Related Research Articles

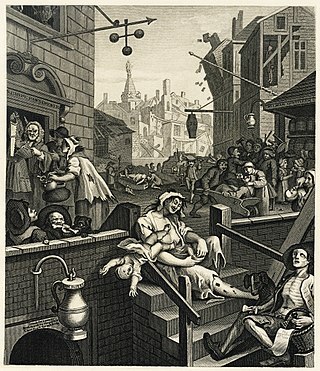
Alcoholism is the continued drinking of alcohol despite it causing problems. Some definitions require evidence of dependence and withdrawal. Problematic use of alcohol has been mentioned in the earliest historical records. The World Health Organization (WHO) estimated there were 283 million people with alcohol use disorders worldwide as of 2016. The term alcoholism was first coined in 1852, but alcoholism and alcoholic are sometimes considered stigmatizing and to discourage seeking treatment, so diagnostic terms such as alcohol use disorder or alcohol dependence are often used instead in a clinical context.

Alcohol abuse encompasses a spectrum of alcohol-related substance abuse, ranging from the consumption of more than 2 drinks per day on average for men, or more than 1 drink per day on average for women, to binge drinking or alcohol use disorder.
The long-term effects of alcohol have been extensively researched. The health effects of long-term alcohol consumption on health vary depending on the amount consumed. Even light drinking poses health risks, but small amounts of alcohol may also have health benefits. Alcoholism causes severe health consequences which outweigh any potential benefits.

Naltrexone, sold under the brand name Revia among others, is a medication primarily used to manage alcohol use or opioid use disorder by reducing cravings and feelings of euphoria associated with substance use disorder. It has also been found effective in the treatment of other addictions and may be used for them off-label. An opioid-dependent person should not receive naltrexone before detoxification. It is taken by mouth or by injection into a muscle. Effects begin within 30 minutes, though a decreased desire for opioids may take a few weeks to occur. Side effects may include trouble sleeping, anxiety, nausea, and headaches. In those still on opioids, opioid withdrawal may occur. Use is not recommended in people with liver failure. It is unclear if use is safe during pregnancy. Naltrexone is an opioid antagonist and works by blocking the effects of opioids, including both opioid drugs as well as opioids naturally produced in the brain.
Alcohol tolerance refers to the bodily responses to the functional effects of ethanol in alcoholic beverages. This includes direct tolerance, speed of recovery from insobriety and resistance to the development of alcohol use disorder.
Alcohol has a number of effects on health. Short-term effects of alcohol consumption include intoxication and dehydration. Long-term effects of alcohol include changes in the metabolism of the liver and brain, several types of cancer and alcohol use disorder. Alcohol intoxication affects the brain, causing slurred speech, clumsiness, and delayed reflexes. There is an increased risk of developing an alcohol use disorder for teenagers while their brain is still developing. Adolescents who drink have a higher probability of injury including death.
The Alcohol Use Disorders Identification Test (AUDIT) is a ten-item questionnaire approved by the World Health Organization to screen patients for hazardous (risky) and harmful alcohol consumption. It was developed from a WHO multi-country collaborative study, the items being selected for the AUDIT being the best performing of approximately 150 items including in the original survey. It is widely used as a summary measure of alcohol use and related problems. It has application in primary health care, medical clinics, and hospital units and performs well in these settings. Using different cut-off points, it can also screen for Alcohol Use Disorder (DSM-5) and Alcohol Dependence. Guidelines for the use of the AUDIT have been published by WHO and are available in several languages. It has become a widely used instrument and has been translated into approximately fifty languages.
The modern disease theory of alcoholism states that problem drinking is sometimes caused by a disease of the brain, characterized by altered brain structure and function. Today, alcohol use disorder (AUD) is used as a more scientific and suitable approach to alcohol dependence and alcohol-related problems.
A drug-related blackout is a phenomenon caused by the intake of any substance or medication in which short-term and long-term memory creation is impaired, therefore causing a complete inability to recall the past. Blackouts are frequently described as having effects similar to that of anterograde amnesia, in which the subject cannot recall any events after the event that caused amnesia.

