Related Research Articles

Coronary artery disease (CAD), also called coronary heart disease (CHD), ischemic heart disease (IHD), myocardial ischemia, or simply heart disease, involves the reduction of blood flow to the cardiac muscle due to build-up of atherosclerotic plaque in the arteries of the heart. It is the most common of the cardiovascular diseases. Types include stable angina, unstable angina, and myocardial infarction.
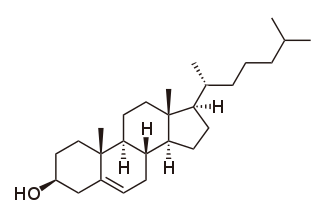
Cholesterol is the principal sterol of all higher animals, distributed in body tissues, especially the brain and spinal cord, and in animal fats and oils.
High-density lipoprotein (HDL) is one of the five major groups of lipoproteins. Lipoproteins are complex particles composed of multiple proteins which transport all fat molecules (lipids) around the body within the water outside cells. They are typically composed of 80–100 proteins per particle. HDL particles enlarge while circulating in the blood, aggregating more fat molecules and transporting up to hundreds of fat molecules per particle.

Low-density lipoprotein (LDL) is one of the five major groups of lipoprotein that transport all fat molecules around the body in extracellular water. These groups, from least dense to most dense, are chylomicrons, very low-density lipoprotein (VLDL), intermediate-density lipoprotein (IDL), low-density lipoprotein (LDL) and high-density lipoprotein (HDL). LDL delivers fat molecules to cells. LDL is involved in atherosclerosis, a process in which it is oxidized within the walls of arteries.

Atherosclerosis is a pattern of the disease arteriosclerosis, characterized by development of abnormalities called lesions in walls of arteries. These lesions may lead to narrowing of the arterial walls due to buildup of atheromatous plaques. At onset there are usually no symptoms, but if they develop, symptoms generally begin around middle age. In severe cases, it can result in coronary artery disease, stroke, peripheral artery disease, or kidney disorders, depending on which body part(s) the affected arteries are located in the body.

Ancel Benjamin Keys was an American physiologist who studied the influence of diet on health. In particular, he hypothesized that replacing dietary saturated fat with polyunsaturated fat reduced cardiovascular heart disease. Modern dietary recommendations by health organizations, systematic reviews, and national health agencies corroborate this.

Statins are a class of medications that reduce illness and mortality in people who are at high risk of cardiovascular disease. They are the most commonly prescribed cholesterol-lowering drugs.

Cardiovascular disease (CVD) is any disease involving the heart or blood vessels. CVDs constitute a class of diseases that includes: coronary artery diseases, heart failure, hypertensive heart disease, rheumatic heart disease, cardiomyopathy, arrhythmia, congenital heart disease, valvular heart disease, carditis, aortic aneurysms, peripheral artery disease, thromboembolic disease, and venous thrombosis.

Hypercholesterolemia, also called high cholesterol, is the presence of high levels of cholesterol in the blood. It is a form of hyperlipidemia, hyperlipoproteinemia, and dyslipidemia.
Dyslipidemia is a metabolic disorder characterized by abnormally high or low amounts of any or all lipids or lipoproteins in the blood. Dyslipidemia is a risk factor for the development of atherosclerotic cardiovascular diseases (ASCVD), which include coronary artery disease, cerebrovascular disease, and peripheral artery disease. Although dyslipidemia is a risk factor for ASCVD, abnormal levels don't mean that lipid lowering agents need to be started. Other factors, such as comorbid conditions and lifestyle in addition to dyslipidemia, is considered in a cardiovascular risk assessment. In developed countries, most dyslipidemias are hyperlipidemias; that is, an elevation of lipids in the blood. This is often due to diet and lifestyle. Prolonged elevation of insulin resistance can also lead to dyslipidemia. Likewise, increased levels of O-GlcNAc transferase (OGT) may cause dyslipidemia.
Hyperlipidemia is abnormally high levels of any or all lipids or lipoproteins in the blood. The term hyperlipidemia refers to the laboratory finding itself and is also used as an umbrella term covering any of various acquired or genetic disorders that result in that finding. Hyperlipidemia represents a subset of dyslipidemia and a superset of hypercholesterolemia. Hyperlipidemia is usually chronic and requires ongoing medication to control blood lipid levels.
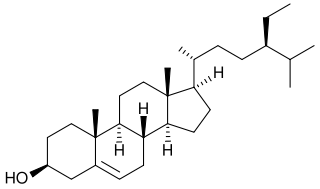
Phytosterols are phytosteroids, similar to cholesterol, that serve as structural components of biological membranes of plants. They encompass plant sterols and stanols. More than 250 sterols and related compounds have been identified. Free phytosterols extracted from oils are insoluble in water, relatively insoluble in oil, and soluble in alcohols.

