Edward Jenner was an English physician and scientist who pioneered the concept of vaccines and created the smallpox vaccine, the world's first vaccine. The terms vaccine and vaccination are derived from Variolae vaccinae, the term devised by Jenner to denote cowpox. He used it in 1798 in the title of his Inquiry into the Variolae vaccinae known as the Cow Pox, in which he described the protective effect of cowpox against smallpox.

Vaccination is the administration of a vaccine to help the immune system develop immunity from a disease. Vaccines contain a microorganism or virus in a weakened, live or killed state, or proteins or toxins from the organism. In stimulating the body's adaptive immunity, they help prevent sickness from an infectious disease. When a sufficiently large percentage of a population has been vaccinated, herd immunity results. Herd immunity protects those who may be immunocompromised and cannot get a vaccine because even a weakened version would harm them. The effectiveness of vaccination has been widely studied and verified. Vaccination is the most effective method of preventing infectious diseases; widespread immunity due to vaccination is largely responsible for the worldwide eradication of smallpox and the elimination of diseases such as polio and tetanus from much of the world. However, some diseases, such as measles outbreaks in America, have seen rising cases due to relatively low vaccination rates in the 2010s – attributed, in part, to vaccine hesitancy. According to the World Health Organization, vaccination prevents 3.5–5 million deaths per year.

Cowpox is an infectious disease caused by the cowpox virus (CPXV). It presents with large blisters in the skin, a fever and swollen glands, historically typically following contact with an infected cow, though in the last several decades more often from infected cats. The hands and face are most frequently affected and the spots are generally very painful.

The smallpox vaccine is the first vaccine to have been developed against a contagious disease. In 1796, British physician Edward Jenner demonstrated that an infection with the relatively mild cowpox virus conferred immunity against the deadly smallpox virus. Cowpox served as a natural vaccine until the modern smallpox vaccine emerged in the 20th century. From 1958 to 1977, the World Health Organization (WHO) conducted a global vaccination campaign that eradicated smallpox, making it the only human disease to be eradicated. Although routine smallpox vaccination is no longer performed on the general public, the vaccine is still being produced to guard against bioterrorism, biological warfare, and mpox.

José Fernando de Abascal y Sousa, 1st Marquess of Concordia, KOS, was a Spanish military officer and colonial administrator in America. From August 20, 1806, to July 7, 1816, he was viceroy of Peru, during the Spanish American wars of independence.

Oswaldo Gonçalves Cruz, was a Brazilian physician, pioneer bacteriologist, epidemiologist and public health officer and the founder of the Oswaldo Cruz Institute.
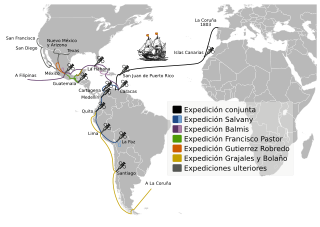
The Royal Philanthropic Vaccine Expedition, commonly referred to as the Balmis Expedition, was a Spanish healthcare mission that lasted from 1803 to 1806, led by Dr Francisco Javier de Balmis, which vaccinated millions of inhabitants of Spanish America and Asia against smallpox. The vaccine was actually transported through children: orphaned boys who sailed with the expedition.

James Phipps was the first person given the experimental cowpox vaccine by Edward Jenner. Jenner knew of a local belief that dairy workers who had contracted a relatively mild infection called cowpox were immune to smallpox, and successfully tested his theory on the 8-years-old James Phipps on 17 May 1796.

Francisco Javier de Balmis was a Spanish physician best known for leading an 1803 expedition to Spanish America and the Philippines to vaccinate populations against smallpox. His expedition is considered the first international vaccination campaign in history and one of the most important events in the history of medicine. It inspired recent vaccination efforts such as that of Carlos Canseco, president of Rotary International, to start the worldwide program PolioPlus to eradicate polio.

