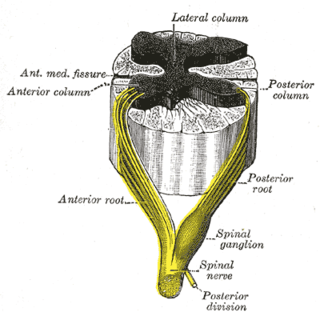
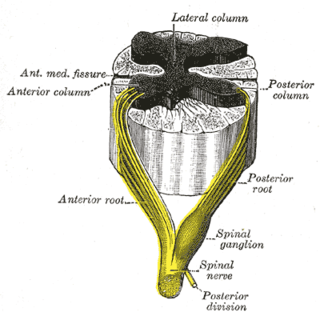
The somatic nervous system (SNS) is made up of nerves that link the brain and spinal cord to voluntary or skeletal muscles that are under conscious control as well as to skin sensory receptors. Specialized nerve fiber ends called sensory receptors are responsible for detecting information within and outside of the body.
Paresthesia is an abnormal sensation of the skin with no apparent physical cause. Paresthesia may be transient or chronic, and may have many possible underlying causes. Paresthesias are usually painless and can occur anywhere on the body, but most commonly occur in the arms and legs.
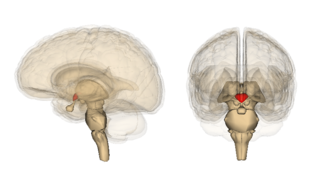
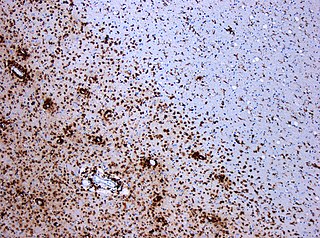
Wernicke encephalopathy (WE), also Wernicke's encephalopathy, or wet brain is the presence of neurological symptoms caused by biochemical lesions of the central nervous system after exhaustion of B-vitamin reserves, in particular thiamine (vitamin B1). The condition is part of a larger group of thiamine deficiency disorders that includes beriberi, in all its forms, and alcoholic Korsakoff syndrome. When it occurs simultaneously with alcoholic Korsakoff syndrome it is known as Wernicke–Korsakoff syndrome.
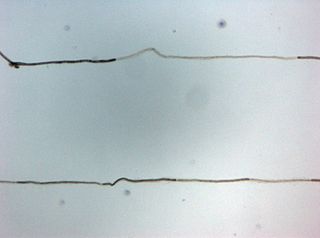
Peripheral neuropathy, often shortened to neuropathy, refers to damage or disease affecting the nerves. Damage to nerves may impair sensation, movement, gland function, and/or organ function depending on which nerves are affected. Neuropathies affecting motor, sensory, or autonomic nerves result in different symptoms. More than one type of nerve may be affected simultaneously. Peripheral neuropathy may be acute or chronic, and may be reversible or permanent.
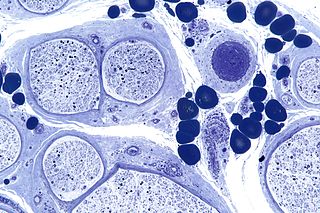
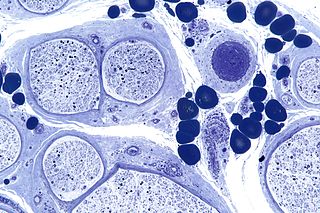
A demyelinating disease refers to any disease affecting the nervous system where the myelin sheath surrounding neurons is damaged. This damage disrupts the transmission of signals through the affected nerves, resulting in a decrease in their conduction ability. Consequently, this reduction in conduction can lead to deficiencies in sensation, movement, cognition, or other functions depending on the nerves affected.

Polyneuropathy is damage or disease affecting peripheral nerves in roughly the same areas on both sides of the body, featuring weakness, numbness, and burning pain. It usually begins in the hands and feet and may progress to the arms and legs and sometimes to other parts of the body where it may affect the autonomic nervous system. It may be acute or chronic. A number of different disorders may cause polyneuropathy, including diabetes and some types of Guillain–Barré syndrome.

