Borderline personality disorder (BPD), also known as emotionally unstable personality disorder (EUPD), is a personality disorder characterized by a long-term pattern of intense and unstable interpersonal relationships, distorted sense of self, and strong emotional reactions. Those affected often engage in self-harm and other dangerous behaviors, often due to their difficulty with returning their emotional level to a healthy or normal baseline. They may also struggle with dissociation, a feeling of emptiness, and a fear of abandonment.
Psychology is an academic and applied discipline involving the scientific study of human mental functions and behavior. Occasionally, in addition or opposition to employing the scientific method, it also relies on symbolic interpretation and critical analysis, although these traditions have tended to be less pronounced than in other social sciences, such as sociology. Psychologists study phenomena such as perception, cognition, emotion, personality, behavior, and interpersonal relationships. Some, especially depth psychologists, also study the unconscious mind.

Anhedonia is a diverse array of deficits in hedonic function, including reduced motivation or ability to experience pleasure. While earlier definitions emphasized the inability to experience pleasure, anhedonia is currently used by researchers to refer to reduced motivation, reduced anticipatory pleasure (wanting), reduced consummatory pleasure (liking), and deficits in reinforcement learning. In the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), anhedonia is a component of depressive disorders, substance-related disorders, psychotic disorders, and personality disorders, where it is defined by either a reduced ability to experience pleasure, or a diminished interest in engaging in previously pleasurable activities. While the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) does not explicitly mention anhedonia, the depressive symptom analogous to anhedonia as described in the DSM-5 is a loss of interest or pleasure.

Depersonalization can consist of a detachment within the self, regarding one's mind or body, or being a detached observer of oneself. Subjects feel they have changed and that the world has become vague, dreamlike, less real, lacking in significance or being outside reality while looking in. It can be described as feeling like one is on "autopilot" and that the person's sense of individuality or selfhood has been hindered or suppressed.