Smallpox was an infectious disease caused by variola virus, which belongs to the genus Orthopoxvirus. The last naturally occurring case was diagnosed in October 1977, and the World Health Organization (WHO) certified the global eradication of the disease in 1980, making smallpox the only human disease to have been eradicated to date.
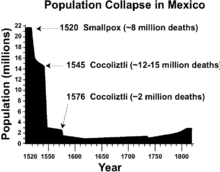
The history of smallpox extends into pre-history. Genetic evidence suggests that the smallpox virus emerged 3,000 to 4,000 years ago. Prior to that, similar ancestral viruses circulated, but possibly only in other mammals, and possibly with different symptoms. Only a few written reports dating from about 500 AD to 1000 AD are considered reliable historical descriptions of smallpox, so understanding of the disease prior to that has relied on genetics and archaeology. However, during the 2nd millennium AD, especially starting in the 16th century, reliable written reports become more common. The earliest physical evidence of smallpox is found in the Egyptian mummies of people who died some 3,000 years ago. Smallpox has had a major impact on world history, not least because indigenous populations of regions where smallpox was non-native, such as the Americas and Australia, were rapidly and greatly reduced by smallpox during periods of initial foreign contact, which helped pave the way for conquest and colonization. During the 18th century the disease killed an estimated 400,000 Europeans each year, including five reigning monarchs, and was responsible for a third of all blindness. Between 20 and 60% of all those infected—and over 80% of infected children—died from the disease.
In 1767, the 11-year-old composer Wolfgang Amadeus Mozart was struck by smallpox. Like all smallpox victims, he was at serious risk of dying, but he survived the disease. This article discusses smallpox as it existed in Mozart's time, the decision taken in 1764 by Mozart's father Leopold not to inoculate his children against the disease, the course of Mozart's illness, and the aftermath.
Variolation was the method of inoculation first used to immunize individuals against smallpox (Variola) with material taken from a patient or a recently variolated individual, in the hope that a mild, but protective, infection would result. Only 1–2% of those variolated died from the intentional infection compared to 30% who contracted smallpox naturally. Variolation is no longer used today. It was replaced by the smallpox vaccine, a safer alternative. This in turn led to the development of the many vaccines now available against other diseases.
Dr. Santiago María del Granado y Navarro Calderón, 1st Count of Cotoca, was a Spanish nobleman and physician, who at the beginning of the 19th century traveled through some of the most remote regions of South America where epidemics were raging, to inoculate Native Americans with the recently discovered vaccine and prevent the spread of smallpox.
Inoculation is the act of implanting a pathogen or other microbe or virus into a person or other organism. It is a method of artificially inducing immunity against various infectious diseases. The term "inoculation" is also used more generally to refer to intentionally depositing microbes into any growth medium, as into a Petri dish used to culture the microbe, or into food ingredients for making cultured foods such as yoghurt and fermented beverages such as beer and wine. This article is primarily about the use of inoculation for producing immunity against infection. Inoculation has been used to eradicate smallpox and to markedly reduce other infectious diseases such as polio. Although the terms "inoculation", "vaccination", and "immunization" are often used interchangeably, there are important differences. Inoculation is the act of implanting a pathogen or microbe into a person or other recipient; vaccination is the act of implanting or giving someone a vaccine specifically; and immunization is the development of disease resistance that results from the immune system's response to a vaccine or natural infection.

Rafael María de Aguilar y Ponce de León was a Spanish military officer who served as the 56th Governor-General of the Philippines and was the longest serving governor in the Spanish Philippines.
Isabel Zendal Gómez was a Spanish nurse from Galicia who took part in the Balmis Expedition, which took smallpox vaccination to South America and Asia.
An epidemic of smallpox in 1856 on the west Pacific island of Guam, then under the control of Spain, resulted in the death of over half of the population, or about 4,500 people. The population collapse led Spanish authorities to transfer the population of Pago to Hagåtña, ending a settlement dating back before colonization. It also led the Governor of the Spanish Mariana Islands to encourage immigration to Guam.

An outbreak of smallpox occurred in the city of Wrocław in Poland in the summer of 1963. The disease was brought to Poland by an officer in the Ministry of Public Security who had returned from India. The epidemic lasted for two months, causing 99 people to fall ill and seven to die. It caused Wrocław to close and quarantine itself.

The Capture of Alhóndiga de Granaditas was a military action carried out in Guanajuato, viceroyalty of New Spain, on September 28, 1810, between the royalist soldiers of the province and the insurgents commanded by Miguel Hidalgo and Ignacio Allende. The fear unleashed in the social circles of the provincial capital made the intendant, Juan Antonio Riaño, ask the population to barrack in the Alhóndiga de Granaditas, a granary built in 1800, and in whose construction Miguel Hidalgo had participated as an advisor to his old friend Riaño. After several hours of combat, Riaño was killed and the Spaniards who had taken refuge there wished to surrender. The military in the viceroy's service continued the fight, until the insurgents managed to enter and then massacred not only the few guards that defended it, but also the numerous families of civilians who had taken refuge there. Many historians consider this confrontation more like a mutiny or massacre of civilians than a battle, since there were no conditions of military equality between the two sides.