Neuritis, from the Greek νεῦρον), is inflammation of a nerve or the general inflammation of the peripheral nervous system. Inflammation, and frequently concomitant demyelination, cause impaired transmission of neural signals and leads to aberrant nerve function. Neuritis is often conflated with neuropathy, a broad term describing any disease process which affects the peripheral nervous system. However, neuropathies may be due to either inflammatory or non-inflammatory causes, and the term encompasses any form of damage, degeneration, or dysfunction, while neuritis refers specifically to the inflammatory process.
Chronic inflammatory demyelinating polyneuropathy (CIDP) is an acquired autoimmune disease of the peripheral nervous system characterized by progressive weakness and impaired sensory function in the legs and arms. The disorder is sometimes called chronic relapsing polyneuropathy (CRP) or chronic inflammatory demyelinating polyradiculoneuropathy. CIDP is closely related to Guillain–Barré syndrome and it is considered the chronic counterpart of that acute disease. Its symptoms are also similar to progressive inflammatory neuropathy. It is one of several types of neuropathy.
Toxic and nutritional optic neuropathy is a group of medical disorders defined by visual impairment due to optic nerve damage secondary to a toxic substance and/or nutritional deficiency. The causes of these disorders are various, but they are linked by shared signs and symptoms, which this article will describe. In several of these disorders, both toxic and nutritional factors play a role, acting synergistically.

Thiamine deficiency is a medical condition of low levels of thiamine (vitamin B1). A severe and chronic form is known as beriberi. The two main types in adults are wet beriberi and dry beriberi. Wet beriberi affects the cardiovascular system, resulting in a fast heart rate, shortness of breath, and leg swelling. Dry beriberi affects the nervous system, resulting in numbness of the hands and feet, confusion, trouble moving the legs, and pain. A form with loss of appetite and constipation may also occur. Another type, acute beriberi, found mostly in babies, presents with loss of appetite, vomiting, lactic acidosis, changes in heart rate, and enlargement of the heart.

Alcoholic cardiomyopathy (ACM) is a disease in which the long-term consumption of alcohol leads to heart failure. ACM is a type of dilated cardiomyopathy. The heart is unable to pump blood efficiently, leading to heart failure. It can affect other parts of the body if the heart failure is severe. It is most common in males between the ages of 35 and 50.

Hereditary neuropathy with liability to pressure palsy (HNPP) is a peripheral neuropathy, a condition that affects the nerves. Pressure on the nerves can cause tingling sensations, numbness, pain, weakness, muscle atrophy and even paralysis of the affected area. In normal individuals, these symptoms disappear quickly, but in sufferers of HNPP even a short period of pressure can cause the symptoms to occur. Palsies can last from minutes or days to weeks or even months.

Nutritional neuroscience is the scientific discipline that studies the effects various components of the diet such as minerals, vitamins, protein, carbohydrates, fats, dietary supplements, synthetic hormones, and food additives have on neurochemistry, neurobiology, behavior, and cognition.
Anti-MAG peripheral neuropathy is a specific type of peripheral neuropathy in which the person's own immune system attacks cells that are specific in maintaining a healthy nervous system. As these cells are destroyed by antibodies, the nerve cells in the surrounding region begin to lose function and create many problems in both sensory and motor function. Specifically, antibodies against myelin-associated glycoprotein (MAG) damage Schwann cells. While the disorder occurs in only 10% of those afflicted with peripheral neuropathy, people afflicted have symptoms such as muscle weakness, sensory problems, and other motor deficits usually starting in the form of a tremor of the hands or trouble walking. There are, however, multiple treatments that range from simple exercises in order to build strength to targeted drug treatments that have been shown to improve function in people with this type of peripheral neuropathy.
Mitohondrial optic neuropathies are a heterogenous group of disorders that present with visual disturbances resultant from mitochondrial dysfunction within the anatomy of the Retinal Ganglion Cells (RGC), optic nerve, optic chiasm, and optic tract. These disturbances are multifactorial, their aetiology consisting of metabolic and/or structural damage as a consequence of genetic mutations, environmental stressors, or both. The three most common neuro-ophthalmic abnormalities seen in mitochondrial disorders are bilateral optic neuropathy, ophthalmoplegia with ptosis, and pigmentary retinopathy.
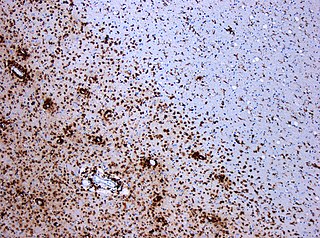
Alcohol-related brain damage alters both the structure and function of the brain as a result of the direct neurotoxic effects of alcohol intoxication or acute alcohol withdrawal. Increased alcohol intake is associated with damage to brain regions including the frontal lobe, limbic system, and cerebellum, with widespread cerebral atrophy, or brain shrinkage caused by neuron degeneration. This damage can be seen on neuroimaging scans.

