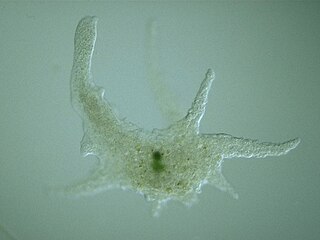
Entamoeba is a genus of Amoebozoa found as internal parasites or commensals of animals. In 1875, Fedor Lösch described the first proven case of amoebic dysentery in St. Petersburg, Russia. He referred to the amoeba he observed microscopically as Amoeba coli; however, it is not clear whether he was using this as a descriptive term or intended it as a formal taxonomic name. The genus Entamoeba was defined by Casagrandi and Barbagallo for the species Entamoeba coli, which is known to be a commensal organism. Lösch's organism was renamed Entamoeba histolytica by Fritz Schaudinn in 1903; he later died, in 1906, from a self-inflicted infection when studying this amoeba. For a time during the first half of the 20th century the entire genus Entamoeba was transferred to Endamoeba, a genus of amoebas infecting invertebrates about which little is known. This move was reversed by the International Commission on Zoological Nomenclature in the late 1950s, and Entamoeba has stayed 'stable' ever since.

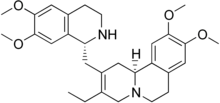
Metronidazole, sold under the brand name Flagyl among others, is an antibiotic and antiprotozoal medication. It is used either alone or with other antibiotics to treat pelvic inflammatory disease, endocarditis, and bacterial vaginosis. It is effective for dracunculiasis, giardiasis, trichomoniasis, and amebiasis. It is an option for a first episode of mild-to-moderate Clostridium difficile colitis if vancomycin or fidaxomicin is unavailable. Metronidazole is available orally, as a cream or gel, and by slow intravenous infusion.

Entamoeba histolytica is an anaerobic parasitic amoebozoan, part of the genus Entamoeba. Predominantly infecting humans and other primates causing amoebiasis, E. histolytica is estimated to infect about 35-50 million people worldwide. E. histolytica infection is estimated to kill more than 55,000 people each year. Previously, it was thought that 10% of the world population was infected, but these figures predate the recognition that at least 90% of these infections were due to a second species, E. dispar. Mammals such as dogs and cats can become infected transiently, but are not thought to contribute significantly to transmission.
Amoebozoa is a major taxonomic group containing about 2,400 described species of amoeboid protists, often possessing blunt, fingerlike, lobose pseudopods and tubular mitochondrial cristae. In traditional classification schemes, Amoebozoa is usually ranked as a phylum within either the kingdom Protista or the kingdom Protozoa. In the classification favored by the International Society of Protistologists, it is retained as an unranked "supergroup" within Eukaryota. Molecular genetic analysis supports Amoebozoa as a monophyletic clade. Modern studies of eukaryotic phylogenetic trees identify it as the sister group to Opisthokonta, another major clade which contains both fungi and animals as well as several other clades comprising some 300 species of unicellular eukaryotes. Amoebozoa and Opisthokonta are sometimes grouped together in a high-level taxon, variously named Unikonta, Amorphea or Opimoda.

Clioquinol (iodochlorhydroxyquin) is an antifungal drug and antiprotozoal drug. It is neurotoxic in large doses. It is a member of a family of drugs called hydroxyquinolines which inhibit certain enzymes related to DNA replication. The drugs have been found to have activity against both viral and protozoal infections.

Famciclovir is a guanosine analogue antiviral drug used for the treatment of various herpesvirus infections, most commonly for herpes zoster (shingles). It is a prodrug form of penciclovir with improved oral bioavailability. Famciclovir is marketed under the trade name Famvir (Novartis).

Auranofin is a gold salt classified by the World Health Organization as an antirheumatic agent. It has the brand name Ridaura.
Antiprotozoal agents is a class of pharmaceuticals used in treatment of protozoan infection.

Miltefosine, sold under the trade name Impavido among others, is a medication mainly used to treat leishmaniasis and free-living amoeba infections such as Naegleria fowleri and Balamuthia mandrillaris. This includes the three forms of leishmaniasis: cutaneous, visceral and mucosal. It may be used with liposomal amphotericin B or paromomycin. It is taken by mouth.

