Related Research Articles

The adrenal glands are endocrine glands that produce a variety of hormones including adrenaline and the steroids aldosterone and cortisol. They are found above the kidneys. Each gland has an outer cortex which produces steroid hormones and an inner medulla. The adrenal cortex itself is divided into three main zones: the zona glomerulosa, the zona fasciculata and the zona reticularis.

Stress, whether physiological, biological or psychological, is an organism's response to a stressor such as an environmental condition. When stressed by stimuli that alter an organism's environment, multiple systems respond across the body. In humans and most mammals, the autonomic nervous system and hypothalamic-pituitary-adrenal (HPA) axis are the two major systems that respond to stress. Two well-known hormones that humans produce during stressful situations are adrenaline and cortisol.

Corticotropin-releasing hormone (CRH) is a peptide hormone involved in stress responses. It is a releasing hormone that belongs to corticotropin-releasing factor family. In humans, it is encoded by the CRH gene. Its main function is the stimulation of the pituitary synthesis of adrenocorticotropic hormone (ACTH), as part of the hypothalamic–pituitary–adrenal axis.

The hypothalamic–pituitary–adrenal axis is a complex set of direct influences and feedback interactions among three components: the hypothalamus, the pituitary gland, and the adrenal glands. These organs and their interactions constitute the HPA axis.
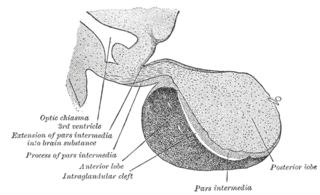
A major organ of the endocrine system, the anterior pituitary is the glandular, anterior lobe that together with the posterior lobe makes up the pituitary gland (hypophysis) which, in humans, is located at the base of the brain, protruding off the bottom of the hypothalamus.

Cortisol is a steroid hormone, in the glucocorticoid class of hormones and a stress hormone. When used as a medication, it is known as hydrocortisone.

Adrenal insufficiency is a condition in which the adrenal glands do not produce adequate amounts of steroid hormones. The adrenal glands—also referred to as the adrenal cortex—normally secrete glucocorticoids, mineralocorticoids, and androgens. These hormones are important in regulating blood pressure, electrolytes, and metabolism as a whole. Deficiency of these hormones leads to symptoms ranging from abdominal pain, vomiting, muscle weakness and fatigue, low blood pressure, depression, mood and personality changes to organ failure and shock. Adrenal crisis may occur if a person having adrenal insufficiency experiences stresses, such as an accident, injury, surgery, or severe infection; this is a life-threatening medical condition resulting from severe deficiency of cortisol in the body. Death may quickly follow.
Corticotropes are basophilic cells in the anterior pituitary that produce pro-opiomelanocortin (POMC) which undergoes cleavage to adrenocorticotropin (ACTH), β-lipotropin (β-LPH), and melanocyte-stimulating hormone (MSH). These cells are stimulated by corticotropin releasing hormone (CRH) and make up 15–20% of the cells in the anterior pituitary. The release of ACTH from the corticotropic cells is controlled by CRH, which is formed in the cell bodies of parvocellular neurosecretory cells within the paraventricular nucleus of the hypothalamus and passes to the corticotropes in the anterior pituitary via the hypophyseal portal system. Adrenocorticotropin hormone stimulates the adrenal cortex to release glucocorticoids and plays an important role in the stress response.
Psychoneuroimmunology (PNI), also referred to as psychoendoneuroimmunology (PENI) or psychoneuroendocrinoimmunology (PNEI), is the study of the interaction between psychological processes and the nervous and immune systems of the human body. It is a subfield of psychosomatic medicine. PNI takes an interdisciplinary approach, incorporating psychology, neuroscience, immunology, physiology, genetics, pharmacology, molecular biology, psychiatry, behavioral medicine, infectious diseases, endocrinology, and rheumatology.
An insulin tolerance test (ITT) is a medical diagnostic procedure during which insulin is injected into a patient's vein, after which blood glucose is measured at regular intervals. This procedure is performed to assess pituitary function, adrenal function, insulin sensitivity, and sometimes for other purposes. An ITT is usually ordered and interpreted by an endocrinologist.
A Corticotropin-releasing hormone antagonist is a specific type of receptor antagonist that blocks the receptor sites for corticotropin-releasing hormone, also known as corticotropin-releasing factor (CRF), which synchronizes the behavioral, endocrine, autonomic, and immune responses to stress by controlling the hypothalamic-pituitary-adrenal axis. CRH antagonists thereby block the consequent secretions of ACTH and cortisol due to stress, among other effects.
Critical illness–related corticosteroid insufficiency is a form of adrenal insufficiency in critically ill patients who have blood corticosteroid levels which are inadequate for the severe stress response they experience. Combined with decreased glucocorticoid receptor sensitivity and tissue response to corticosteroids, this adrenal insufficiency constitutes a negative prognostic factor for intensive care patients.

