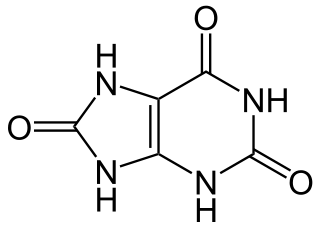
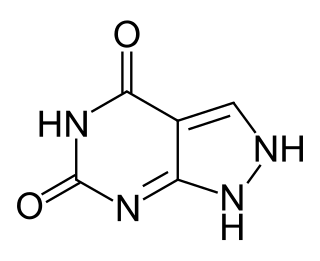
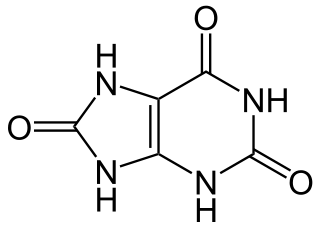
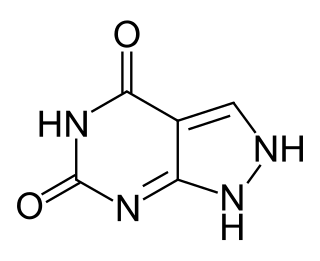
Uric acid is a heterocyclic compound of carbon, nitrogen, oxygen, and hydrogen with the formula C5H4N4O3. It forms ions and salts known as urates and acid urates, such as ammonium acid urate. Uric acid is a product of the metabolic breakdown of purine nucleotides, and it is a normal component of urine. High blood concentrations of uric acid can lead to gout and are associated with other medical conditions, including diabetes and the formation of ammonium acid urate kidney stones.

Xanthine is a purine base found in most human body tissues and fluids, as well as in other organisms. Several stimulants are derived from xanthine, including caffeine, theophylline, and theobromine.

Gout is a form of inflammatory arthritis characterized by recurrent attacks of a red, tender, hot, and swollen joint, caused by the deposition of needle-like crystals of uric acid known as monosodium urate crystals. Pain typically comes on rapidly, reaching maximal intensity in less than 12 hours. The joint at the base of the big toe is affected (Podagra) in about half of cases. It may also result in tophi, kidney stones, or kidney damage.
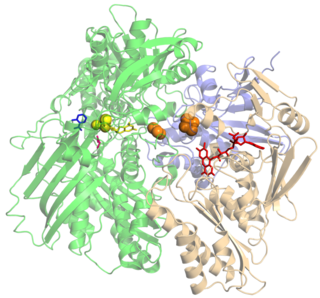
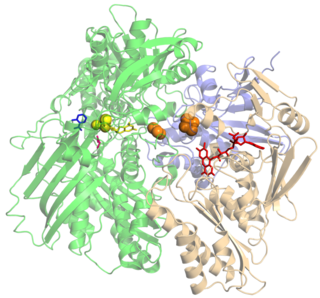
Xanthine oxidase is a form of xanthine oxidoreductase, a type of enzyme that generates reactive oxygen species. These enzymes catalyze the oxidation of hypoxanthine to xanthine and can further catalyze the oxidation of xanthine to uric acid. These enzymes play an important role in the catabolism of purines in some species, including humans.
Hyperuricaemia or hyperuricemia is an abnormally high level of uric acid in the blood. In the pH conditions of body fluid, uric acid exists largely as urate, the ion form. Serum uric acid concentrations greater than 6 mg/dL for females, 7 mg/dL for men, and 5.5 mg/dL for youth are defined as hyperuricemia. The amount of urate in the body depends on the balance between the amount of purines eaten in food, the amount of urate synthesised within the body, and the amount of urate that is excreted in urine or through the gastrointestinal tract. Hyperuricemia may be the result of increased production of uric acid, decreased excretion of uric acid, or both increased production and reduced excretion.
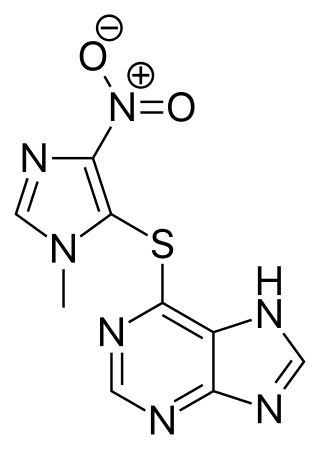
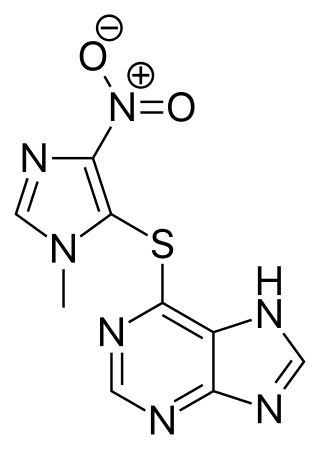
Azathioprine, sold under the brand name Imuran, among others, is an immunosuppressive medication. It is used for the treatment of rheumatoid arthritis, granulomatosis with polyangiitis, Crohn's disease, ulcerative colitis, and systemic lupus erythematosus; and in kidney transplants to prevent rejection. It is listed by the International Agency for Research on Cancer as a group 1 human carcinogen. It is taken by mouth or injected into a vein.

