Dietary fiber or roughage is the portion of plant-derived food that cannot be completely broken down by human digestive enzymes. Dietary fibers are diverse in chemical composition, and can be grouped generally by their solubility, viscosity, and fermentability, which affect how fibers are processed in the body. Dietary fiber has two main components: soluble fiber and insoluble fiber, which are components of plant-based foods, such as legumes, whole grains and cereals, vegetables, fruits, and nuts or seeds. A diet high in regular fiber consumption is generally associated with supporting health and lowering the risk of several diseases. Dietary fiber consists of non-starch polysaccharides and other plant components such as cellulose, resistant starch, resistant dextrins, inulin, lignins, chitins, pectins, beta-glucans, and oligosaccharides.

Fecal incontinence (FI), or in some forms, encopresis, is a lack of control over defecation, leading to involuntary loss of bowel contents, both liquid stool elements and mucus, or solid feces. When this loss includes flatus (gas), it is referred to as anal incontinence. FI is a sign or a symptom, not a diagnosis. Incontinence can result from different causes and might occur with either constipation or diarrhea. Continence is maintained by several interrelated factors, including the anal sampling mechanism, and incontinence usually results from a deficiency of multiple mechanisms. The most common causes are thought to be immediate or delayed damage from childbirth, complications from prior anorectal surgery, altered bowel habits. An estimated 2.2% of community-dwelling adults are affected. However, reported prevalence figures vary. A prevalence of 8.39% among non-institutionalized U.S adults between 2005 and 2010 has been reported, and among institutionalized elders figures come close to 50%.

Fart lighting, also known as pyroflatulence or flatus ignition, is the practice of igniting the gases produced by flatulence. The resulting flame is often of a blue hue hence the act being known colloquially as a "blue angel", "blue dart" or in Australia, a "blue flame". The fact that flatus is flammable and the actual combustion of it through this practice gives rise to much humorous derivation. Other colors of flame such as orange and yellow are possible depending on the mixture of gases formed in the colon.

Irritable bowel syndrome (IBS) is a functional gastrointestinal disorder characterized by a group of symptoms that commonly include abdominal pain, abdominal bloating and changes in the consistency of bowel movements. These symptoms may occur over a long time, sometimes for years. IBS can negatively affect quality of life and may result in missed school or work or reduced productivity at work. Disorders such as anxiety, major depression, and chronic fatigue syndrome are common among people with IBS.
Fructose malabsorption, formerly named dietary fructose intolerance (DFI), is a digestive disorder in which absorption of fructose is impaired by deficient fructose carriers in the small intestine's enterocytes. This results in an increased concentration of fructose. Intolerance to fructose was first identified and reported in 1956.
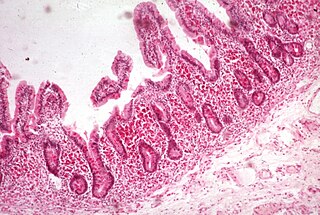
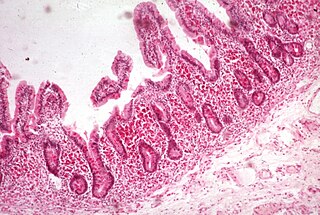
Malabsorption is a state arising from abnormality in absorption of food nutrients across the gastrointestinal (GI) tract. Impairment can be of single or multiple nutrients depending on the abnormality. This may lead to malnutrition and a variety of anaemias.
Functional gastrointestinal disorders (FGID), also known as disorders of gut–brain interaction, include a number of separate idiopathic disorders which affect different parts of the gastrointestinal tract and involve visceral hypersensitivity and motility disturbances.

Ileus is a disruption of the normal propulsive ability of the intestine. It can be caused by lack of peristalsis or by mechanical obstruction. The word 'ileus' is from Ancient Greek eileós. The term 'subileus' refers to a partial obstruction.

Small intestinal bacterial overgrowth (SIBO), also termed bacterial overgrowth, or small bowel bacterial overgrowth syndrome (SBBOS), is a disorder of excessive bacterial growth in the small intestine. Unlike the colon, which is rich with bacteria, the small bowel usually has fewer than 100,000 organisms per millilitre. Patients with bacterial overgrowth typically develop symptoms which may include nausea, bloating, vomiting, diarrhea, malnutrition, weight loss and malabsorption, which is caused by a number of mechanisms.