A hangover is the experience of various unpleasant physiological and psychological effects usually following the consumption of alcohol, such as wine, beer, and liquor. Hangovers can last for several hours or for more than 24 hours. Typical symptoms of a hangover may include headache, drowsiness, concentration problems, dry mouth, dizziness, fatigue, gastrointestinal distress, absence of hunger, light sensitivity, depression, sweating, hyper-excitability, irritability, and anxiety.
Alcohol myopia is a cognitive-physiological theory on alcohol use disorder in which many of alcohol's social and stress-reducing effects, which may underlie its addictive capacity, are explained as a consequence of alcohol's narrowing of perceptual and cognitive functioning. The alcohol myopia model posits that rather than disinhibit, alcohol produces a myopia effect that causes users to pay more attention to salient environmental cues and less attention to less salient cues. Therefore, alcohol's myopic effects cause intoxicated people to respond almost exclusively to their immediate environment. This "nearsightedness" limits their ability to consider future consequences of their actions as well as regulate their reactive impulses.
The impact of alcohol on aging is multifaceted. Evidence shows that alcoholism or alcohol abuse can cause both accelerated (or premature) aging – in which symptoms of aging appear earlier than normal – and exaggerated aging, in which the symptoms appear at the appropriate time but in a more exaggerated form. The effects of alcohol use disorder on the aging process include hypertension, cardiac dysrhythmia, cancers, gastrointestinal disorders, neurocognitive deficits, bone loss, and emotional disturbances especially depression. On the other hand, research also shows that drinking moderate amounts of alcohol may protect healthy adults from developing coronary heart disease. The American Heart Association cautions people not to start drinking, if you are not already drinking.

Alcoholism in family systems refers to the conditions in families that enable alcoholism and the effects of alcoholic behavior by one or more family members on the rest of the family. Mental health professionals are increasingly considering alcoholism and addiction as diseases that flourish in and are enabled by family systems.

Alcohol withdrawal syndrome (AWS) is a set of symptoms that can occur following a reduction in alcohol use after a period of excessive use. Symptoms typically include anxiety, shakiness, sweating, vomiting, fast heart rate, and a mild fever. More severe symptoms may include seizures, and delirium tremens (DTs); which can be fatal in untreated patients. Symptoms start at around 6 hours after last drink. Peak incidence of seizures occurs at 24-36 hours and peak incidence of delirium tremens is at 48-72 hours.

The short-term effects of alcohol consumption range from a decrease in anxiety and motor skills and euphoria at lower doses to intoxication (drunkenness), to stupor, unconsciousness, anterograde amnesia, and central nervous system depression at higher doses. Cell membranes are highly permeable to alcohol, so once it is in the bloodstream, it can diffuse into nearly every cell in the body.

Binge drinking, or heavy episodic drinking, is drinking alcoholic beverages with an intention of becoming intoxicated by heavy consumption of alcohol over a short period of time, but definitions vary considerably.

Alcohol and sex deals with the effects of the consumption of alcohol on sexual behavior. The effects of alcohol are balanced between its suppressive effects on sexual physiology, which will decrease sexual activity, and its suppression of sexual inhibitions.

Effects of alcohol on memory include disruption of various memory processes, affecting both formation and recall of information.
Kindling due to substance withdrawal is the neurological condition which results from repeated withdrawal episodes from sedative–hypnotic drugs such as alcohol and benzodiazepines.

