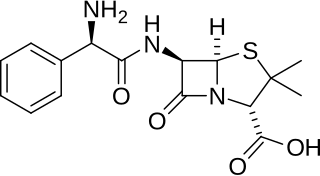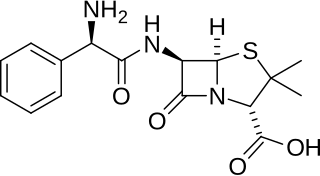
Ampicillin is an antibiotic belonging to the aminopenicillin class of the penicillin family. The drug is used to prevent and treat a number of bacterial infections, such as respiratory tract infections, urinary tract infections, meningitis, salmonellosis, and endocarditis. It may also be used to prevent group B streptococcal infection in newborns. It is used by mouth, by injection into a muscle, or intravenously.

Phenytoin (PHT), sold under the brand name Dilantin among others, is an anti-seizure medication. It is useful for the prevention of tonic-clonic seizures and focal seizures, but not absence seizures. The intravenous form, fosphenytoin, is used for status epilepticus that does not improve with benzodiazepines. It may also be used for certain heart arrhythmias or neuropathic pain. It can be taken intravenously or by mouth. The intravenous form generally begins working within 30 minutes and is effective for roughly 24 hours. Blood levels can be measured to determine the proper dose.
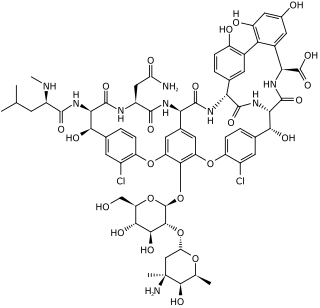
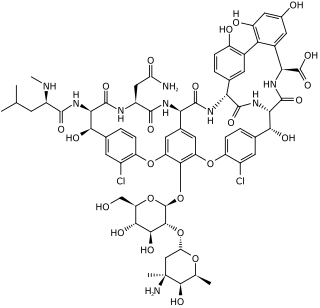
Vancomycin is a glycopeptide antibiotic medication used to treat a number of bacterial infections. It is used intravenously as a treatment for complicated skin infections, bloodstream infections, endocarditis, bone and joint infections, and meningitis caused by methicillin-resistant Staphylococcus aureus. Blood levels may be measured to determine the correct dose. Vancomycin is also taken orally as a treatment for severe Clostridium difficile colitis. When taken orally it is poorly absorbed.
Aplastic anemia (AA) is a severe hematologic condition in which the body fails to make blood cells in sufficient numbers. Aplastic anemia is associated with cancer and various cancer syndromes. Blood cells are produced in the bone marrow by stem cells that reside there. Aplastic anemia causes a deficiency of all blood cell types: red blood cells, white blood cells, and platelets.

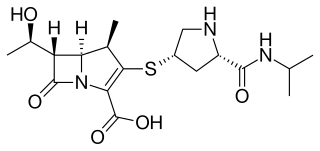
Ertapenem, sold under the brand name Invanz, is a carbapenem antibiotic medication used for the treatment of infections of the abdomen, the lungs, the upper part of the female reproductive system, and the diabetic foot.

Linezolid is an antibiotic used for the treatment of infections caused by Gram-positive bacteria that are resistant to other antibiotics. Linezolid is active against most Gram-positive bacteria that cause disease, including streptococci, vancomycin-resistant enterococci (VRE), and methicillin-resistant Staphylococcus aureus (MRSA). The main uses are infections of the skin and pneumonia although it may be used for a variety of other infections including drug-resistant tuberculosis. It is used either by injection into a vein or by mouth.

Clindamycin is a lincosamide antibiotic medication used for the treatment of a number of bacterial infections, including osteomyelitis (bone) or joint infections, pelvic inflammatory disease, strep throat, pneumonia, acute otitis media, and endocarditis. It can also be used to treat acne, and some cases of methicillin-resistant Staphylococcus aureus (MRSA). In combination with quinine, it can be used to treat malaria. It is available by mouth, by injection into a vein, and as a cream or a gel to be applied to the skin or in the vagina.
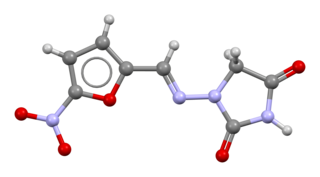
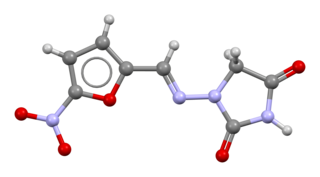
Nitrofurantoin is an antibacterial medication of the nitrofuran class used to treat urinary tract infections, although it is not as effective for kidney infections. It is taken by mouth.

