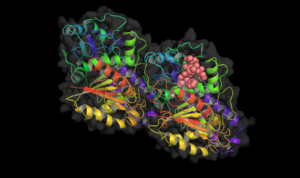
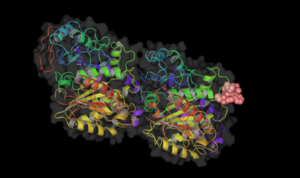
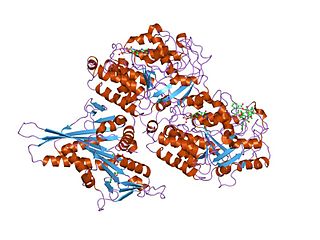
Microtubules are polymers of tubulin that form part of the cytoskeleton and provide structure and shape to eukaryotic cells. Microtubules can be as long as 50 micrometres, as wide as 23 to 27 nm and have an inner diameter between 11 and 15 nm. They are formed by the polymerization of a dimer of two globular proteins, alpha and beta tubulin into protofilaments that can then associate laterally to form a hollow tube, the microtubule. The most common form of a microtubule consists of 13 protofilaments in the tubular arrangement.

Nocodazole is an antineoplastic agent which exerts its effect in cells by interfering with the polymerization of microtubules. Microtubules are one type of fibre which constitutes the cytoskeleton, and the dynamic microtubule network has several important roles in the cell, including vesicular transport, forming the mitotic spindle and in cytokinesis. Several drugs including vincristine and colcemid are similar to nocodazole in that they interfere with microtubule polymerization.
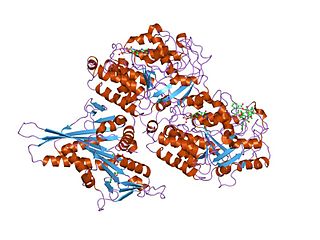
Tubulin in molecular biology can refer either to the tubulin protein superfamily of globular proteins, or one of the member proteins of that superfamily. α- and β-tubulins polymerize into microtubules, a major component of the eukaryotic cytoskeleton. Microtubules function in many essential cellular processes, including mitosis. Tubulin-binding drugs kill cancerous cells by inhibiting microtubule dynamics, which are required for DNA segregation and therefore cell division.
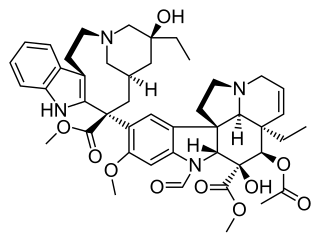
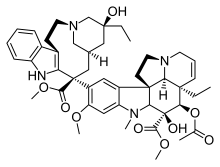
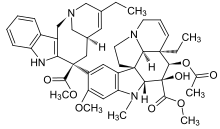
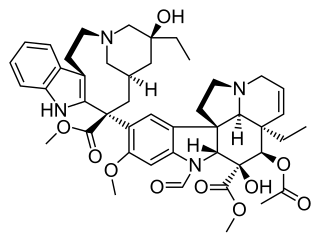
Vincristine, also known as leurocristine and marketed under the brand name Oncovin among others, is a chemotherapy medication used to treat a number of types of cancer. This includes acute lymphocytic leukemia, acute myeloid leukemia, Hodgkin's disease, neuroblastoma, and small cell lung cancer among others. It is given intravenously.

Vinorelbine (NVB), sold under the brand name Navelbine among others, is a chemotherapy medication used to treat a number of types of cancer. This includes breast cancer and non-small cell lung cancer. It is given by injection into a vein or by mouth.

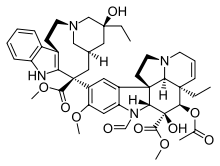
Vinblastine (VBL), sold under the brand name Velban among others, is a chemotherapy medication, typically used with other medications, to treat a number of types of cancer. This includes Hodgkin's lymphoma, non-small-cell lung cancer, bladder cancer, brain cancer, melanoma, and testicular cancer. It is given by injection into a vein.
A spindle poison, also known as a spindle toxin, is a poison that disrupts cell division by affecting the protein threads that connect the centromere regions of chromosomes, known as spindles. Spindle poisons effectively cease the production of new cells by interrupting the mitosis phase of cell division at the spindle assembly checkpoint (SAC). However, as numerous and varied as they are, spindle poisons are not yet 100% effective at ending the formation of tumors (neoplasms). Although not 100% effective, substantive therapeutic efficacy has been found in these types of chemotherapeutic treatments. The mitotic spindle is composed of microtubules that aid, along with regulatory proteins, each other in the activity of appropriately segregating replicated chromosomes. Certain compounds affecting the mitotic spindle have proven highly effective against solid tumors and hematological malignancies.

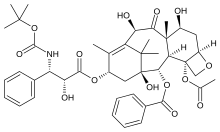
Taxanes are a class of diterpenes. They were originally identified from plants of the genus Taxus (yews), and feature a taxadiene core. Paclitaxel (Taxol) and docetaxel (Taxotere) are widely used as chemotherapy agents. Cabazitaxel was FDA approved to treat hormone-refractory prostate cancer.
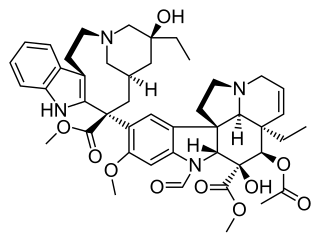
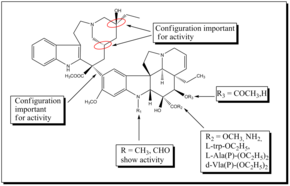
Vinca alkaloids are a set of anti-mitotic and anti-microtubule alkaloid agents originally derived from the periwinkle plant Catharanthus roseus and other vinca plants. They block beta-tubulin polymerization in a dividing cell.

