Cerebrospinal fluid (CSF) is a clear, colorless body fluid found within the tissue that surrounds the brain and spinal cord of all vertebrates.

Syringomyelia is a generic term referring to a disorder in which a cyst or cavity forms within the spinal cord. Often, syringomyelia is used as a generic term before an etiology is determined. This cyst, called a syrinx, can expand and elongate over time, destroying the spinal cord. The damage may result in loss of feeling, paralysis, weakness, and stiffness in the back, shoulders, and extremities. Syringomyelia may also cause a loss of the ability to feel extremes of hot or cold, especially in the hands. It may also lead to a cape-like bilateral loss of pain and temperature sensation along the upper chest and arms. The combination of symptoms varies from one patient to another depending on the location of the syrinx within the spinal cord, as well as its extent.

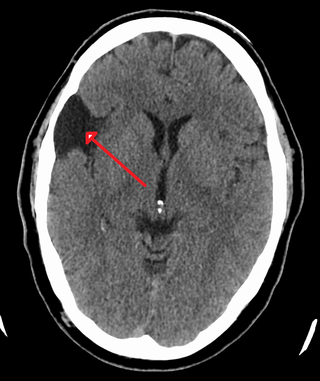
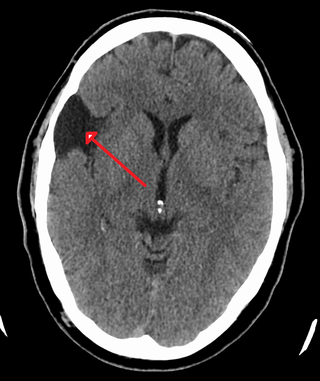
A brain tumor occurs when abnormal cells form within the brain. There are two main types of tumors: malignant tumors and benign (non-cancerous) tumors. These can be further classified as primary tumors, which start within the brain, and secondary tumors, which most commonly have spread from tumors located outside the brain, known as brain metastasis tumors. All types of brain tumors may produce symptoms that vary depending on the size of the tumor and the part of the brain that is involved. Where symptoms exist, they may include headaches, seizures, problems with vision, vomiting and mental changes. Other symptoms may include difficulty walking, speaking, with sensations, or unconsciousness.

Viral meningitis, also known as aseptic meningitis, is a type of meningitis due to a viral infection. It results in inflammation of the meninges. Symptoms commonly include headache, fever, sensitivity to light and neck stiffness.

Lumbar puncture (LP), also known as a spinal tap, is a medical procedure in which a needle is inserted into the spinal canal, most commonly to collect cerebrospinal fluid (CSF) for diagnostic testing. The main reason for a lumbar puncture is to help diagnose diseases of the central nervous system, including the brain and spine. Examples of these conditions include meningitis and subarachnoid hemorrhage. It may also be used therapeutically in some conditions. Increased intracranial pressure is a contraindication, due to risk of brain matter being compressed and pushed toward the spine. Sometimes, lumbar puncture cannot be performed safely. It is regarded as a safe procedure, but post-dural-puncture headache is a common side effect if a small atraumatic needle is not used.

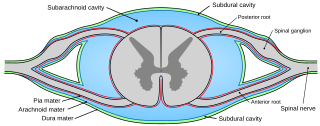
In anatomy, the meninges are the three membranes that envelop the brain and spinal cord. In mammals, the meninges are the dura mater, the arachnoid mater, and the pia mater. Cerebrospinal fluid is located in the subarachnoid space between the arachnoid mater and the pia mater. The primary function of the meninges is to protect the central nervous system.
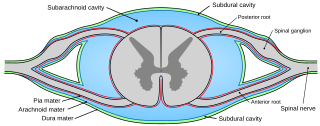
Pia mater, often referred to as simply the pia, is the delicate innermost layer of the meninges, the membranes surrounding the brain and spinal cord. Pia mater is medieval Latin meaning "tender mother". The other two meningeal membranes are the dura mater and the arachnoid mater. Both the pia and arachnoid mater are derivatives of the neural crest while the dura is derived from embryonic mesoderm. The pia mater is a thin fibrous tissue that is permeable to water and small solutes. The pia mater allows blood vessels to pass through and nourish the brain. The perivascular space between blood vessels and pia mater is proposed to be part of a pseudolymphatic system for the brain. When the pia mater becomes irritated and inflamed the result is meningitis.

The crown is the top portion of the head behind the vertex. The anatomy of the crown varies between different organisms. The human crown is made of three layers of the scalp above the skull. The crown also covers a range of bone sutures, and contains blood vessels and branches of the trigeminal nerve.

Aseptic meningitis is the inflammation of the meninges, a membrane covering the brain and spinal cord, in patients whose cerebral spinal fluid test result is negative with routine bacterial cultures. Aseptic meningitis is caused by viruses, mycobacteria, spirochetes, fungi, medications, and cancer malignancies. The testing for both meningitis and aseptic meningitis is mostly the same. A cerebrospinal fluid sample is taken by lumbar puncture and is tested for leukocyte levels to determine if there is an infection and goes on to further testing to see what the actual cause is. The symptoms are the same for both meningitis and aseptic meningitis but the severity of the symptoms and the treatment can depend on the certain cause.