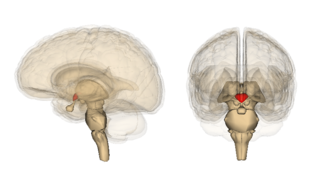
Cerebellar degeneration is a condition in which cerebellar cells, otherwise known as neurons, become damaged and progressively weaken in the cerebellum. There are two types of cerebellar degeneration; paraneoplastic cerebellar degeneration, and alcoholic or nutritional cerebellar degeneration. As the cerebellum contributes to the coordination and regulation of motor activities, as well as controlling equilibrium of the human body, any degeneration to this part of the organ can be life-threatening. Cerebellar degeneration can result in disorders in fine movement, posture, and motor learning in humans, due to a disturbance of the vestibular system. This condition may not only cause cerebellar damage on a temporary or permanent basis, but can also affect other tissues of the central nervous system, those including the cerebral cortex, spinal cord and the brainstem.
Peripheral mononeuropathy is a nerve related disease where a single nerve, that is used to transport messages from the brain to the peripheral body, is diseased or damaged. Peripheral neuropathy is a general term that indicates any disorder of the peripheral nervous system. The name of the disorder itself can be broken down in order to understand this better; peripheral: in regard to peripheral neuropathy, refers to outside of the brain and spinal cord; neuro: means nerve related; -pathy; means disease. Peripheral mononeuropathy is a disorder that links to Peripheral Neuropathy, as it only effects a single peripheral nerve rather than several damaged or diseased nerves throughout the body. Healthy peripheral nerves are able to “carry messages from the brain and spinal cord to muscles, organs, and other body tissues”.
Megavitamin-B6 syndrome is a collection of symptoms that can result from chronic supplementation, or acute overdose, of vitamin B6. While it is also known as hypervitaminosis B6, vitamin B6 toxicity and vitamin B6 excess, megavitamin-b6 syndrome is the name used in the ICD-10.
Sensory neuronopathy is a type of peripheral neuropathy that results primarily in sensory symptoms due to destruction of nerve cell bodies in the dorsal root ganglion. The causes of nerve damage are grouped into categories including those due to paraneoplastic causes, immune mediated, infectious, inherited or degenerative causes and those due to toxin exposure. In idiopathic sensory neuronopathy no cause is identified. Idiopathic causes account for about 50% of cases. Sensory neuronopathy differs from the more common length dependent axonal polyneuropathies in that the symptoms do not progress in a distal to proximal pattern, rather symptoms develop in a multifocal, asymmetric, and non-length dependent manner. Ataxia is a prominent symptom early in the disease course. The trigeminal nerve ganglion is also commonly affected leading to facial numbness. Motor nerves are usually not affected however some cases do have mild motor involvement in the form of weakness. Symptoms tend to develop sub-acutely, over weeks, in acquired sensory neuronopathy and more slowly in inherited or primary degenerative cases. In cases of paraneoplastic or infectious sensory neuropathy, treatment is directed at the underlying cancer or infectious cause respectively. Immunomodulatory and anti-inflammatory therapies are also commonly used however their effectiveness is limited.