Yellow fever is a viral disease of typically short duration. In most cases, symptoms include fever, chills, loss of appetite, nausea, muscle pains – particularly in the back – and headaches. Symptoms typically improve within five days. In about 15% of people, within a day of improving the fever comes back, abdominal pain occurs, and liver damage begins causing yellow skin. If this occurs, the risk of bleeding and kidney problems is increased.

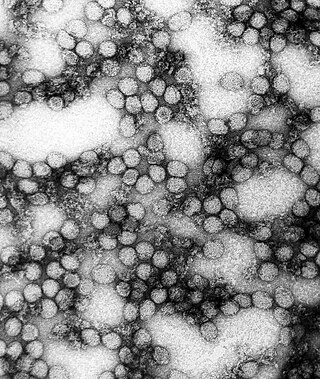
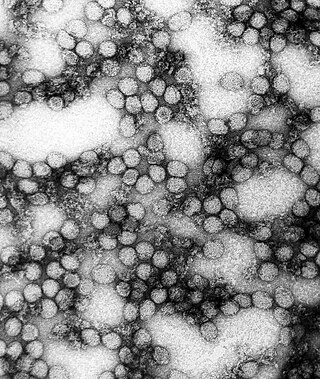
Dengue fever is a mosquito-borne tropical disease caused by the dengue virus. Symptoms typically begin three to fourteen days after infection. These may include a high fever, headache, vomiting, muscle and joint pains, and a characteristic skin itching and skin rash. Recovery generally takes two to seven days. In a small proportion of cases, the disease develops into a more severe dengue hemorrhagic fever, resulting in bleeding, low levels of blood platelets and blood plasma leakage, or into dengue shock syndrome, where dangerously low blood pressure occurs.

Aedes albopictus, from the mosquito (Culicidae) family, also known as the (Asian) tiger mosquito or forest mosquito, is a mosquito native to the tropical and subtropical areas of Southeast Asia. In the past few centuries, however, this species has spread to many countries through the transport of goods and international travel. It is characterized by the white bands on its legs and body.

Arbovirus is an informal name for any virus that is transmitted by arthropod vectors. The term arbovirus is a portmanteau word. Tibovirus is sometimes used to more specifically describe viruses transmitted by ticks, a superorder within the arthropods. Arboviruses can affect both animals and plants. In humans, symptoms of arbovirus infection generally occur 3–15 days after exposure to the virus and last three or four days. The most common clinical features of infection are fever, headache, and malaise, but encephalitis and viral hemorrhagic fever may also occur.

Singapore Green Plan 2012 was released in 2002 by the Ministry of the Environment and Water Resources (MEWR) as a continuation of the Singapore Green Plan first issued in 1992. Comprising eight distinct key measures, SGP 2012 aims to create an environmentally-conscious Singapore, promoting conservation of the nation's natural resources and the use of green technology to conserve the environment, both locally and globally. It also aims to ensure sustainability in the country's development and to instill within Singaporeans personal duty and commitment towards the environment.

National Environment Agency (NEA) is a statutory board under the Ministry of Sustainability and the Environment of the Government of Singapore.

Chikungunya is a mosquito-borne alpha virus that was first isolated after a 1952 outbreak in modern-day Tanzania. The virus has circulated in forested regions of sub-Saharan African in cycles involving nonhuman primate hosts and arboreal mosquito vectors. Phylogenetic studies indicate that the urban transmission cycle—the transmission of a pathogen between humans and mosquitoes that exist in urban environments—was established on multiple occasions from strains occurring on the eastern half of Africa in non-human primate hosts. This emergence and spread beyond Africa may have started as early as the 18th century. Currently, available data does not indicate whether the introduction of chikungunya into Asia occurred in the 19th century or more recently, but this epidemic Asian strain causes outbreaks in India and continues to circulate in Southeast Asia.
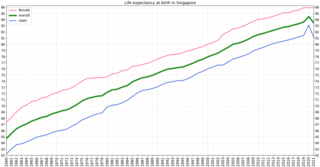
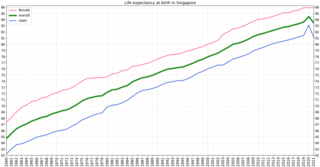
Singapore is one of the wealthiest countries in the world, with a gross domestic product (GDP) per capita of more than $57,000. Life expectancy at birth is 82.3 and infant mortality is 2.7 per 1000 live births. The population is ageing and by 2030, 20% will be over 65. However it is estimated that about 85% of those over 65 are healthy and reasonably active. Singapore has a universal health care system.

Zika virus is a member of the virus family Flaviviridae. It is spread by daytime-active Aedes mosquitoes, such as A. aegypti and A. albopictus. Its name comes from the Ziika Forest of Uganda, where the virus was first isolated in 1947. Zika virus shares a genus with the dengue, yellow fever, Japanese encephalitis, and West Nile viruses. Since the 1950s, it has been known to occur within a narrow equatorial belt from Africa to Asia. From 2007 to 2016, the virus spread eastward, across the Pacific Ocean to the Americas, leading to the 2015–2016 Zika virus epidemic.