Familial hypercholesterolemia (FH) is a genetic disorder characterized by high cholesterol levels, specifically very high levels of low-density lipoprotein cholesterol, in the blood and early cardiovascular diseases. The most common mutations diminish the number of functional LDL receptors in the liver or produce abnormal LDL receptors that never go to the cell surface to function properly. Since the underlying body biochemistry is slightly different in individuals with FH, their high cholesterol levels are less responsive to the kinds of cholesterol control methods which are usually more effective in people without FH. Nevertheless, treatment is usually effective.

Lipoprotein(a) is a low-density lipoprotein variant containing a protein called apolipoprotein(a). Genetic and epidemiological studies have identified lipoprotein(a) as a risk factor for atherosclerosis and related diseases, such as coronary heart disease and stroke.

Proprotein convertase subtilisin/kexin type 9 (PCSK9) is an enzyme encoded by the PCSK9 gene in humans on chromosome 1. It is the 9th member of the proprotein convertase family of proteins that activate other proteins. Similar genes (orthologs) are found across many species. As with many proteins, PCSK9 is inactive when first synthesized, because a section of peptide chains blocks their activity; proprotein convertases remove that section to activate the enzyme. The PCSK9 gene also contains one of 27 loci associated with increased risk of coronary artery disease.
The chronic endothelial injury hypothesis is one of two major mechanisms postulated to explain the underlying cause of atherosclerosis and coronary heart disease (CHD), the other being the lipid hypothesis. Although an ongoing debate involving connection between dietary lipids and CHD sometimes portrays the two hypotheses as being opposed, they are in no way mutually exclusive. Moreover, since the discovery of the role of LDL cholesterol (LDL-C) in the pathogenesis of atherosclerosis, the two hypotheses have become tightly linked by a number of molecular and cellular processes.

The Seven Countries Study is an epidemiological longitudinal study directed by Ancel Keys at what is today the University of Minnesota Laboratory of Physiological Hygiene & Exercise Science (LPHES). Begun in 1956 with a yearly grant of US$200,000 from the U.S. Public Health Service, the study was first published in 1978 and then followed up on its subjects every five years thereafter.