The cranial cavity, also known as intracranial space, is the space within the skull that accommodates the brain. The skull minus the mandible is called the cranium. The cavity is formed by eight cranial bones known as the neurocranium that in humans includes the skull cap and forms the protective case around the brain. The remainder of the skull is called the facial skeleton. Meninges are protective membranes that surround the brain to minimize damage to the brain in the case of head trauma. Meningitis is the inflammation of meninges caused by bacterial or viral infections.

Neurosyphilis is the infection of the central nervous system in a patient with syphilis. In the era of modern antibiotics, the majority of neurosyphilis cases have been reported in HIV-infected patients. Meningitis is the most common neurological presentation in early syphilis. Tertiary syphilis symptoms are exclusively neurosyphilis, though neurosyphilis may occur at any stage of infection.

Tuberculous meningitis, also known as TB meningitis or tubercular meningitis, is a specific type of bacterial meningitis caused by the Mycobacterium tuberculosis infection of the meninges—the system of membranes which envelop the central nervous system.

Mollaret's meningitis is a recurrent or chronic inflammation of the protective membranes covering the brain and spinal cord, known collectively as the meninges. Since Mollaret's meningitis is a recurrent, benign (non-cancerous), aseptic meningitis, it is also referred to as benign recurrent lymphocytic meningitis. It was named for Pierre Mollaret, the French neurologist who first described it in 1944.

Meningitis is acute or chronic inflammation of the protective membranes covering the brain and spinal cord, collectively called the meninges. The most common symptoms are fever, intense headache, vomiting and neck stiffness and occasionally photophobia.

A cerebrospinal fluid leak is a medical condition where the cerebrospinal fluid (CSF) surrounding the brain or spinal cord leaks out of one or more holes or tears in the dura mater. A cerebrospinal fluid leak can be either cranial or spinal, and these are two different disorders. A spinal CSF leak can be caused by one or more meningeal diverticula or CSF-venous fistulas not associated with an epidural leak.
A central nervous system cyst is a type of cyst that presents and affects part of the central nervous system (CNS). They are usually benign and filled with either cerebrospinal fluid, blood, or tumor cells. CNS cysts are classified into two categories: cysts that originate from non-central nervous system tissue, migrate to, and form on a portion of the CNS, and cysts that originate within central nervous system tissue itself. Within these two categories, there are many types of CNS cysts that have been identified from previous studies.

Tarlov cysts, are type II innervated meningeal cysts, cerebrospinal-fluid-filled (CSF) sacs most frequently located in the spinal canal of the sacral region of the spinal cord (S1–S5) and much less often in the cervical, thoracic or lumbar spine. They can be distinguished from other meningeal cysts by their nerve-fiber-filled walls. Tarlov cysts are defined as cysts formed within the nerve-root sheath at the dorsal root ganglion. The etiology of these cysts is not well understood; some current theories explaining this phenomenon have not yet been tested or challenged but include increased pressure in CSF, filling of congenital cysts with one-way valves, inflammation in response to trauma and disease. They are named for American neurosurgeon Isadore Tarlov, who described them in 1938.
Superficial hemosiderosis of the central nervous system is a disease of the brain resulting from chronic iron deposition in neuronal tissues associated with cerebrospinal fluid. This occurs via the deposition of hemosiderin in neuronal tissue, and is associated with neuronal loss, gliosis, and demyelination of neuronal cells. This disease was first discovered in 1908 by R.C. Hamill after performing an autopsy. Detection of this disease was largely post-mortem until the advent of MRI technology, which made diagnosis far easier. Superficial siderosis is largely considered a rare disease, with less than 270 total reported cases in scientific literature as of 2006, and affects people of a wide range of ages with men being approximately three times more frequently affected than women. The number of reported cases of superficial siderosis has increased with advances in MRI technology, but it remains a rare disease.
Neuro-oncology is the study of brain and spinal cord neoplasms, many of which are very dangerous and life-threatening. Among the malignant brain cancers, gliomas of the brainstem and pons, glioblastoma multiforme, and high-grade astrocytoma/oligodendroglioma are among the worst. In these cases, untreated survival usually amounts to only a few months, and survival with current radiation and chemotherapy treatments may extend that time from around a year to a year and a half, possibly two or more, depending on the patient's condition, immune function, treatments used, and the specific type of malignant brain neoplasm. Surgery may in some cases be curative, but, as a general rule, malignant brain cancers tend to regenerate and emerge from remission easily, especially highly malignant cases. In such cases, the goal is to excise as much of the mass and as much of the tumor margin as possible without endangering vital functions or other important cognitive abilities. The Journal of Neuro-Oncology is the longest continuously published journal in the field and serves as a leading reference to those practicing in the area of neuro-oncology.
Cancer pain can be caused by pressure on, or chemical stimulation of, specialised pain-signalling nerve endings called nociceptors, or by damage or illness affecting nerve fibers themselves.