA levels were found. This shows a correlation between binge drinking, poor executive functioning, and working memory. A decrease in frontal lobe NAA levels is associated with impaired executive functioning and processing speed in neuro-performance tests. [5]
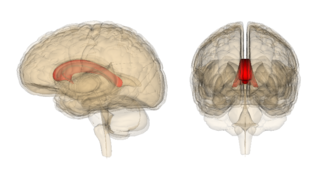
The volume of the corpus callosum, a large white matter tract that connects the two cerebral hemispheres, is shown to decrease with alcohol abuse due to a loss of myelination. This integration between the two cerebral hemispheres and cognitive function is affected. A limited amount of myelin can be restored with alcohol abstinence, leading to transient neurological deficits. [7]
Alcohol abuse affects neurons in the frontal cortex that typically have a large soma, or cell body. This type of neuron is more susceptible to Alzheimer's disease and normal aging. Research is still being conducted to determine whether there is a direct link between excessive alcohol consumption and Alzheimer's disease. [7]
Higher order functioning of the cerebral cortex is organized by the cerebellum. In those with cerebral atrophy, Purkinje cells, or the cerebellar output neurons, in the vermis are reduced in number by 43%. [7] This large reduction in Purkinje cells causes a decrease in high order cerebral cortex organization. The cerebellum is also responsible for refining crude motor output from the primary motor cortex. When this refinement is missing, symptoms such as unsteadiness and ataxia [7] will present. A potential cause of chronic alcoholic cerebellar dysfunction is an alteration of GABA-A receptor. This dysfunction causes an increase in the neurotransmitter GABA in cerebellar Purkinje cells, granule cells, and interneurons leading to a disruption in normal cell signaling. [7]

Kindling and excitotoxicity
Binge drinkers and alcoholics who go through multiple detoxifications show prefrontal cortex dysfunction, as it is known that alcohol has long-term effects on prefrontal cortex function, leading to impairments in executive control tasks. Animal studies show that repeated alcohol withdrawals are associated with a significantly impaired ability to learn new information. [11] Alcohol's acute effects on GABAergic enhancement and NMDA suppression cause alcohol induced neurotoxicity and kindling, or worsening of alcohol withdrawal symptoms with each subsequent withdrawal period. This may cause CNS depression leading to acute tolerance to these withdrawal effects. This tolerance is followed by a damaging rebound effect during withdrawal. This rebound causes hyperexcitability of neurotransmission systems. If this hyperexcitability state occurs multiple times, kindling and neurotoxicity can occur leading to increased alcohol-related brain damage. Damaging excitotoxicity may also occur as a result of repeated withdrawals. Similar to people who have gone through multiple detoxifications, binge drinkers show a higher rate of emotional disturbance due to these damaging effects. [11]
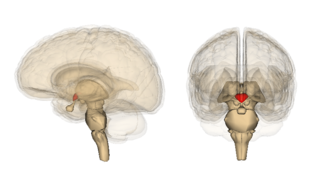
Thiamine deficiency
Thiamine is a vitamin your body needs for growth, development, and cellular function, as well as converting food into energy. Thiamine is naturally present in some foods, added to some food products, and available as a dietary supplement. [12] A nutritional deficiency in thiamine can worsen alcohol-related brain damage. There is a genetic component to thiamine deficiency that causes intestinal malabsorption. [13] A nutritional vitamin deficiency state that is caused by thiamine deficiency which is seen most commonly in alcoholics leads to Wernicke's encephalopathy and Alcoholic Korsakoff syndrome (AKS) which frequently occur simultaneously, known as Wernicke–Korsakoff syndrome (WKS). This disorder is preventable through supplementation of the diet by thiamine and an awareness by health professionals to treat 'at risk' patients with thiamine. [13] Thiamine deficiency may occur in upwards of 80% of patients with alcoholism however, only ≈13% of such individuals develop WKS, raising the possibility that a genetic predisposition to WKS may exist in some individuals. [14] [15] Lesions, or brain abnormalities, are typically located in the diencephalon which result in anterograde and retrograde amnesia, or memory loss. [15]