Evacetrapib was a drug under development by Eli Lilly & Company that inhibits cholesterylester transfer protein. CETP collects triglycerides from very low-density lipoproteins (VLDL) or low-density lipoproteins (LDL) and exchanges them for cholesteryl esters from high-density lipoproteins (HDL), and vice versa, but primarily increasing high-density lipoprotein and lowering low-density lipoprotein. It is thought that modifying lipoprotein levels modifies the risk of cardiovascular disease. The first CETP inhibitor, torcetrapib, was unsuccessful because it increased levels of the hormone aldosterone and increased blood pressure, which led to excess cardiac events when it was studied. Evacetrapib does not have the same effect. When studied in a small clinical trial in people with elevated LDL and low HDL, significant improvements were noted in their lipid profile.
Therapeutic Lifestyle Changes, also known as the TLC Diet, is a dietary pattern recommended by the National Cholesterol Education Program, part of the National Institutes of Health, to control hypercholesterolemia. This pattern focuses on saturated fats and cholesterol, dietary options to enhance LDL cholesterol lowering, weight control, and physical activity.
Remnant cholesterol, also known as remnant lipoprotein, is a very atherogenic lipoprotein composed primarily of very low-density lipoprotein (VLDL) and intermediate-density lipoprotein (IDL). Stated another way, remnant cholesterol is all plasma cholesterol that is not LDL cholesterol or HDL cholesterol, which are triglyceride-poor lipoproteins. However, remnant cholesterol is primarily chylomicron and VLDL, and each remnant particle contains about 40 times more cholesterol than LDL.
References
- ↑ Ahrens EH Jr (July 1976). "The management of hyperlipidemia: whether, rather than how". Ann Intern Med. 85 (1): 87–93. doi:10.7326/0003-4819-85-1-87. PMID 779574.
- ↑ Steinberg D (2006). "An interpretive history of the cholesterol controversy, part IV: The 1984 coronary primary prevention trial ends it - almost". J Lipid Res. 47 (1): 1–14. doi: 10.1194/jlr.R500014-JLR200 . PMID 16227628.
- 1 2 3 4 Ference BA, Ginsberg HN, Graham I, et al. (August 2017). "Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel". European Heart Journal. 38 (32): 2459–2472. doi:10.1093/eurheartj/ehx144. PMC 5837225 . PMID 28444290.
- ↑ Linton MF, Yancey PG, Davies SS, et al. (3 January 2019). "The Role of Lipids and Lipoproteins in Atherosclerosis". Endotext. PMID 26844337.
- ↑ Duarte Lau F, Giugliano RP (July 2022). "Lipoprotein(a) and its Significance in Cardiovascular Disease: A Review". JAMA Cardiology. 7 (7): 760–769. doi:10.1001/jamacardio.2022.0987. PMID 35583875.
- 1 2 "World Heart Report 2023: Confronting the World's Number One Killer" (PDF). World Heart Federation. 2023. Retrieved 22 January 2024.
- ↑ Virchow, Rudolf (1856). "Gesammelte Abhandlungen zur wissenschaftlichen Medizin". Vierteljahrschrift für die praktische Heilkunde. Germany: Staatsdruckerei Frankfurt. Phlogose und Thrombose im Gefäßsystem.
- ↑ Steinberg, Daniel (21 April 2004). "Thematic review series: The Pathogenesis of Atherosclerosis. An interpretive history of the cholesterol controversy: Part I". Journal of Lipid Research . 45 (9): 1583–1593. doi: 10.1194/jlr.R400003-JLR200 . PMID 15102877.
- ↑ Steinberg, Daniel (2013). "In celebration of the 100th anniversary of the lipid hypothesis of atherosclerosis". Journal of Lipid Research. 54 (11): 2946–2949. doi: 10.1194/jlr.R043414 . PMC 3793599 . PMID 23975896.
- 1 2 3 Blackburn, Henry (2012). "20th-Century "Medical Marco Polos" in the Origins of Preventive Cardiology and Cardiovascular Disease Epidemiology". The American Journal of Cardiology . 109 (5): 756–767. doi:10.1016/j.amjcard.2011.10.038. PMID 22470931.
- ↑ de Langen, Cornelis (1916). "Cholesterine-stofwisseling en rassenpathologie". Geneeskundig Tijdschrift voor Nederlandsch-Indie (in Dutch). 56: 1–34.
- ↑ Duff GL, McMillan GC (1951). "Pathology of atherosclerosis". Am J Med. 11 (1): 92–108. doi:10.1016/0002-9343(51)90011-3. PMID 14837929.