Lactulose is a non-absorbable sugar used in the treatment of constipation and hepatic encephalopathy. It is administered orally for constipation, and either orally or rectally for hepatic encephalopathy. It generally begins working after 8–12 hours, but may take up to 2 days to improve constipation.
Abdominal bloating is a short-term disease that affects the gastrointestinal tract. Bloating is generally characterized by an excess buildup of gas, air or fluids in the stomach. A person may have feelings of tightness, pressure or fullness in the stomach; it may or may not be accompanied by a visibly distended abdomen. Bloating can affect anyone of any age range and is usually self-diagnosed, in most cases does not require serious medical attention or treatment. Although this term is usually used interchangeably with abdominal distension, these symptoms probably have different pathophysiological processes, which are not fully understood.

Abdominal distension occurs when substances, such as air (gas) or fluid, accumulate in the abdomen causing its expansion. It is typically a symptom of an underlying disease or dysfunction in the body, rather than an illness in its own right. People with this condition often describe it as "feeling bloated". Affected people often experience a sensation of fullness, abdominal pressure, and sometimes nausea, pain, or cramping. In the most extreme cases, upward pressure on the diaphragm and lungs can also cause shortness of breath. Through a variety of causes, bloating is most commonly due to buildup of gas in the stomach, small intestine, or colon. The pressure sensation is often relieved, or at least lessened, by belching or flatulence. Medications that settle gas in the stomach and intestines are also commonly used to treat the discomfort and lessen the abdominal distension.
A hydrogen breath test is used as a diagnostic tool for small intestine bacterial overgrowth and carbohydrate malabsorption, such as lactose, fructose, and sorbitol malabsorption.

Rifaximin, is a non-absorbable, broad spectrum antibiotic mainly used to treat travelers' diarrhea. It is based on the rifamycin antibiotics family. Since its approval in Italy in 1987, it has been licensed in over more than 30 countries for the treatment of a variety of gastrointestinal diseases like irritable bowel syndrome, and hepatic encephalopathy. It acts by inhibiting RNA synthesis in susceptible bacteria by binding to the RNA polymerase enzyme. This binding blocks translocation, which stops transcription. It is marketed under the brand name Xifaxan by Salix Pharmaceuticals.
The gastrocolic reflex or gastrocolic response is a physiological reflex that controls the motility, or peristalsis, of the gastrointestinal tract following a meal. It involves an increase in motility of the colon consisting primarily of giant migrating contractions, or migrating motor complexes, in response to stretch in the stomach following ingestion and byproducts of digestion entering the small intestine. Thus, this reflex is responsible for the urge to defecate following a meal. The small intestine also shows a similar motility response. The gastrocolic reflex's function in driving existing intestinal contents through the digestive system helps make way for ingested food.

Polycarbophil calcium (INN) is a drug used as a stool stabilizer. Chemically, it is a synthetic polymer of polyacrylic acid cross-linked with divinyl glycol, with calcium as a counter-ion.
Jejunoileal bypass (JIB) was a surgical weight-loss procedure performed for the relief of morbid obesity from the 1950s through the 1970s in which all but 30 cm (12 in) to 45 cm (18 in) of the small bowel were detached and set to the side.

Human feces are the solid or semisolid remains of food that could not be digested or absorbed in the small intestine of humans, but has been further broken down by bacteria in the large intestine. It also contains bacteria and a relatively small amount of metabolic waste products such as bacterially altered bilirubin, and the dead epithelial cells from the lining of the gut. It is discharged through the anus during a process called defecation.
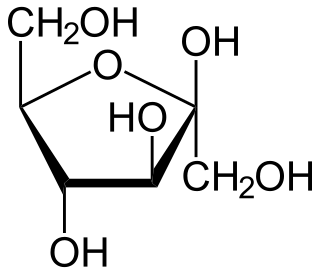
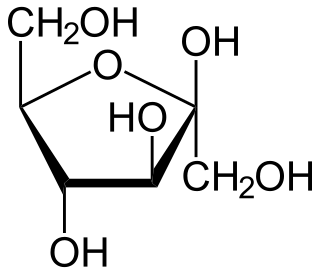
FODMAPs or fermentable oligosaccharides, disaccharides, monosaccharides, and polyols are short-chain carbohydrates that are poorly absorbed in the small intestine and ferment in the colon. They include short-chain oligosaccharide polymers of fructose (fructans) and galactooligosaccharides, disaccharides (lactose), monosaccharides (fructose), and sugar alcohols (polyols), such as sorbitol, mannitol, xylitol, and maltitol. Most FODMAPs are naturally present in food and the human diet, but the polyols may be added artificially in commercially prepared foods and beverages.
A low-FODMAP diet is a person's global restriction of consumption of all fermentable carbohydrates (FODMAPs), recommended only for a short time. A low-FODMAP diet is recommended for managing patients with irritable bowel syndrome (IBS) and can reduce digestive symptoms of IBS including bloating and flatulence.