Caesarean section, also known as C-section or caesarean delivery, is the surgical procedure by which one or more babies are delivered through an incision in the mother's abdomen. It is often performed because vaginal delivery would put the mother or child at risk. Reasons for the operation include obstructed labor, twin pregnancy, high blood pressure in the mother, breech birth, shoulder presentation, and problems with the placenta or umbilical cord. A caesarean delivery may be performed based upon the shape of the mother's pelvis or history of a previous C-section. A trial of vaginal birth after C-section may be possible. The World Health Organization recommends that caesarean section be performed only when medically necessary.

Ectopic pregnancy is a complication of pregnancy in which the embryo attaches outside the uterus. Signs and symptoms classically include abdominal pain and vaginal bleeding, but fewer than 50 percent of affected women have both of these symptoms. The pain may be described as sharp, dull, or crampy. Pain may also spread to the shoulder if bleeding into the abdomen has occurred. Severe bleeding may result in a fast heart rate, fainting, or shock. With very rare exceptions, the fetus is unable to survive.
A multiple birth is the culmination of one multiple pregnancy, where in the mother gives birth to two or more babies. A term most applicable to vertebrate species, multiple births occur in most kinds of mammals, with varying frequencies. Such births are often named according to the number of offspring, as in twins and triplets. In non-humans, the whole group may also be referred to as a litter, and multiple births may be more common than single births. Multiple births in humans are the exception and can be exceptionally rare in the largest mammals.

Amniocentesis is a medical procedure used primarily in the prenatal diagnosis of genetic conditions. It has other uses such as in the assessment of infection and fetal lung maturity. Prenatal diagnostic testing, which includes amniocentesis, is necessary to conclusively diagnose the majority of genetic disorders, with amniocentesis being the gold-standard procedure after 15 weeks' gestation.

In human reproduction, a live birth occurs when a fetus exits the mother showing any definite sign of life such as voluntary movement, heartbeat, or pulsation of the umbilical cord, for however brief a time and regardless of whether the umbilical cord or placenta are intact. After the fetus is expelled from the maternal body it is called a neonate. Whether the birth is vaginal or by caesarean section, and whether the neonate is ultimately viable, is irrelevant.
Fetal distress, also known as non-reassuring fetal status, is a condition during pregnancy or labor in which the fetus shows signs of inadequate oxygenation. Due to its imprecision, the term "fetal distress" has fallen out of use in American obstetrics. The term "non-reassuring fetal status" has largely replaced it. It is characterized by changes in fetal movement, growth, heart rate, and presence of meconium stained fluid.
A hysterotomy is an incision made in the uterus. This surgical incision is used in several medical procedures, including during termination of pregnancy in the second trimester and delivering the fetus during caesarean section. It is also used to gain access and perform surgery on a fetus during pregnancy to correct birth defects, and it is an option to achieve resuscitation if cardiac arrest occurs during pregnancy and it is necessary to remove the fetus from the uterus.

Placental abruption is when the placenta separates early from the uterus, in other words separates before childbirth. It occurs most commonly around 25 weeks of pregnancy. Symptoms may include vaginal bleeding, lower abdominal pain, and dangerously low blood pressure. Complications for the mother can include disseminated intravascular coagulopathy and kidney failure. Complications for the baby can include fetal distress, low birthweight, preterm delivery, and stillbirth.
Fetal viability is the ability of a human fetus to survive outside the uterus. Viability depends upon factors such as birth weight, gestational age, and the availability of advanced medical care. In low-income countries, more than 90% of extremely preterm newborns die due to a lack of said medical care; in high-income countries, the vast majority of these newborns survive.

Prelabor rupture of membranes (PROM), previously known as premature rupture of membranes, is breakage of the amniotic sac before the onset of labor. Women usually experience a painless gush or a steady leakage of fluid from the vagina. Complications in the baby may include premature birth, cord compression, and infection. Complications in the mother may include placental abruption and postpartum endometritis.
A self-performed caesarean section is a form of self-surgery where a woman attempts to perform a caesarean section on herself. Cases of self-inflicted caesarean section have been reported since the 18th and 19th century. While mostly deadly to either the woman, the child, or both, there are at least five known documented successful cases.

ABC and its variations are initialism mnemonics for essential steps used by both medical professionals and lay persons when dealing with a patient. In its original form it stands for Airway, Breathing, and Circulation. The protocol was originally developed as a memory aid for rescuers performing cardiopulmonary resuscitation, and the most widely known use of the initialism is in the care of the unconscious or unresponsive patient, although it is also used as a reminder of the priorities for assessment and treatment of patients in many acute medical and trauma situations, from first-aid to hospital medical treatment. Airway, breathing, and circulation are all vital for life, and each is required, in that order, for the next to be effective: a viable Airway is necessary for Breathing to provide oxygenated blood for Circulation. Since its development, the mnemonic has been extended and modified to fit the different areas in which it is used, with different versions changing the meaning of letters or adding other letters.