- 1 2 Keys, Ancel; Taylor, Henry Longstreet; Blackburn, Henry; et al. (1 September 1963). "Coronary Heart Disease among Minnesota Business and Professional Men Followed Fifteen Years". Circulation . 28 (3): 381–95. doi: 10.1161/01.cir.28.3.381 . PMID 14059458.
- ↑ Famous Polemics on Diet-Heart Theory. Henry Blackburn, School of Public Health, University of Minnesota. http://www.epi.umn.edu/cvdepi/essay.asp?id=33 accessed 18 March 2014
- ↑ Keys, Ancel (1980). Seven Countries: A Multivariate Analysis of Death and Coronary Heart Disease . Harvard University Press. ISBN 978-0-674-80237-7.
- ↑ Yerushalmy J, Hilleboe HE (1957). "Fat in the diet and mortality from heart disease. A methodologic note". NY State J Med. 57: 2343–54.
- ↑ "Dietary Fat and Its Relation to Heart Attacks and Strokes". JAMA . 175 (5): 389–391. 4 February 1961. doi:10.1001/jama.1961.63040050001011. PMID 14447694.
- ↑ "TIME Magazine Cover: Ancel Keys". TIME.com. 13 January 1961. Retrieved 23 July 2017.
- ↑ Keys A (Ed). Seven Countries: A multivariate analysis of death and coronary heart disease. Harvard University Press. Cambridge, Massachusetts. 1980. ISBN 0-674-80237-3.
- ↑ Keys, Ancel (1959). Eat Well and Stay Well. United States: Doubleday. ISBN 978-0-385-06575-7.
- ↑ "Ancel Keys Obituary". The American Physiological Society. Archived from the original on 27 September 2007. Retrieved 15 April 2007.
- ↑ Steinberg D (2006). "Thematic review series: the pathogenesis of atherosclerosis. An interpretive history of the cholesterol controversy, part V: the discovery of the statins and the end of the controversy". J. Lipid Res. 47 (7): 1339–51. doi: 10.1194/jlr.R600009-JLR200 . PMID 16585781.
- ↑ Steinberg D (1989). "The cholesterol controversy is over. Why did it take so long?". Circulation. 80 (4): 1070–1078. doi: 10.1161/01.cir.80.4.1070 . PMID 2676235.
- ↑ LaRosa JC (1998). "Cholesterol & atherosclerosis: a controversy resolved". Adv Nurse Pract. 6 (5): 36–37. PMID 9633288.
- ↑ Steinberg D (2002). "Atherogenesis in perspective: hypercholesterolemia and inflammation as partners in crime". Nature Medicine . 8 (11): 1211–1217. doi:10.1038/nm1102-1211. PMID 12411947. S2CID 30459713.
- ↑ Thompson GR, Packard CJ, Stone NJ (2002). "Goals of statin therapy: three viewpoints". Curr Atheroscler Rep. 4 (1): 26–33. doi:10.1007/s11883-002-0059-6. PMID 11772419. S2CID 72257114.
- ↑ Bucher, HC; Griffith, LE; Guyatt, GH (February 1999). "Systematic review on the risk and benefit of different cholesterol-lowering interventions". Arteriosclerosis, Thrombosis, and Vascular Biology. 19 (2): 187–195. doi: 10.1161/01.atv.19.2.187 . PMID 9974397.
- ↑ Tyroler HA (1987). "Review of lipid-lowering clinical trials in relation to observational epidemiologic studies". Circulation. 76 (3): 515–522. doi: 10.1161/01.cir.76.3.515 . PMID 3304704.
- ↑ Brown WV (1990). "Review of clinical trials: proving the lipid hypothesis". Eur Heart J. 11 Suppl H: 15–20. doi:10.1093/eurheartj/11.suppl_h.15. PMID 2073909.
- ↑ Kroon AA, Stalenhoef AF (1997). "LDL-cholesterol lowering and atherosclerosis -- clinical benefit and possible mechanisms: an update". Neth J Med. 51 (1): 16–27. doi:10.1016/S0300-2977(97)00031-4. hdl: 2066/26174 . PMID 9260486. S2CID 7075128.
- ↑ "The Lipid Hypothesis". lipid.org. Retrieved 22 January 2024.
- ↑ Ference BA, Graham I, Tokgozoglu L, Catapano AL (2018). "Impact of Lipids on Cardiovascular Health: JACC Health Promotion Series". Journal of the American College of Cardiology. 72 (10): 1141–1156. doi:10.1016/j.jacc.2018.06.046. PMID 30165986. S2CID 52136486.
- ↑ Pearson GJ, Thanassoulis G, Anderson TJ, et al. (August 2021). "2021 Canadian Cardiovascular Society Guidelines for the Management of Dyslipidemia for the Prevention of Cardiovascular Disease in Adults". The Canadian Journal of Cardiology. 37 (8): 1129–1150. doi:10.1016/j.cjca.2021.03.016. PMID 33781847.
- ↑ Kuijpers PM (13 January 2021). "History in medicine: the story of cholesterol, lipids and cardiology". e-Journal of Cardiology Practice. 18 (9).