Lesch–Nyhan syndrome (LNS) is a rare inherited disorder caused by a deficiency of the enzyme hypoxanthine-guanine phosphoribosyltransferase (HGPRT). This deficiency occurs due to mutations in the HPRT1 gene located on the X chromosome. LNS affects about 1 in 380,000 live births. The disorder was first recognized and clinically characterized by American medical student Michael Lesch and his mentor, pediatrician William Nyhan, at Johns Hopkins.

Rasburicase is a medication that helps to clear uric acid from the blood. It is a recombinant version of urate oxidase, an enzyme that metabolizes uric acid to allantoin. Urate oxidase is known to be present in many mammals but does not naturally occur in humans. Rasburicase is produced by a genetically modified Saccharomyces cerevisiae strain. The complementary DNA (cDNA) coding for rasburicase was cloned from a strain of Aspergillus flavus.

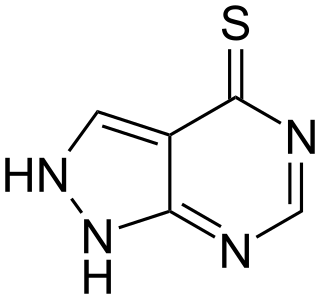
Mercaptopurine (6-MP), sold under the brand name Purinethol among others, is a medication used for cancer and autoimmune diseases. Specifically it is used to treat acute lymphocytic leukemia (ALL), acute promyelocytic leukemia (APL), Crohn's disease, and ulcerative colitis. For acute lymphocytic leukemia it is generally used with methotrexate. It is taken orally.

Thiopurine methyltransferase or thiopurine S-methyltransferase (TPMT) is an enzyme that in humans is encoded by the TPMT gene. A pseudogene for this locus is located on chromosome 18q.

Hypouricemia or hypouricaemia is a level of uric acid in blood serum that is below normal. In humans, the normal range of this blood component has a lower threshold set variously in the range of 2 mg/dL to 4 mg/dL, while the upper threshold is 530 μmol/L (6 mg/dL) for women and 619 μmol/L (7 mg/dL) for men. Hypouricemia usually is benign and sometimes is a sign of a medical condition.
Acute uric acid nephropathy is a rapidly worsening (decreasing) kidney function that is caused by high levels of uric acid in the urine (hyperuricosuria).
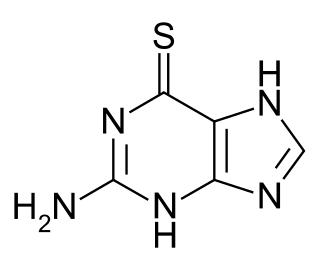
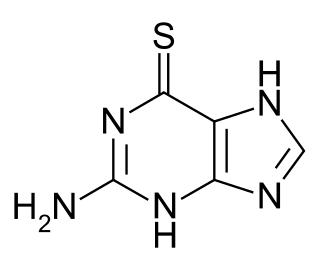
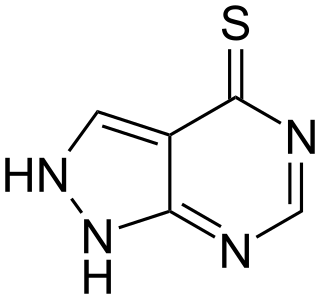
Tioguanine, also known as thioguanine or 6-thioguanine (6-TG) or tabloid is a medication used to treat acute myeloid leukemia (AML), acute lymphocytic leukemia (ALL), and chronic myeloid leukemia (CML). Long-term use is not recommended. It is given by mouth.
Purine metabolism refers to the metabolic pathways to synthesize and break down purines that are present in many organisms.

Febuxostat, sold under the brand names Uloric among others, is a medication used long-term to treat gout due to high uric acid levels. It is generally recommended only for people who cannot take allopurinol. When initially started, medications such as NSAIDs are often recommended to prevent gout flares. It is taken by mouth.

Hyperuricosuria is a medical term referring to the presence of excessive amounts of uric acid in the urine. For men this is at a rate greater than 800 mg/day, and for women, 750 mg/day. Notable direct causes of hyperuricosuria are dissolution of uric acid crystals in the kidneys or urinary bladder, and hyperuricemia. Notable indirect causes include uricosuric drugs, rapid breakdown of bodily tissues containing large quantities of DNA and RNA, and a diet high in purine.
Oxipurinol is an inhibitor of xanthine oxidase. It is an active metabolite of allopurinol and it is cleared renally. In cases of renal disease, this metabolite will accumulate to toxic levels. By inhibiting xanthine oxidase, it reduces uric acid production. High serum uric acid levels may result in gout, kidney stones, and other medical conditions.
Tisopurine is a drug used in the treatment of gout in some countries. It reduces uric acid production through inhibiting an early stage in its production.
A xanthine oxidase inhibitor is any substance that inhibits the activity of xanthine oxidase, an enzyme involved in purine metabolism. In humans, inhibition of xanthine oxidase reduces the production of uric acid, and several medications that inhibit xanthine oxidase are indicated for treatment of hyperuricemia and related medical conditions including gout. Xanthine oxidase inhibitors are being investigated for management of reperfusion injury.

Lesinurad is a urate transporter inhibitor for treating high blood uric acid levels associated with gout. It is recommended only as an adjuvant with either allopurinol or febuxostat when these medications are not sufficient.