A syringe is a simple reciprocating pump consisting of a plunger that fits tightly within a cylindrical tube called a barrel. The plunger can be linearly pulled and pushed along the inside of the tube, allowing the syringe to take in and expel liquid or gas through a discharge orifice at the front (open) end of the tube. The open end of the syringe may be fitted with a hypodermic needle, a nozzle or tubing to direct the flow into and out of the barrel. Syringes are frequently used in clinical medicine to administer injections, infuse intravenous therapy into the bloodstream, apply compounds such as glue or lubricant, and draw/measure liquids. There are also prefilled syringes.

Intravenous therapy is a medical technique that administers fluids, medications and nutrients directly into a person's vein. The intravenous route of administration is commonly used for rehydration or to provide nutrients for those who cannot, or will not—due to reduced mental states or otherwise—consume food or water by mouth. It may also be used to administer medications or other medical therapy such as blood products or electrolytes to correct electrolyte imbalances. Attempts at providing intravenous therapy have been recorded as early as the 1400s, but the practice did not become widespread until the 1900s after the development of techniques for safe, effective use.

A hypodermic needle, one of a category of medical tools which enter the skin, called sharps, is a very thin, hollow tube with one sharp tip. It is commonly used with a syringe, a hand-operated device with a plunger, to inject substances into the body or extract fluids from the body. Large-bore hypodermic intervention is especially useful in catastrophic blood loss or treating shock.

In pharmacology and toxicology, a route of administration is the way by which a drug, fluid, poison, or other substance is taken into the body.

Subcutaneous administration is the insertion of medications beneath the skin either by injection or infusion.

Intramuscular injection, often abbreviated IM, is the injection of a substance into a muscle. In medicine, it is one of several methods for parenteral administration of medications. Intramuscular injection may be preferred because muscles have larger and more numerous blood vessels than subcutaneous tissue, leading to faster absorption than subcutaneous or intradermal injections. Medication administered via intramuscular injection is not subject to the first-pass metabolism effect which affects oral medications.
Needle sharing is the practice of intravenous drug-users by which a needle or syringe is shared by multiple individuals to administer intravenous drugs such as heroin, steroids, and hormones. This is a primary vector for blood-borne diseases which can be transmitted through blood. People who inject drugs (PWID) are at an increased risk for Hepatitis C (HCV) and HIV due to needle sharing practices. From 1933 to 1943, malaria was spread between users in the New York City area by this method. Afterwards, the use of quinine as a cutting agent in drug mixes became more common. Harm reduction efforts including safe disposal of needles, supervised injection sites, and public education may help bring awareness on safer needle sharing practices.

Oxymorphone is a highly potent opioid analgesic indicated for treatment of severe pain. Pain relief after injection begins after about 5–10 minutes, after oral administration it begins after about 30 minutes, and lasts about 3–4 hours for immediate-release tablets and 12 hours for extended-release tablets. The elimination half-life of oxymorphone is much faster intravenously, and as such, the drug is most commonly used orally. Like oxycodone, which metabolizes to oxymorphone, oxymorphone has a high potential to be abused.

A jet injector is a type of medical injecting syringe device used for a method of drug delivery known as jet injection. A narrow, high-pressure stream of liquid is made to penetrate the outermost layer of the skin to deliver medication to targeted underlying tissues of the epidermis or dermis, fat, or muscle.

Black tar heroin, also known as black dragon, is a form of heroin that is sticky like tar or hard like coal. Its dark color is the result of crude processing methods that leave behind impurities. Despite its name, black tar heroin can also be dark orange or dark brown in appearance.

A needlestick injury is the penetration of the skin by a hypodermic needle or other sharp object that has been in contact with blood, tissue or other body fluids before the exposure. Even though the acute physiological effects of a needlestick injury are generally negligible, these injuries can lead to transmission of blood-borne diseases, placing those exposed at increased risk of infection from disease-causing pathogens, such as the hepatitis B virus (HBV), hepatitis C virus (HCV), and human immunodeficiency virus (HIV). Among healthcare workers and laboratory personnel worldwide, more than 25 blood-borne virus infections have been reported to have been caused by needlestick injuries. In addition to needlestick injuries, transmission of these viruses can also occur as a result of contamination of the mucous membranes, such as those of the eyes, with blood or body fluids, but needlestick injuries make up more than 80% of all percutaneous exposure incidents in the United States. Various other occupations are also at increased risk of needlestick injury, including law enforcement, laborers, tattoo artists, food preparers, and agricultural workers.

Sharps waste is a form of biomedical waste composed of used "sharps", which includes any device or object used to puncture or lacerate the skin. Sharps waste is classified as biohazardous waste and must be carefully handled. Common medical materials treated as sharps waste are hypodermic needles, disposable scalpels and blades, contaminated glass and certain plastics, and guidewires used in surgery.

