Syphilis is a sexually transmitted infection caused by the bacterium Treponema pallidum subspecies pallidum. The signs and symptoms of syphilis vary depending in which of the four stages it presents. The primary stage classically presents with a single chancre though there may be multiple sores. In secondary syphilis, a diffuse rash occurs, which frequently involves the palms of the hands and soles of the feet. There may also be sores in the mouth or vagina. In latent syphilis, which can last for years, there are few or no symptoms. In tertiary syphilis, there are gummas, neurological problems, or heart symptoms. Syphilis has been known as "the great imitator" as it may cause symptoms similar to many other diseases.

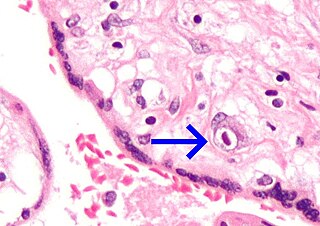
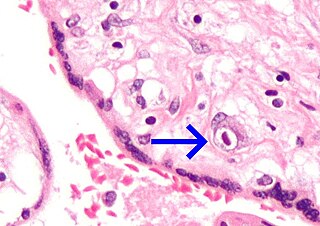
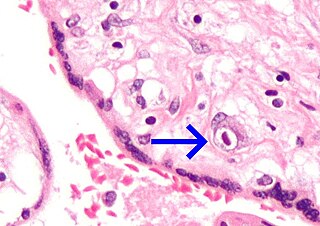
Treponema pallidum, formerly known as Spirochaeta pallida, is a microaerophilic spirochaete bacterium with subspecies that cause the diseases syphilis, bejel, and yaws. It is known to be transmitted only among humans and baboons. It is a helically coiled microorganism usually 6–15 μm long and 0.1–0.2 μm wide. T. pallidum's lack of both a tricarboxylic acid cycle and processes for oxidative phosphorylation results in minimal metabolic activity. The treponemes have cytoplasmic and outer membranes. Using light microscopy, treponemes are visible only by using dark-field illumination. T. pallidum consists of three subspecies, T. p. pallidum, T. p. endemicum, and T. p. pertenue, each of which has a distinct associated disease.

Yaws is a tropical infection of the skin, bones, and joints caused by the spirochete bacterium Treponema pallidum pertenue. The disease begins with a round, hard swelling of the skin, 2 to 5 cm in diameter. The center may break open and form an ulcer. This initial skin lesion typically heals after 3–6 months. After weeks to years, joints and bones may become painful, fatigue may develop, and new skin lesions may appear. The skin of the palms of the hands and the soles of the feet may become thick and break open. The bones may become misshapen. After 5 years or more, large areas of skin may die, leaving scars.

The Venereal Disease Research Laboratory test (VDRL) is a blood test for syphilis and related non-venereal treponematoses that was developed by the eponymous US laboratory. The VDRL test is used to screen for syphilis, whereas other, more specific tests are used to diagnose the disease.

Argyll Robertson pupils are bilateral small pupils that reduce in size on a near object, but do not constrict when exposed to bright light. They are a highly specific sign of neurosyphilis; however, Argyll Robertson pupils may also be a sign of diabetic neuropathy. In general, pupils that accommodate but do not react are said to show light-near dissociation (i.e., it is the absence of a miotic reaction to light, both direct and consensual, with the preservation of a miotic reaction to near stimulus.

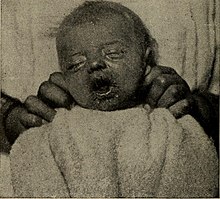
Hemolytic disease of the newborn, also known as hemolytic disease of the fetus and newborn, HDN, HDFN, or erythroblastosis fetalis, is an alloimmune condition that develops in a fetus at or around birth, when the IgG molecules produced by the mother pass through the placenta. Among these antibodies are some which attack antigens on the red blood cells in the fetal circulation, breaking down and destroying the cells. The fetus can develop reticulocytosis and anemia. The intensity of this fetal disease ranges from mild to very severe, and fetal death from heart failure can occur. When the disease is moderate or severe, many erythroblasts are present in the fetal blood, earning these forms of the disease the name erythroblastosis fetalis.
Pinta is a human skin disease caused by infection with the spirochete Treponema carateum, which is morphologically and serologically indistinguishable from the bacterium that causes syphilis. The disease was previously known to be endemic to Mexico, Central America, and South America; it may have been eradicated since, with the latest case occurring in Brazil in 2020.
A vertically transmitted infection is an infection caused by pathogenic bacteria or viruses that use mother-to-child transmission, that is, transmission directly from the mother to an embryo, fetus, or baby during pregnancy or childbirth. It can occur when the mother has a pre-existing disease or becomes infected during pregnancy. Nutritional deficiencies may exacerbate the risks of perinatal infections. Vertical transmission is important for the mathematical modelling of infectious diseases, especially for diseases of animals with large litter sizes, as it causes a wave of new infectious individuals.