Epothilones are a class of potential cancer drugs. Like taxanes, they prevent cancer cells from dividing by interfering with tubulin, but in early trials, epothilones have better efficacy and milder adverse effects than taxanes.

Vindesine, also termed Eldisine, is a semisynthetic vinca alkaloid derived from the flowering plant Catharanthus roseus. Like the natural and semisynthetic vinca alkaloids derived from this plant, vindesine is an inhibitor of mitosis that is used as a chemotherapy drug. By inhibiting mitosis, vinedsine blocks the proliferation of cells, particularly the rapidly proliferation cells of certain types of cancer. It is used, generally in combination with other chemotherapeutic drugs, in the treatment of various malignancies such as leukaemia, lymphoma, melanoma, breast cancer, and lung cancer.

Rhizoxin is an antimitotic agent with anti-tumor activity. It is isolated from a pathogenic plant fungus which causes rice seedling blight.

Combretastatin is a dihydrostilbenoid found in Combretum caffrum.

Eribulin, sold under the brand name Halaven among others, is an anti-cancer medication used to treat breast cancer and liposarcoma.
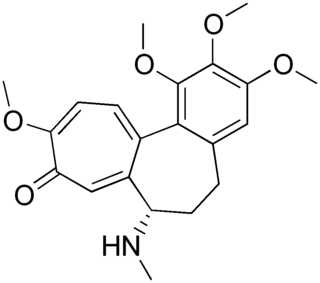
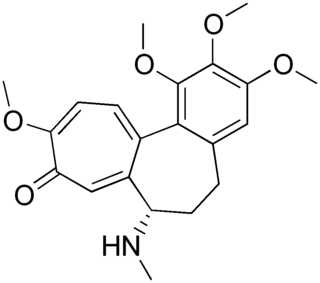
Demecolcine is a drug used in chemotherapy. It is closely related to the natural alkaloid colchicine with the replacement of the acetyl group on the amino moiety with methyl, but it is less toxic. It depolymerises microtubules and limits microtubule formation, thus arresting cells in metaphase and allowing cell harvest and karyotyping to be performed.

Paclitaxel trevatide is an experimental chemotherapy drug that is under development by Angiochem Inc, a Canadian biotech company. Phase II clinical trials have completed for several indications, and the company is preparing for phase III trials.

Taccalonolides are a class of microtubule-stabilizing agents isolated from Tacca chantrieri that has been shown to have selective cancer-fighting properties. Other examples of microtubule-stabilizing agents include taxanes and epothilones, both of which prevent cancer cells from dividing by interfering with tubulin. While taxanes like Paclitaxel and docetaxel have been used successfully against breast, ovarian, prostate, and non–small-cell lung cancers, intrinsic and acquired drug resistance limit their anticancer properties. Unlike taxanes, taccalonolides appear to work through a different mechanism of action that does not involve tubulin, although recently isolated taccalonolides AF and AJ have shown tubulin-interaction activity. The discovery of taccalonolides opens up new possibilities to treat cancer cells, especially ones that are taxane or epithilone resistant.
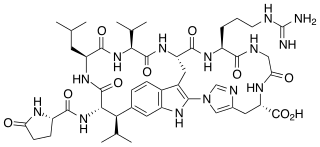
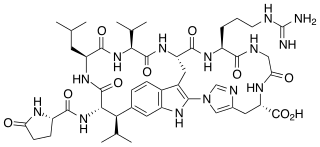
Moroidin is a biologically active compound found in the plants Dendrocnide moroides and Celosia argentea. It is a peptide composed of eight amino acids, with unusual leucine-tryptophan and tryptophan-histidine cross-links that form its two rings. Moroidin has been shown to be at least one of several bioactive compounds responsible for the painful sting of the Dendrocnide moroides plant. It also has demonstrated anti-mitotic properties, specifically by inhibition of tubulin polymerization. Anti-mitotic activity gives moroidin potential as a chemotherapy drug, and this property combined with its unusual chemical structure has made it a target for organic synthesis.

2-Methoxyestradiol disulfamate is a synthetic, oral active anti-cancer medication which was previously under development for potential clinical use. It has improved potency, low metabolism, and good pharmacokinetic properties relative to 2-methoxyestradiol (2-MeO-E2). It is also a potent inhibitor of steroid sulfatase, the enzyme that catalyzes the desulfation of steroids such as estrone sulfate and dehydroepiandrosterone sulfate (DHEA-S).
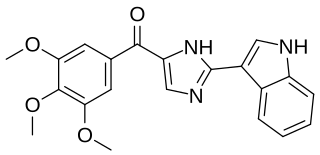
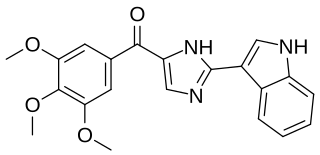
Sabizabulin is a chemical compound from the group of indole and imidazole derivatives that was first reported in 2012 by Dalton, Li, and Miller. It is being studied as a mitotic inhibitor and chemotherapeutic agent in castration-resistant metastatic prostate cancer and in SARS-CoV-2 (COVID-19) infections.