Drug injection is a method of introducing a drug into the bloodstream via a hollow hypodermic needle, which is pierced through the skin into the body. Intravenous therapy, a form of drug injection, is universally practiced in modernized medical care. As of 2004, there were 13.2 million people worldwide who self-administered injection drugs outside of medical supervision, of which 22% are from developed countries.
Dosage forms are pharmaceutical drug products in the form in which they are marketed for use, with a specific mixture of active ingredients and inactive components (excipients), in a particular configuration, and apportioned into a particular dose. For example, two products may both be amoxicillin, but one is in 500 mg capsules and another is in 250 mg chewable tablets. The term unit dose can also sometimes encompass non-reusable packaging as well, although the FDA distinguishes that by unit-dose "packaging" or "dispensing". Depending on the context, multi(ple) unit dose can refer to distinct drug products packaged together, or to a single drug product containing multiple drugs and/or doses. The term dosage form can also sometimes refer only to the pharmaceutical formulation of a drug product's constituent drug substance(s) and any blends involved, without considering matters beyond that. Because of the somewhat vague boundaries and unclear overlap of these terms and certain variants and qualifiers within the pharmaceutical industry, caution is often advisable when conversing with someone who may be unfamiliar with another person's use of the term.
Veterinary anesthesia is a specialization in the veterinary medicine field dedicated to the proper administration of anesthetic agents to non-human animals to control their consciousness during procedures. A veterinarian or a Registered Veterinary Technician administers these drugs to minimize stress, destructive behavior, and the threat of injury to both the patient and the doctor. The duration of the anesthesia process goes from the time before an animal leaves for the visit to the time after the animal reaches home after the visit, meaning it includes care from both the owner and the veterinary staff. Generally, anesthesia is used for a wider range of circumstances in animals than in people not only due to their inability to cooperate with certain diagnostic or therapeutic procedures, but also due to their species, breed, size, and corresponding anatomy. Veterinary anesthesia includes anesthesia of the major species: dogs, cats, horses, cattle, sheep, goats, and pigs, as well as all other animals requiring veterinary care such as birds, pocket pets, and wildlife.
Skin popping is a route of administration of street drugs where they are injected or deposited under the skin. It is usually a depot injection, either subcutaneous or intradermal, and not an intramuscular injection. After deposition, the drug then diffuses slowly from the depot into the capillary networks, where it enters circulation. Skin popping is distinct from intravenous injection in that the latter deposits the drug directly into the bloodstream via a vein. Nonetheless, it is included with IV injection in the category of injection drug use because both involve injection, both are often done with the same drugs, and both carry many of the same risks. Higher-potency prescription opioids, such as morphine, fentanyl, or meperidine can be injected subcutaneously, as can cocaine. Skin popping increases the duration of the high one gets from drugs such as cocaine. The sites where skin popping with cocaine has been performed have an area of central pallor surrounded by bruising (ecchymosis). This pattern is due to the vasoconstrictive properties of cocaine acting locally at the injection site with hemorrhage occurring in the surrounding tissue. Skin popping puts one at risk for developing secondary amyloid associated (AA) amyloidosis. Tetanus has also been associated with skin-popping as has botulism.
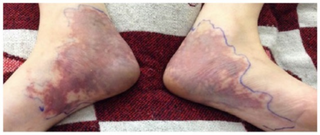
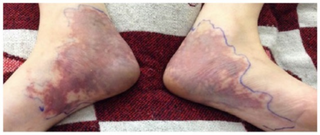
Livedoid dermatitis is a iatrogenic cutaneous reaction that occurs immediately after a drug injection. It presents as an immediate, extreme pain around the injection site, with overlying skin rapidly becoming erythematous, violaceous, or blanched and sometimes with reticular pattern. The reaction eventually leads to variable degrees of necrosis to the skin and underlying tissue. The wound eventually heals, but can lead to atrophic, disfiguring scarring.
Injection site reactions (ISRs) are reactions that occur at the site of injection of a drug. They may be mild or severe and may or may not require medical intervention. Some reactions may appear immediately after injection, and some may be delayed. Such reactions can occur with subcutaneous, intramuscular, or intravenous administration.

Intradermal injection is a shallow or superficial injection of a substance into the dermis, which is located between the epidermis and the hypodermis. For certain substances, administration via an ID route can result in a faster systemic uptake compared with subcutaneous injections, leading to a stronger immune response to vaccinations, immunology and novel cancer treatments, and faster drug uptake. Additionally, since administration is closer to the surface of the skin, the body's reaction to substances is more easily visible. However, due to complexity of the procedure compared to subcutaneous injection and intramuscular injection, administration via ID is relatively rare, and is only used for tuberculosis and allergy tests, Monkeypox vaccination, and certain therapies.

An injector pen is a device used for injecting medication under the skin. First introduced in the 1980s, injector pens are designed to make injectable medication easier and more convenient to use, thus increasing patient adherence. The primary difference between injector pens and traditional vial and syringe administration is the easier use of an injector pen by people with low dexterity, poor vision, or who need portability to administer medicine on time. Injector pens also decrease the fear or adversity towards self-injection of medications, which increases the likelihood that a person takes the medication.