Colistin, also known as polymyxin E, is an antibiotic medication used as a last-resort treatment for multidrug-resistant Gram-negative infections including pneumonia. These may involve bacteria such as Pseudomonas aeruginosa, Klebsiella pneumoniae, or Acinetobacter. It comes in two forms: colistimethate sodium can be injected into a vein, injected into a muscle, or inhaled, and colistin sulfate is mainly applied to the skin or taken by mouth. Colistimethate sodium is a prodrug; it is produced by the reaction of colistin with formaldehyde and sodium bisulfite, which leads to the addition of a sulfomethyl group to the primary amines of colistin. Colistimethate sodium is less toxic than colistin when administered parenterally. In aqueous solutions it undergoes hydrolysis to form a complex mixture of partially sulfomethylated derivatives, as well as colistin. Resistance to colistin began to appear as of 2015.

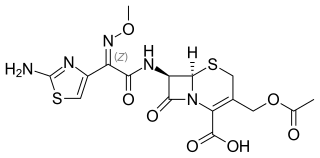
Ceftriaxone, sold under the brand name Rocephin, is a third-generation cephalosporin antibiotic used for the treatment of a number of bacterial infections. These include middle ear infections, endocarditis, meningitis, pneumonia, bone and joint infections, intra-abdominal infections, skin infections, urinary tract infections, gonorrhea, and pelvic inflammatory disease. It is also sometimes used before surgery and following a bite wound to try to prevent infection. Ceftriaxone can be given by injection into a vein or into a muscle.
Meropenem, sold under the brand name Merrem among others, is an intravenous carbapenem antibiotic used to treat a variety of bacterial infections. Some of these include meningitis, intra-abdominal infection, pneumonia, sepsis, and anthrax.
Pancytopenia is a medical condition in which there is significant reduction in the number of almost all blood cells.

Ceftazidime, sold under the brand name Fortaz among others, is a third-generation cephalosporin antibiotic useful for the treatment of a number of bacterial infections. Specifically it is used for joint infections, meningitis, pneumonia, sepsis, urinary tract infections, malignant otitis externa, Pseudomonas aeruginosa infection, and vibrio infection. It is given by injection into a vein, muscle, or eye.

Cefaclor, sold under the trade name Ceclor among others, is a second-generation cephalosporin antibiotic used to treat certain bacterial infections such as pneumonia and infections of the ear, lung, skin, throat, and urinary tract. It is also available from other manufacturers as a generic.

Tigecycline, sold under the brand name Tygacil, is a tetracycline antibiotic medication for a number of bacterial infections. It is a glycylcycline class drug that is administered intravenously. It was developed in response to the growing rate of antibiotic resistant bacteria such as Staphylococcus aureus, Acinetobacter baumannii, and E. coli. As a tetracycline derivative antibiotic, its structural modifications has expanded its therapeutic activity to include Gram-positive and Gram-negative organisms, including those of multi-drug resistance.
Cefotaxime is an antibiotic used to treat a number of bacterial infections in human, other animals and plant tissue culture. Specifically in humans it is used to treat joint infections, pelvic inflammatory disease, meningitis, pneumonia, urinary tract infections, sepsis, gonorrhea, and cellulitis. It is given either by injection into a vein or muscle.

Flucytosine, also known as 5-fluorocytosine (5-FC), is an antifungal medication. It is specifically used, together with amphotericin B, for serious Candida infections and cryptococcosis. It may be used by itself or with other antifungals for chromomycosis. Flucytosine is used by mouth and by injection into a vein.

Iron supplements, also known as iron salts and iron pills, are a number of iron formulations used to treat and prevent iron deficiency including iron deficiency anemia. For prevention they are only recommended in those with poor absorption, heavy menstrual periods, pregnancy, hemodialysis, or a diet low in iron. Prevention may also be used in low birth weight babies. They are taken by mouth, injection into a vein, or injection into a muscle. While benefits may be seen in days, up to two months may be required until iron levels return to normal.
A drug of last resort (DoLR), also known as a heroic dose, is a pharmaceutical drug which is tried after all other drug options have failed to produce an adequate response in the patient. Drug resistance, such as antimicrobial resistance or antineoplastic resistance, may make the first-line drug ineffective, especially in case of multidrug-resistant pathogens and tumors. Such an alternative may be outside of extant regulatory requirements or medical best practices, in which case it may be viewed as salvage therapy.
Gray baby syndrome is a rare but serious, even fatal, side effect that occurs in newborn infants following the accumulation of the antibiotic chloramphenicol. Chloramphenicol is a broad-spectrum antibiotic that has been used to treat a variety of bacteria infections like Streptococcus pneumoniae as well as typhoid fever, meningococcal sepsis, cholera, and eye infections. Chloramphenicol works by binding to ribosomal subunits which blocks transfer ribonucleic acid (RNA) and prevents the synthesis of bacterial proteins. Chloramphenicol has also been used to treat neonates born before 37 weeks of the gestational period for prophylactic purposes. In 1958, newborns born prematurely due to rupture of the amniotic sac were given chloramphenicol to prevent possible infections, and it was noticed that these newborns had a higher mortality rate compared with those who were not treated with the antibiotic. Over the years, chloramphenicol has been used less in clinical practice due to the risks of toxicity not only to neonates, but also to adults due to the risk of aplastic anemia. Chloramphenicol is now reserved to treat certain severe bacteria infections that were not successfully treated with other antibiotic medications.