Nitazoxanide, sold under the brand name Alinia among others, is a broad-spectrum antiparasitic and broad-spectrum antiviral medication that is used in medicine for the treatment of various helminthic, protozoal, and viral infections. It is indicated for the treatment of infection by Cryptosporidium parvum and Giardia lamblia in immunocompetent individuals and has been repurposed for the treatment of influenza. Nitazoxanide has also been shown to have in vitro antiparasitic activity and clinical treatment efficacy for infections caused by other protozoa and helminths; evidence as of 2014 suggested that it possesses efficacy in treating a number of viral infections as well.

Diloxanide is a medication used to treat amoeba infections. In places where infections are not common, it is a second line treatment after paromomycin when a person has no symptoms. For people who are symptomatic, it is used after treatment with metronidazole or tinidazole. It is taken by mouth.

Protozoan infections are parasitic diseases caused by organisms formerly classified in the kingdom Protozoa. They are usually contracted by either an insect vector or by contact with an infected substance or surface and include organisms that are now classified in the supergroups Excavata, Amoebozoa, SAR, and Archaeplastida.
An amebicide is an agent that is destructive to amoeba, especially parasitic amoeba that cause amoebiasis.

Amoebiasis, or amoebic dysentery, is an infection of the intestines caused by a parasitic amoeba Entamoeba histolytica. Amoebiasis can be present with no, mild, or severe symptoms. Symptoms may include lethargy, loss of weight, colonic ulcerations, abdominal pain, diarrhea, or bloody diarrhea. Complications can include inflammation and ulceration of the colon with tissue death or perforation, which may result in peritonitis. Anemia may develop due to prolonged gastric bleeding.

A amoebic liver abscess is a type of liver abscess caused by amebiasis. It is the involvement of liver tissue by trophozoites of the organism Entamoeba histolytica and of its abscess due to necrosis.

Amoebic brain abscess is an affliction caused by the anaerobic parasitic protist Entamoeba histolytica. It is extremely rare; the first case being reported in 1849. Brain abscesses resulting from Entamoeba histolytica are difficult to diagnose and very few case reports suggest complete recovery even after the administration of appropriate treatment regimen.
Cutaneous amoebiasis, refers to a form of amoebiasis that presents primarily in the skin. It can be caused by Acanthamoeba or Entamoeba histolytica. When associated with Acanthamoeba, it is also known as "cutaneous acanthamoebiasis". Balamuthia mandrillaris can also cause cutaneous amoebiasis, but can prove fatal if the amoeba enters the bloodstream It is characterized by ulcers. Diagnosis of amebiasis cutis calls for high degree of clinical suspicion. This needs to be backed with demonstration of trophozoites from lesions. Unless an early diagnosis can be made such patients can develop significant morbidity.

Glaucarubin is a quassinoid derived from the tropical shrub, Simarouba glauca. It is used as an antiamoebic agent.
Entamoeba moshkovskii is part of the genus Entamoeba. It is found in areas with polluted water sources, and is prevalent in places such as Malaysia, India, and Bangladesh, but more recently has made its way to Turkey, Australia, and North America. This amoeba is said to rarely infect humans, but recently this has changed. It is in question as to whether it is pathogenic or not. Despite some sources stating this is a free living amoeba, various studies worldwide have shown it contains the ability to infect humans, with some cases of pathogenic potential being reported. Some of the symptoms that often occur are diarrhea, weight loss, bloody stool, and abdominal pain. The first known human infection also known as the "Laredo strain" of Entamoebic mushkovskii was in Laredo, Texas in 1991, although it was first described by a man named Tshalaia in 1941 in Moscow, Russia. It is known to affect people of all ages and genders.
Entamoeba invadens is an amoebozoa parasite of reptiles, within the genus Entamoeba. It is closely related to the human parasite Entamoeba histolytica, causing similar invasive disease in reptiles, in addition to a similar morphology and lifecycle.