As of 2010, dengue fever is believed to infect 50 to 100 million people worldwide a year with 1/2 million life-threatening infections. It dramatically increased in frequency between 1960 and 2010, by 30 fold. This increase is believed to be due to a combination of urbanization, population growth, increased international travel, and global warming. The geographical distribution is around the equator with 70% of the total 2.5 billion people living in endemic areas from Asia and the Pacific. Many of the infected people during outbreaks are not virally tested, therefore their infections may also be due to chikungunya, a coinfection of both, or even other similar viruses.
Dengue fever is an important infectious disease in Pakistan with increasingly frequent epidemics. Despite the efforts of the Government of Pakistan, especially in Punjab, the high cost of prevention has limited the ability of Pakistan to control epidemics. In Pakistan, in the summer of 2011, more than 300 people died of Dengue fever. The prevalence of the disease was over 14,000. The outbreaks occurred mostly in the Lahore area, Punjab, Pakistan.
In the 2013 dengue outbreak in Singapore, a significant rise in the number of dengue fever cases was reported in Singapore. The outbreak began in January, with the number of infections beginning to surge in April, before eventually reaching a peak of 842 dengue cases in the week of 16–22 June 2013. This figure was far beyond the highest number of cases per week in the previous three years. Although there were concerns that the rate of infection could exceed 1,000 per week, these fears did not materialize.

A lethal ovitrap is a device which attracts gravid female container-breeding mosquitoes and kills them. The traps halt the insect's life cycle by killing adult insects and stopping reproduction. The original use of ovitraps was to monitor the spread and density of Aedes and other container-breeding mosquito populations by collecting eggs which could be counted, or hatched to identify the types of insects. Since its conception, researchers found that adding lethal substances to the ovitraps could control the populations of these targeted species. These traps are called lethal ovitraps. They primarily target Aedes aegypti and Aedes albopictus mosquitoes, which are the main vectors of dengue fever, Zika virus, west Nile virus, yellow fever, and chikungunya.
The 2013–2014 chikungunya outbreak represented the first recorded outbreak of the disease outside of tropical Africa and Asia. In December 2013, the first locally transmitted case of chikungunya in the Americas was detected in Saint Martin. Shortly after the first case the disease began to spread rapidly throughout the Caribbean region. By the end of the year, it had spread to Martinique and Guadeloupe, with suspected cases in Saint Barthélemy. By the end of January 2014, cases had been confirmed in Saint Barthélemy, as well as the British Virgin Islands, Dominica, and French Guiana. On the basis of 4,000 confirmed cases and over 30,000 suspected cases, the Caribbean Public Health Agency (CARPHA) declared a Caribbean-wide epidemic of the virus in early May. By the end of May, four cases of chikungunya had been confirmed in Florida. By July 2014 there were an estimated 355,000 cases in the Caribbean. By August 2014, 25 Caribbean countries had confirmed at least one case. The epidemic was over by 2015.

An epidemic of Zika fever, caused by Zika virus, began in Brazil and affected other countries in the Americas from April 2015 to November 2016. The World Health Organization (WHO) declared the end of the epidemic in November 2016, but noted that the virus still represents "a highly significant and long term problem". It is estimated that 1.5 million people were infected by Zika virus in Brazil, with over 3,500 cases of infant microcephaly reported between October 2015 and January 2016. The epidemic also affected other parts of South and North America, as well as several islands in the Pacific.
In October 2013, there was an outbreak of Zika fever in French Polynesia, the first outbreak of several Zika outbreaks across Oceania. With 8,723 cases reported, it was the largest outbreak of Zika fever before the outbreak in the Americas that began in April 2015. An earlier outbreak occurred on Yap Island in the Federated States of Micronesia in 2007, but it is thought that the 2013–2014 outbreak involved an independent introduction of the Zika virus from Southeast Asia. Investigators suggested that the outbreaks of mosquito-borne diseases in the Pacific from 2012 to 2014 were "the early stages of a wave that will continue for several years", particularly because of their vulnerability to infectious diseases stemming from isolation and immunologically naive populations.

This article primarily covers the chronology of the 2015–16 Zika virus epidemic. Flag icons denote the first announcements of confirmed cases by the respective nation-states, their first deaths, and relevant sessions and announcements of the World Health Organization (WHO), and the U.S. Centers for Disease Control (CDC), as well as relevant virological, epidemiological, and entomological studies.

The 2019–2020 dengue fever epidemic was an epidemic of the infectious disease dengue fever in several countries of Southeast Asia, including the Philippines, Malaysia, Vietnam, and Bangladesh, Pakistan, India, Thailand, Singapore, and Laos. The spread of the disease was exacerbated by falling vaccination levels in certain areas, and by a growing population of mosquitoes, which are the primary carriers of the disease, and which are able to reproduce in larger numbers where humans have littered the environment with plastic containers, which provide an ideal breeding ground for mosquitoes. Affected countries have sought to control the epidemic through increased vaccination efforts, and through efforts to control the mosquito population.

Global climate change has resulted in a wide range of impacts on the spread of infectious diseases. Like other ways in which climate change affects on human health, climate change exacerbates existing inequalities and challenges in managing infectious disease. Infectious diseases whose transmission can be impacted by climate change include dengue fever, malaria, tick-borne diseases, leishmaniasis and Ebola virus disease. For example, climate change is altering the geographic range and seasonality of the mosquito that can carry dengue.
In the 2020 dengue outbreak in Singapore, a record-breaking number of dengue fever cases was reported in Singapore. This was part of the wider 2019–2020 dengue fever epidemic which also affected several neighbouring countries in Southeast Asia.