Allergies, also known as allergic diseases, are various conditions caused by hypersensitivity of the immune system to typically harmless substances in the environment. These diseases include hay fever, food allergies, atopic dermatitis, allergic asthma, and anaphylaxis. Symptoms may include red eyes, an itchy rash, sneezing, coughing, a runny nose, shortness of breath, or swelling. Note that food intolerances and food poisoning are separate conditions.
An allergen is a type of antigen that produces an abnormally vigorous immune response in which the immune system fights off a perceived threat that would otherwise be harmless to the body. Such reactions are called allergies.

Anaphylaxis is a serious, potentially fatal allergic reaction and medical emergency that is rapid in onset and requires immediate medical attention regardless of use of emergency medication on site. It typically causes more than one of the following: an itchy rash, throat closing due to swelling that can obstruct or stop breathing; severe tongue swelling that can also interfere with or stop breathing; shortness of breath, vomiting, lightheadedness, loss of consciousness, low blood pressure, and medical shock. These symptoms typically start in minutes to hours and then increase very rapidly to life-threatening levels. Urgent medical treatment is required to prevent serious harm and death, even if the patient has used an epipen or has taken other medications in response, and even if symptoms appear to be improving.

Allergic rhinitis, of which the seasonal type is called hay fever, is a type of inflammation in the nose that occurs when the immune system overreacts to allergens in the air. Signs and symptoms include a runny or stuffy nose, sneezing, red, itchy, and watery eyes, and swelling around the eyes. The fluid from the nose is usually clear. Symptom onset is often within minutes following allergen exposure, and can affect sleep and the ability to work or study. Some people may develop symptoms only during specific times of the year, often as a result of pollen exposure. Many people with allergic rhinitis also have asthma, allergic conjunctivitis, or atopic dermatitis.
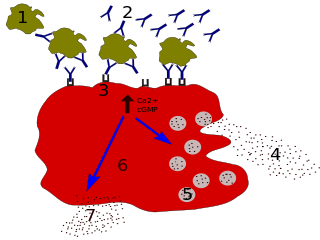
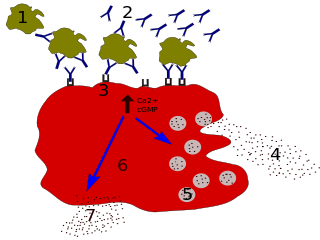
Immunoglobulin E (IgE) is a type of antibody that has been found only in mammals. IgE is synthesised by plasma cells. Monomers of IgE consist of two heavy chains and two light chains, with the ε chain containing four Ig-like constant domains (Cε1–Cε4). IgE is thought to be an important part of the immune response against infection by certain parasitic worms, including Schistosoma mansoni, Trichinella spiralis, and Fasciola hepatica. IgE is also utilized during immune defense against certain protozoan parasites such as Plasmodium falciparum. IgE may have evolved as a defense to protect against venoms.

A food allergy is an abnormal immune response to food. The symptoms of the allergic reaction may range from mild to severe. They may include itchiness, swelling of the tongue, vomiting, diarrhea, hives, trouble breathing, or low blood pressure. This typically occurs within minutes to several hours of exposure. When the symptoms are severe, it is known as anaphylaxis. A food intolerance and food poisoning are separate conditions, not due to an immune response.
Omalizumab, sold under the brand name Xolair, is a medication to treat asthma, nasal polyps, and urticaria (hives).

Allergic conjunctivitis (AC) is inflammation of the conjunctiva due to allergy. Although allergens differ among patients, the most common cause is hay fever. Symptoms consist of redness, edema (swelling) of the conjunctiva, itching, and increased lacrimation. If this is combined with rhinitis, the condition is termed allergic rhinoconjunctivitis (ARC).

Atopy is the tendency to produce an exaggerated immunoglobulin E (IgE) immune response to otherwise harmless substances in the environment. Allergic diseases are clinical manifestations of such inappropriate, atopic responses.

Peanut allergy is a type of food allergy to peanuts. It is different from tree nut allergies, because peanuts are legumes and not true nuts. Physical symptoms of allergic reaction can include itchiness, hives, swelling, eczema, sneezing, asthma attack, abdominal pain, drop in blood pressure, diarrhea, and cardiac arrest. Anaphylaxis may occur. Those with a history of asthma are more likely to be severely affected.