A mood swing is an extreme or sudden change of mood. Such changes can play a positive part in promoting problem solving and in producing flexible forward planning, or be disruptive. When mood swings are severe, they may be categorized as part of a mental illness, such as bipolar disorder, where erratic and disruptive mood swings are a defining feature.
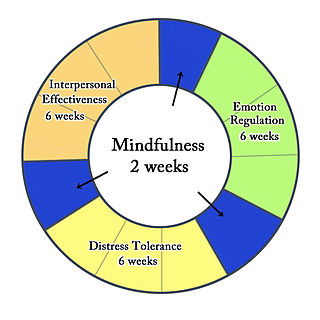
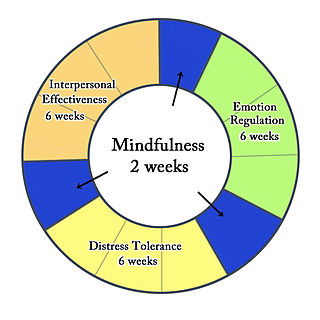
Dialectical behavior therapy (DBT) is an evidence-based psychotherapy that began with efforts to treat personality disorders and interpersonal conflicts. Evidence suggests that DBT can be useful in treating mood disorders and suicidal ideation as well as for changing behavioral patterns such as self-harm and substance use. DBT evolved into a process in which the therapist and client work with acceptance and change-oriented strategies and ultimately balance and synthesize them—comparable to the philosophical dialectical process of thesis and antithesis, followed by synthesis.
In psychoanalytic theory, a defence mechanism is an unconscious psychological operation that functions to protect a person from anxiety-producing thoughts and feelings related to internal conflicts and outer stressors.
Dissociation is a concept that has been developed over time and which concerns a wide array of experiences, ranging from a mild emotional detachment from the immediate surroundings, to a more severe disconnection from physical and emotional experiences. The major characteristic of all dissociative phenomena involves a detachment from reality, rather than a false perception of reality as in psychosis.
Psychological trauma is an emotional response caused by severe distressing events that are outside the normal range of human experiences, with extreme examples being violence, rape, or a terrorist attack. The event must be understood by the affected person as directly threatening the affected person or their loved ones with death, severe bodily injury, or sexual violence; indirect exposure, such as from watching television news, may be extremely distressing and can produce an involuntary and possibly overwhelming physiological stress response, but does not produce trauma per se.
Depersonalization-derealization disorder is a mental disorder in which the person has persistent or recurrent feelings of depersonalization and/or derealization. Depersonalization is described as feeling disconnected or detached from one's self. Individuals may report feeling as if they are an outside observer of their own thoughts or body, and often report feeling a loss of control over their thoughts or actions. Derealization is described as detachment from one's surroundings. Individuals experiencing derealization may report perceiving the world around them as foggy, dreamlike, surreal, and/or visually distorted.
Acute stress reaction is a psychological response to a terrifying, traumatic or surprising experience. It may bring about delayed stress reactions if not correctly addressed. Acute stress may present in reactions which include but are not limited to: intrusive or dissociative symptoms, and reactivity symptoms such as avoidance or arousal. Reactions may be exhibited for days or weeks after the traumatic event.
Dissociative disorders (DD) are conditions that involve significant disruptions and/or breakdowns "in the normal integration of consciousness, memory, identity, emotion, perception, body representation, motor control, and behavior." People with dissociative disorders also use dissociation as a defense mechanism involuntarily. The individual experiences these dissociations to protect themselves from traumatic stress. Some dissociative disorders are triggered by significant psychological trauma, though depersonalization-derealization disorder may be preceded by lesser stress, psychoactive substances, or no identifiable trigger at all.
Reduced affect display, sometimes referred to as emotional blunting or emotional numbing, is a condition of reduced emotional reactivity in an individual. It manifests as a failure to express feelings either verbally or nonverbally, especially when talking about issues that would normally be expected to engage emotions. In this condition, expressive gestures are rare and there is little animation in facial expression or vocal inflection. Additionally, reduced affect can be symptomatic of autism, schizophrenia, depression, post-traumatic stress disorder, depersonalization disorder, schizoid personality disorder or brain damage. It may also be a side effect of certain medications.
A major depressive episode (MDE) is a period characterized by symptoms of major depressive disorder. Those affected primarily exhibit a depressive mood for at least two weeks or more, and a loss of interest or pleasure in everyday activities. Other symptoms can include feelings of emptiness, hopelessness, anxiety, worthlessness, guilt, irritability, changes in appetite, difficulties in concentration, difficulties remembering details, making decisions, and thoughts of suicide. Insomnia or hypersomnia and aches, pains, or digestive problems that are resistant to treatment may also be present.
Multiple complex developmental disorder (MCDD) is a research category, proposed to involve several neurological and psychological symptoms where at least some symptoms are first noticed during early childhood and persist throughout life. It was originally suggested to be a subtype of pervasive developmental disorders (PDD) with co-morbid schizophrenia or another psychotic disorder; however, there is some controversy that not everyone with MCDD meets criteria for both PDD and psychosis. The term multiplex developmental disorder was coined by Donald J. Cohen in 1986.
Derealization is an alteration in the perception of the external world, causing those with the condition to perceive it as unreal, distant, distorted or falsified. Other symptoms include feeling as if one's environment is lacking in spontaneity, emotional coloring, and depth. It is a dissociative symptom that may appear in moments of severe stress.
Thought blocking is a neuropsychological symptom expressing a sudden and involuntary silence within a speech, and eventually an abrupt switch to another topic. Persons undergoing thought blocking may utter incomprehensible speech; they may also repeat words involuntarily or make up new words. The main causes of thought blocking are schizophrenia, anxiety disorders, petit mal seizures, post-traumatic stress disorder, bradyphrenia, aphasia, dementia and delirium.
Pseudoneurotic schizophrenia is a postulated mental disorder categorized by the presence of two or more symptoms of mental illness such as anxiety, hysteria, and phobic or obsessive-compulsive neuroses. It is often acknowledged as a personality disorder. Patients generally display salient anxiety symptoms that disguise an underlying psychotic disorder.
PTSD or post-traumatic stress disorder, is a psychiatric disorder characterised by intrusive thoughts and memories, dreams or flashbacks of the event; avoidance of people, places and activities that remind the individual of the event; ongoing negative beliefs about oneself or the world, mood changes and persistent feelings of anger, guilt or fear; alterations in arousal such as increased irritability, angry outbursts, being hypervigilant, or having difficulty with concentration and sleep.
Cognitive emotional behavioral therapy (CEBT) is an extended version of cognitive behavioral therapy (CBT) aimed at helping individuals to evaluate the basis of their emotional distress and thus reduce the need for associated dysfunctional coping behaviors. This psychotherapeutic intervention draws on a range of models and techniques including dialectical behavior therapy (DBT), mindfulness meditation, acceptance and commitment therapy (ACT), and experiential exercises.