The cortisol awakening response (CAR) is an increase between 38% and 75% in cortisol levels peaking 30–45 minutes after awakening in the morning in some people. This rise is superimposed upon the late-night rise in cortisol which occurs before awakening. While its purpose is uncertain, it may be linked to the hippocampus' preparation of the hypothalamic-pituitary-adrenal axis (HPA) in order to face anticipated stress.
Early childhood is a critical period in a child's life that includes ages from conception to five years old. Psychological stress is an inevitable part of life. Human beings can experience stress from an early age. Although stress is a factor for the average human being, it can be a positive or negative molding aspect in a young child's life.
Glucocorticoid deficiency is a condition where the body doesn’t produce enough glucocorticoid hormones.
Maternal fetal stress transfer is a physiological phenomenon in which psychosocial stress experienced by a mother during her pregnancy can be transferred to the fetus. Psychosocial stress describes the brain's physiological response to perceived social threat. Because of a link in blood supply between a mother and fetus, it has been found that stress can leave lasting effects on a developing fetus, even before a child is born. According to recent studies, these effects are mainly the result of two particular stress biomarkers circulating in the maternal blood supply: cortisol and catecholamines.
Epigenetics of anxiety and stress–related disorders is the field studying the relationship between epigenetic modifications of genes and anxiety and stress-related disorders, including mental health disorders such as generalized anxiety disorder (GAD), post-traumatic stress disorder, obsessive-compulsive disorder (OCD), and more. These changes can lead to transgenerational stress inheritance.
Fetal programming, also known as prenatal programming, is the theory that environmental cues experienced during fetal development play a seminal role in determining health trajectories across the lifespan.
Opioid-induced endocrinopathy (OIE) is a complication of chronic opioid treatment. It is a common name for all hypothalamo-pituitary axis disorders, which can be observed mostly after long term use of opioids, both as a treatment and as a substance of abuse.
In social psychology, social buffering is a phenomenon where social connections can alleviate negative consequences of stressful events.
References
- 1 2 Dai, Xing; Thavundayil, Joseph; Santella, Sandra; Gianoulakis, Christina (2007). "Response of the HPA-axis to alcohol and stress as a function of alcohol dependence and family history of alcoholism". Psychoneuroendocrinology. 32 (3): 293–305. doi:10.1016/j.psyneuen.2007.01.004. PMID 17349749. S2CID 39315868.
- ↑ Lupien, Sonia J.; McEwen, Bruce S.; Gunnar, Megan R.; Heim, Christine (2009). "Effects of stress throughout the lifespan on the brain, behaviour and cognition". Nature Reviews Neuroscience. 10 (6): 434–45. doi:10.1038/nrn2639. PMID 19401723. S2CID 205504945.
- ↑ Mendelson, Jack; Stein, Stefan (1966). "Serum Cortisol Levels in Alcoholic and Nonalcoholic Subjects During Experimentally Induced Ethanol Intoxication". Psychosomatic Medicine. 28 (4): 616–26. CiteSeerX 10.1.1.503.1374 . doi:10.1097/00006842-196607000-00037. S2CID 147372625 . Retrieved 2014-01-07.
- ↑ Thayer, Julian F.; Hall, Martica; Sollers, John J.; Fischer, Joachim E. (2006). "Alcohol use, urinary cortisol, and heart rate variability in apparently healthy men: Evidence for impaired inhibitory control of the HPA axis in heavy drinkers". International Journal of Psychophysiology. 59 (3): 244–50. doi:10.1016/j.ijpsycho.2005.10.013. PMID 16325293.
- ↑ Stalder, Tobias; Kirschbaum, Clemens; Heinze, Kareen; Steudte, Susann; Foley, Paul; Tietze, Antje; Dettenborn, Lucia (2010). "Use of hair cortisol analysis to detect hypercortisolism during active drinking phases in alcohol-dependent individuals". Biological Psychology. 85 (3): 357–60. doi:10.1016/j.biopsycho.2010.08.005. PMID 20727937. S2CID 14554271.