Soy allergy is a type of food allergy. It is a hypersensitivity to ingesting compounds in soy, causing an overreaction of the immune system, typically with physical symptoms, such as gastrointestinal discomfort, respiratory distress, or a skin reaction. Soy is among the eight most common foods inducing allergic reactions in children and adults. It has a prevalence of about 0.3% in the general population.

Milk allergy is an adverse immune reaction to one or more proteins in cow's milk. Symptoms may take hours to days to manifest, with symptoms including atopic dermatitis, inflammation of the esophagus, enteropathy involving the small intestine and proctocolitis involving the rectum and colon. However, rapid anaphylaxis is possible, a potentially life-threatening condition that requires treatment with epinephrine, among other measures.

Egg allergy is an immune hypersensitivity to proteins found in chicken eggs, and possibly goose, duck, or turkey eggs. Symptoms can be either rapid or gradual in onset. The latter can take hours to days to appear. The former may include anaphylaxis, a potentially life-threatening condition which requires treatment with epinephrine. Other presentations may include atopic dermatitis or inflammation of the esophagus.

A tree nut allergy is a hypersensitivity to dietary substances from tree nuts and edible tree seeds causing an overreaction of the immune system which may lead to severe physical symptoms. Tree nuts include almonds, Brazil nuts, cashews, chestnuts, filberts/hazelnuts, macadamia nuts, pecans, pistachios, shea nuts and walnuts.
Enzyme potentiated desensitization (EPD), is a treatment for allergies developed in the 1960s by Dr. Leonard M. McEwen in the United Kingdom. EPD uses much lower doses of antigens than conventional desensitization treatment paired with the enzyme β-glucuronidase. EPD is approved in the United Kingdom for the treatment of hay fever, food allergy and intolerance and environmental allergies.
Peanut Allergen Powder, sold under the brand name Palforzia, is an oral medication for the treatment of allergic reactions, including anaphylaxis, in children typically aged between four and 17 years of age who have confirmed cases of peanut allergy. It is taken by mouth.

Fish allergy is an immune hypersensitivity to proteins found in fish. Symptoms can be either rapid or gradual in onset. The latter can take hours to days to appear. The former may include anaphylaxis, a potentially life-threatening condition which requires treatment with epinephrine. Other presentations may include atopic dermatitis or inflammation of the esophagus. Fish is one of the eight common food allergens which are responsible for 90% of allergic reactions to foods: cow's milk, eggs, wheat, shellfish, peanuts, tree nuts, fish, and soy beans.

Dust mite allergy, also known as house dust allergy, is a sensitization and allergic reaction to the droppings of house dust mites. The allergy is common and can trigger allergic reactions such as asthma, eczema or itching. The mite's gut contains potent digestive enzymes that persist in their feces and are major inducers of allergic reactions such as wheezing. The mite's exoskeleton can also contribute to allergic reactions. Unlike scabies mites or skin follicle mites, house dust mites do not burrow under the skin and are not parasitic.

Shellfish allergy is among the most common food allergies. "Shellfish" is a colloquial and fisheries term for aquatic invertebrates used as food, including various species of molluscs such as clams, mussels, oysters and scallops, crustaceans such as shrimp, lobsters and crabs, and cephalopods such as squid and octopus. Shellfish allergy is an immune hypersensitivity to proteins found in shellfish. Symptoms can be either rapid or gradual in onset. The latter can take hours to days to appear. The former may include anaphylaxis, a potentially life-threatening condition which requires treatment with epinephrine. Other presentations may include atopic dermatitis or inflammation of the esophagus. Shellfish is one of the eight common food allergens, responsible for 90% of allergic reactions to foods: cow's milk, eggs, wheat, shellfish, peanuts, tree nuts, fish, and soy beans.

A food allergy to sesame seeds has prevalence estimates in the range of 0.1–0.2% of the general population, and are higher in the Middle East and other countries where sesame seeds are used in traditional foods. Reporting of sesame seed allergy has increased in the 21st century, either due to a true increase from exposure to more sesame foods or due to an increase in awareness. Increasing sesame allergy rates have induced more countries to regulate food labels to identify sesame ingredients in products and the potential for allergy. In the United States, sesame became the ninth food allergen with mandatory labeling, effective 1 January 2023.