Fetal surgery also known as antenatal surgery, prenatal surgery, is a growing branch of maternal-fetal medicine that covers any of a broad range of surgical techniques that are used to treat congenital abnormalities in fetuses who are still in the pregnant uterus. There are three main types: open fetal surgery, which involves completely opening the uterus to operate on the fetus; minimally invasive fetoscopic surgery, which uses small incisions and is guided by fetoscopy and sonography; and percutaneous fetal therapy, which involves placing a catheter under continuous ultrasound guidance.

Uterine atony is the failure of the uterus to contract adequately following delivery. Contraction of the uterine muscles during labor compresses the blood vessels and slows flow, which helps prevent hemorrhage and facilitates coagulation. Therefore, a lack of uterine muscle contraction can lead to an acute hemorrhage, as the vasculature is not being sufficiently compressed. Uterine atony is the most common cause of postpartum hemorrhage, which is an emergency and potential cause of fatality. Across the globe, postpartum hemorrhage is among the top five causes of maternal death. Recognition of the warning signs of uterine atony in the setting of extensive postpartum bleeding should initiate interventions aimed at regaining stable uterine contraction.
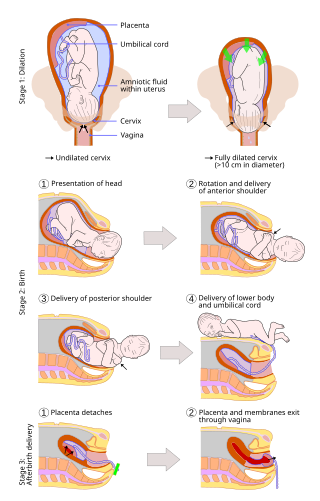
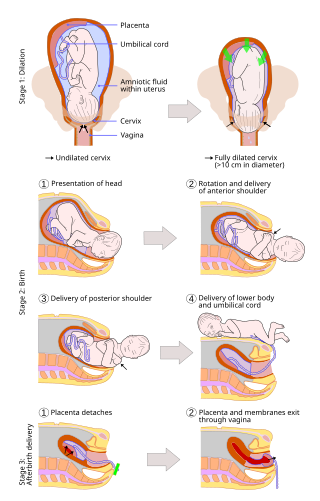
A vaginal delivery is the birth of offspring in mammals through the vagina. It is the most common method of childbirth worldwide. It is considered the preferred method of delivery, with lower morbidity and mortality than caesarean sections (C-sections).

A shoulder presentation is a malpresentation at childbirth where the baby is in a transverse lie, thus the leading part is an arm, a shoulder, or the trunk. While a baby can be delivered vaginally when either the head or the feet/buttocks are the leading part, it usually cannot be expected to be delivered successfully with a shoulder presentation unless a cesarean section (C/S) is performed.

Circumvallate placenta is a rare condition affecting about 1-2% of pregnancies, in which the amnion and chorion fetal membranes essentially "double back" on the fetal side around the edges of the placenta. After delivery, a circumvallate placenta has a thick ring of membranes on its fetal surface. Circumvallate placenta is a placental morphological abnormality associated with increased fetal morbidity and mortality due to the restricted availability of nutrients and oxygen to the developing fetus.

A lower (uterine) segment Caesarean section (LSCS) is the most commonly used type of Caesarean section. Most commonly to deliver the baby a transverse incision is made in the lower uterine segment above the attachment of the urinary bladder to the uterus. This type of incision results in less blood loss and is easier to repair than other types of Caesarean sections.
Definitions of abortion vary from one source to another. Abortion has many definitions that can differ from each other in significant ways. Given the contentious nature of abortion, lawmakers and other stakeholders often face controversy in defining abortion. Language referring to abortion often reflects societal and political opinions . Influential non-state actors like the United Nations and the Roman Catholic Church have also engendered controversy over efforts to define abortion.

Emergency childbirth is the precipitous birth of an infant in an unexpected setting. In planned childbirth, mothers choose the location and obstetric team ahead of time. Options range from delivering at home, at a hospital, a medical facility or a birthing center. Sometimes, birth can occur on the way to these facilities, without a healthcare team. The rates of unplanned childbirth are low. If the birth is imminent, emergency measures may be needed. Emergency services can be contacted for help in some countries.