Group B streptococcal infection, also known as Group B streptococcal disease or just Group B strep infection, is the infectious disease caused by the bacterium Streptococcus agalactiae, which is the most common human pathogen belonging to the group B of the Lancefield classification of streptococci—hence the group B stretococcal (GBS) infection nomenclature. Infection with GBS can cause serious illness and sometimes death, especially in newborns, the elderly, and people with compromised immune systems. The most severe form of group B streptococcal disease is neonatal meningitis in infants, which is frequently lethal and can cause permanent neuro-cognitive impairment.

Neurosyphilis is the infection of the central nervous system in a patient with syphilis. In the era of modern antibiotics, the majority of neurosyphilis cases have been reported in HIV-infected patients. Meningitis is the most common neurological presentation in early syphilis. Tertiary syphilis symptoms are exclusively neurosyphilis, though neurosyphilis may occur at any stage of infection.
The fluorescent treponemal antibody absorption (FTA-ABS) test is a diagnostic test for syphilis. Using antibodies specific for the Treponema pallidum species, such tests would be assumed to be more specific than non-treponemal testing such as VDRL but have been shown repeatedly to be sensitive but not specific for the diagnosis of neurosyphilis in cerebrospinal fluid (CSF). In addition, FTA-ABS turns positive earlier and remains positive longer than VDRL. Other treponemes, such as T. pertenue, may also produce a positive FTA-ABS. The ABS suffix refers particularly to a processing step used to remove nonspecific antispirochetal antibodies present in normal serum.

Craniotabes is softening or thinning of the skull in infants and children, which may be normally present in newborns. It is seen mostly in the occipital and parietal bones. The bones are soft, and when pressure is applied they will collapse underneath it. When the pressure is relieved, the bones will usually snap back into place.

Blueberry muffin baby, also known as extramedullary hematopoiesis, describes a newborn baby with multiple purpura, associated with several non-cancerous and cancerous conditions in which extra blood is produced in the skin. The bumps range from one to seven mm, do not blanch and have a tendency to occur on the head, neck and trunk. They often fade by three to six weeks after birth, leaving brownish marks. When due to a cancer, the bumps tend to be fewer, firmer and larger.
Congenital cytomegalovirus (cCMV) is cytomegalovirus (CMV) infection in a newborn baby. Most have no symptoms. Some affected babies are small. Other signs and symptoms include a rash, jaundice, hepatomegaly, retinitis, and seizures. It may lead to loss of hearing or vision, developmental disability, or a small head.

The Treponema pallidum particle agglutination assay is an indirect agglutination assay used for detection and titration of antibodies against the causative agent of syphilis, Treponema pallidum subspecies pallidum. It also detects other treponematoses.

Syphilis is a bacterial infection transmitted by sexual contact and is believed to have infected 12 million people in 1999 with greater than 90% of cases in the developing world. It affects between 700,000 and 1.6 million pregnancies a year, resulting in spontaneous abortions, stillbirths, and congenital syphilis. In Sub-Saharan Africa syphilis contributes to approximately 20% of perinatal deaths.

The first recorded outbreak of syphilis in Europe occurred in 1494/1495 in Naples, Italy, during a French invasion. Because it was spread geographically by French troops returning from that campaign, the disease was known as "French disease", and it was not until 1530 that the term "syphilis" was first applied by the Italian physician and poet Girolamo Fracastoro. The causative organism, Treponema pallidum, was first identified by Fritz Schaudinn and Erich Hoffmann in 1905 at the Charité Clinic in Berlin. The first effective treatment, Salvarsan, was developed in 1910 by Sahachiro Hata in the laboratory of Paul Ehrlich. It was followed by the introduction of penicillin in 1943.

Meningeal syphilis is a chronic form of syphilis infection that affects the central nervous system. Treponema pallidum, a spirochate bacterium, is the main cause of syphilis, which spreads drastically throughout the body and can infect all its systems if not treated appropriately. Treponema pallidum is the main cause of the onset of meningeal syphilis and other treponemal diseases, and it consists of a cytoplasmic and outer membrane that can cause a diverse array of diseases in the central nervous system and brain.
HIV in pregnancy is the presence of an HIV/AIDS infection in a woman while she is pregnant. There is a risk of HIV transmission from mother to child in three primary situations: pregnancy, childbirth, and while breastfeeding. This topic is important because the risk of viral transmission can be significantly reduced with appropriate medical intervention, and without treatment HIV/AIDS can cause significant illness and death in both the mother and child. This is exemplified by data from The Centers for Disease Control (CDC): In the United States and Puerto Rico between the years of 2014–2017, where prenatal care is generally accessible, there were 10,257 infants in the United States and Puerto Rico who were exposed to a maternal HIV infection in utero who did not become infected and 244 exposed infants who did become infected.

Neonatal infections are infections of the neonate (newborn) acquired during prenatal development or within the first four weeks of life. Neonatal infections may be contracted by mother to child transmission, in the birth canal during childbirth, or after birth. Neonatal infections may present soon after delivery, or take several weeks to show symptoms. Some neonatal infections such as HIV, hepatitis B, and malaria do not become apparent until much later. Signs and symptoms of infection may include respiratory distress, temperature instability, irritability, poor feeding, failure to thrive, persistent crying and skin rashes.