Mycophenolic acid is an immunosuppressant medication used to prevent rejection following organ transplantation and to treat autoimmune conditions such as Crohn's disease and lupus. Specifically it is used following kidney, heart, and liver transplantation. It can be given by mouth or by injection into a vein. It comes as mycophenolate sodium and mycophenolate mofetil.

A desmosome, also known as a macula adherens, is a cell structure specialized for cell-to-cell adhesion. A type of junctional complex, they are localized spot-like adhesions randomly arranged on the lateral sides of plasma membranes. Desmosomes are one of the stronger cell-to-cell adhesion types and are found in tissue that experience intense mechanical stress, such as cardiac muscle tissue, bladder tissue, gastrointestinal mucosa, and epithelia.

Pemphigus is a rare group of blistering autoimmune diseases that affect the skin and mucous membranes. The name is derived from the Greek root pemphix, meaning "blister".

Rituximab, sold under the brand name Rituxan among others, is a monoclonal antibody medication used to treat certain autoimmune diseases and types of cancer. It is used for non-Hodgkin lymphoma, chronic lymphocytic leukemia, rheumatoid arthritis, granulomatosis with polyangiitis, idiopathic thrombocytopenic purpura, pemphigus vulgaris, myasthenia gravis and Epstein–Barr virus-positive mucocutaneous ulcers. It is given by slow intravenous infusion. Biosimilars of Rituxan include Blitzima, Riabni, Ritemvia, Rituenza, Rixathon, Ruxience, and Truxima.

Staphylococcal scalded skin syndrome (SSSS) is a dermatological condition caused by Staphylococcus aureus.

Bullous pemphigoid is an autoimmune pruritic skin disease that typically occurs in people aged over 60, that may involve the formation of blisters (bullae) in the space between the epidermal and dermal skin layers. It is classified as a type II hypersensitivity reaction, which involves formation of anti-hemidesmosome antibodies, causing a loss of keratinocytes to basement membrane adhesion.
Nikolsky's sign is a clinical dermatological sign, named after Pyotr Nikolsky (1858–1940), a Russian physician who trained and worked in the Russian Empire. The sign is present when slight rubbing of the skin results in exfoliation of the outermost layer. A typical test would be to place the eraser of a pencil on the roof of a lesion and spin the pencil in a rolling motion between the thumb and forefinger. If the lesion is opened, then the Nikolsky's sign is present/positive.

Hailey–Hailey disease (HHD), or familial benign chronic pemphigus or familial benign pemphigus, was originally described by the Hailey brothers in 1939. It is a genetic disorder that causes blisters to form on the skin.
The desmogleins are a family of desmosomal cadherins consisting of proteins DSG1, DSG2, DSG3, and DSG4. They play a role in the formation of desmosomes that join cells to one another.
Desmoglein-1 is a protein that in humans is encoded by the DSG1 gene. Desmoglein-1 is expressed everywhere in the skin epidermis, but mainly it is expressed in the superficial upper layers of the skin epidermis.

Desmoglein-3 is a protein that in humans is encoded by the DSG3 gene. In the skin epidermis Desmoglein-3 is expressed in the basal lower layers of the epidermis, and dominates in terms of expression on mucosal surfaces compared to Desmoglein-1.

Pemphigoid is a group of rare autoimmune blistering diseases of the skin, and mucous membranes. As its name indicates, pemphigoid is similar in general appearance to pemphigus, but, unlike pemphigus, pemphigoid does not feature acantholysis, a loss of connections between skin cells.

Dermatitis herpetiformis (DH) is a chronic autoimmune blistering skin condition, characterised by intensely itchy blisters filled with a watery fluid. DH is a cutaneous manifestation of coeliac disease, although the exact causal mechanism is not known. DH is neither related to nor caused by herpes virus; the name means that it is a skin inflammation having an appearance similar to herpes.
Pemphigus foliaceus is an autoimmune blistering disease of the skin. Pemphigus foliaceus causes a characteristic inflammatory attack at the subcorneal layer of epidermis, which results in skin lesions that are scaly or crusted erosions with an erythematous (red) base. Mucosal involvement is absent even with widespread disease.
Pemphigus erythematosus is simply a localized form of pemphigus foliaceus with features of lupus erythematosus.
Paraneoplastic pemphigus (PNP) is an autoimmune disorder stemming from an underlying tumor. It is hypothesized that antigens associated with the tumor trigger an immune response resulting in blistering of the skin and mucous membranes.
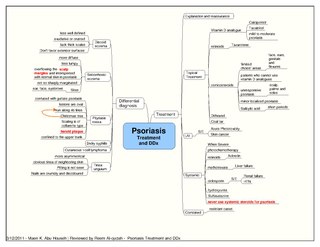
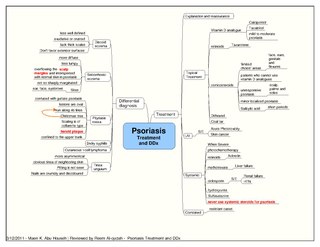
Psoriatic erythroderma represents a form of psoriasis that affects all body sites, including the face, hands, feet, nails, trunk, and extremities. This specific form of psoriasis affects 3 percent of persons diagnosed with psoriasis. First-line treatments for psoriatic erythroderma include immunosuppressive medications such as methotrexate, acitretin, or ciclosporin.

Bullous impetigo is a bacterial skin infection caused by Staphylococcus aureus that results in the formation of large blisters called bullae, usually in areas with skin folds like the armpit, groin, between the fingers or toes, beneath the breast, and between the buttocks. It accounts for 30% of cases of impetigo, the other 70% being non-bullous impetigo.
Mucous membrane pemphigoid is a rare chronic autoimmune subepithelial blistering disease characterized by erosive lesions of the mucous membranes and skin. It is one of the pemphigoid diseases that can result in scarring.
Primary cutaneous diffuse large B-cell lymphoma, leg type (PCDLBCL-LT) is a cutaneous lymphoma skin disease that occurs mostly in elderly females. In this disease, B cells become malignant, accumulate in the dermis and subcutaneous tissue below the dermis to form red and violaceous skin nodules and tumors. These lesions typically occur on the lower extremities but in uncommon cases may develop on the skin at virtually any other site. In ~10% of cases, the disease presents with one or more skin lesions none of which are on the lower extremities; the disease in these cases is sometimes regarded as a variant of PCDLBL, LT termed primary cutaneous diffuse large B-cell lymphoma, other (PCDLBC-O). PCDLBCL, LT is a subtype of the diffuse large B-cell lymphomas (DLBCL) and has been thought of as a cutaneous counterpart to them. Like most variants and subtypes of the DLBCL, PCDLBCL, LT is an aggressive malignancy. It has a 5-year overall survival rate of 40–55%, although the PCDLBCL-O variant has a better prognosis than cases in which the legs are involved.