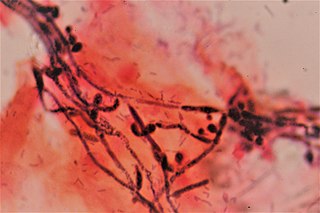
Candidiasis is a fungal infection due to any species of the genus Candida. When it affects the mouth, in some countries it is commonly called thrush. Signs and symptoms include white patches on the tongue or other areas of the mouth and throat. Other symptoms may include soreness and problems swallowing. When it affects the vagina, it may be referred to as a yeast infection or thrush. Signs and symptoms include genital itching, burning, and sometimes a white "cottage cheese-like" discharge from the vagina. Yeast infections of the penis are less common and typically present with an itchy rash. Very rarely, yeast infections may become invasive, spreading to other parts of the body. This may result in fevers, among other symptoms.
Vaginitis, also known as vulvovaginitis, is inflammation of the vagina and vulva. Symptoms may include itching, burning, pain, discharge, and a bad smell. Certain types of vaginitis may result in complications during pregnancy.

An antifungal medication, also known as an antimycotic medication, is a pharmaceutical fungicide or fungistatic used to treat and prevent mycosis such as athlete's foot, ringworm, candidiasis (thrush), serious systemic infections such as cryptococcal meningitis, and others. Such drugs are usually obtained by a doctor's prescription, but a few are available over the counter (OTC). The evolution of antifungal resistance is a growing threat to health globally.

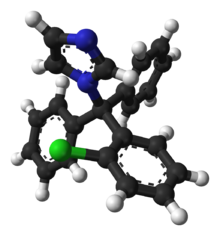
Nystatin, sold under the brand name Mycostatin among others, is an antifungal medication. It is used to treat Candida infections of the skin including diaper rash, thrush, esophageal candidiasis, and vaginal yeast infections. It may also be used to prevent candidiasis in those who are at high risk. Nystatin may be used by mouth, in the vagina, or applied to the skin.

Miconazole, sold under the brand name Monistat among others, is an antifungal medication used to treat ring worm, pityriasis versicolor, and yeast infections of the skin or vagina. It is used for ring worm of the body, groin, and feet. It is applied to the skin or vagina as a cream or ointment.

Athlete's foot, known medically as tinea pedis, is a common skin infection of the feet caused by a fungus. Signs and symptoms often include itching, scaling, cracking and redness. In rare cases the skin may blister. Athlete's foot fungus may infect any part of the foot, but most often grows between the toes. The next most common area is the bottom of the foot. The same fungus may also affect the nails or the hands. It is a member of the group of diseases known as tinea.

Terbinafine, sold under the brand name Lamisil among others, is an antifungal medication used to treat pityriasis versicolor, fungal nail infections, and ringworm including jock itch and athlete's foot. It is either taken by mouth or applied to the skin as a cream or ointment. The cream and ointment are not effective for nail infections.
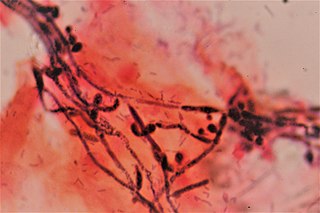
Dermatophyte is a common label for a group of fungus of Arthrodermataceae that commonly causes skin disease in animals and humans. Traditionally, these anamorphic mold genera are: Microsporum, Epidermophyton and Trichophyton. There are about 40 species in these three genera. Species capable of reproducing sexually belong in the teleomorphic genus Arthroderma, of the Ascomycota. As of 2019 a total of nine genera are identified and new phylogenetic taxonomy has been proposed.

Tinea corporis is a fungal infection of the body, similar to other forms of tinea. Specifically, it is a type of dermatophytosis that appears on the arms and legs, especially on glabrous skin; however, it may occur on any superficial part of the body.

Terconazole is an antifungal drug used to treat vaginal yeast infection. It comes as a lotion or a suppository and disrupts the biosynthesis of fats in a yeast cell. It has a relatively broad spectrum compared to azole compounds but not triazole compounds. Testing shows that it is a suitable compound for prophylaxis for those that suffer from chronic vulvovaginal candidiasis.

Dermatophytosis, also known as ringworm, is a fungal infection of the skin (Dermatomycosis). Typically it results in a red, itchy, scaly, circular rash. Hair loss may occur in the area affected. Symptoms begin four to fourteen days after exposure. Multiple areas can be affected at a given time.

Tioconazole is an antifungal medication of the imidazole class used to treat infections caused by a fungus or yeast. It is marketed under the brand names Trosyd and Gyno-Trosyd. Tioconazole ointments serve to treat women's vaginal yeast infections. They are available in one day doses, as opposed to the 7-day treatments commonly used in the past.

Tinea faciei is a fungal infection of the skin of the face. It generally appears as a photosensitive painless red rash with small bumps and a raised edge appearing to grow outwards, usually over eyebrows or one side of the face. It may feel wet or have some crusting, and overlying hairs may fall out easily. There may be a mild itch.
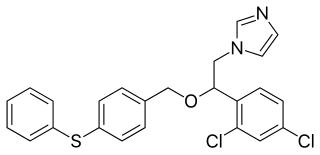
Fenticonazole is an imidazole antifungal drug, used locally as the nitrate in the treatment of vulvovaginal candidiasis. It is active against a range of organisms including dermatophyte pathogens, Malassezia furfur, and Candida albicans. Fenticonazole has also been shown to exhibit antibacterial action, with a spectrum of activity that includes bacteria commonly associated with superinfected fungal skin and vaginal infections, and antiparasitic action against the protozoan Trichomonas vaginalis.

Tinea incognita, also spelled tinea incognito, is a fungal infection of the skin that generally looks odd for a typical tinea infection. The border of the skin lesion is usually blurred and it appears to have florid growth.
Vaginal yeast infection, also known as candidal vulvovaginitis and vaginal thrush, is excessive growth of yeast in the vagina that results in irritation. The most common symptom is vaginal itching, which may be severe. Other symptoms include burning with urination, a thick, white vaginal discharge that typically does not smell bad, pain during sex, and redness around the vagina. Symptoms often worsen just before a woman's period.
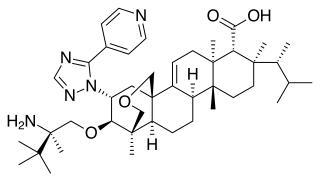
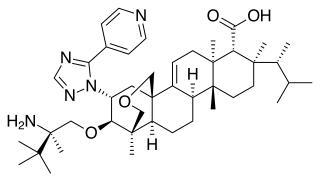
Ibrexafungerp, sold under the brand name Brexafemme, is an antifungal medication used to treat vulvovaginal candidiasis (VVC). It is taken orally. It is also currently undergoing clinical trials for other indications via an intravenous (IV) formulation. An estimated 75% of women will have at least one episode of VVC and 40 to 45% will have two or more episodes in their lifetime.
Topical antifungaldrugs are used to treat fungal infections on the skin, scalp, nails, vagina or inside the mouth. These medications come as creams, gels, lotions, ointments, powders, shampoos, tinctures and sprays. Most antifungal drugs induce fungal cell death by destroying the cell wall of the fungus. These drugs inhibit the production of ergosterol, which is a fundamental component of the fungal cell membrane and wall.

Oteseconazole, a novel orally bioavailable and selective inhibitor of fungal cytochrome P450 enzyme 51 (CYP51), has shown promising efficacy in the treatment of recurrent vulvovaginal candidiasis (RVVC) in patients.