Alcohol, sometimes referred to by the chemical name ethanol, is a depressant drug found in fermented beverages such as beer, wine, and distilled spirit — in particular, rectified spirit. Ethanol is colloquially referred to as "alcohol" because it is the most prevalent alcohol in alcoholic beverages, but technically all alcoholic beverages contain several types of psychoactive alcohols, that are categorized as primary, secondary, or tertiary; Primary, and secondary alcohols, are oxidized to aldehydes, and ketones, respectively, while tertiary alcohols are generally resistant to oxidation; Ethanol is a primary alcohol that has unpleasant actions in the body, many of which are mediated by its toxic metabolite acetaldehyde. Less prevalent alcohols found in alcoholic beverages, are secondary, and tertiary alcohols. For example, the tertiary alcohol 2M2B which is up to 50 times more potent than ethanol and found in trace quantities in alcoholic beverages, has been synthesized and used as a designer drug. Alcoholic beverages are sometimes laced with toxic alcohols, such as methanol and isopropyl alcohol. A mild, brief exposure to isopropyl alcohol is unlikely to cause any serious harm, but many methanol poisoning incidents have occurred through history, since methanol is lethal even in small quantities, as little as 10–15 milliliters. Ethanol is used to treat methanol and ethylene glycol toxicity.
References
- 1 2 Martin, Christopher S.; Earleywine, Mitchell; Musty, Richard E.; Perrine, M. W.; Swift, Robert M. (1 February 1993). "Development and Validation of the Biphasic Alcohol Effects Scale". Alcoholism: Clinical and Experimental Research. 17 (1): 140–146. doi:10.1111/j.1530-0277.1993.tb00739.x. ISSN 1530-0277. PMID 8452195.
- 1 2 3 4 5 6 7 8 9 10 11 12 Roche, Daniel JO; Ray, Lara A (1 May 2015). "Subjective response as a consideration in the pharmacogenetics of alcoholism treatment". Pharmacogenomics. 16 (7): 721–736. doi:10.2217/pgs.14.143. ISSN 1462-2416. PMID 25950242. S2CID 7828383.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 Morean, Meghan E.; Corbin, William R.; Treat, Teresa A. (December 2015). "Evaluating the accuracy of alcohol expectancies relative to subjective response to alcohol". Addictive Behaviors. 51: 197–203. doi:10.1016/j.addbeh.2015.07.027. PMC 4772766 . PMID 26291291.
- 1 2 3 4 5 Quinn, P; Fromme, K (October 2011). "Subjective response to alcohol challenge: a quantitative review". Alcoholism: Clinical and Experimental Research. 35 (10): 1759–70. doi:10.1111/j.1530-0277.2011.01521.x. PMC 3183255 . PMID 21777258.
- 1 2 Pollock, VE (1 November 1992). "Meta-analysis of subjective sensitivity to alcohol in sons of alcoholics". American Journal of Psychiatry. 149 (11): 1534–1538. doi:10.1176/ajp.149.11.1534. ISSN 0002-953X. PMID 1415821.
- ↑ Trim, Ryan S.; Schuckit, Marc A.; Smith, Tom L. (1 September 2009). "The Relationships of the Level of Response to Alcohol and Additional Characteristics to Alcohol Use Disorders Across Adulthood: A Discrete-Time Survival Analysis". Alcoholism: Clinical and Experimental Research. 33 (9): 1562–1570. doi:10.1111/j.1530-0277.2009.00984.x. ISSN 1530-0277. PMC 2947374 . PMID 19485971.
- ↑ "Self-rating of alcohol intoxication by young men with and without family histories of alcoholism". Journal of Studies on Alcohol. 41.
- ↑ O'Malley, S S; Maisto, S A (4 January 2015). "Effects of family drinking history and expectancies on responses to alcohol in men". Journal of Studies on Alcohol. 46 (4): 289–297. doi:10.15288/jsa.1985.46.289. PMID 4033129.
- ↑ Newlin, David B.; Thomson, James B. (1990). "Alcohol challenge with sons of alcoholics: A critical review and analysis". Psychological Bulletin. 108 (3): 383–402. doi:10.1037/0033-2909.108.3.383. PMID 2270234.
- ↑ Morzorati, S. L.; Ramchandani, V. A.; Flury, L.; Li, T.-K.; O'Connor, S. (1 August 2002). "Self-Reported Subjective Perception of Intoxication Reflects Family History of Alcoholism When Breath Alcohol Levels Are Constant". Alcoholism: Clinical and Experimental Research. 26 (8): 1299–1306. doi:10.1111/j.1530-0277.2002.tb02670.x. ISSN 1530-0277. PMID 12198408.
- ↑ King, Andrea C.; Wit, Harriet de; McNamara, Patrick J.; Cao, Dingcai (4 April 2011). "Rewarding, Stimulant, and Sedative Alcohol Responses and Relationship to Future Binge Drinking". Archives of General Psychiatry. 68 (4): 389–99. doi:10.1001/archgenpsychiatry.2011.26. ISSN 0003-990X. PMC 4633413 . PMID 21464363.
- ↑ King, Andrea C.; McNamara, Patrick J.; Hasin, Deborah S.; Cao, Dingcai (15 May 2014). "Alcohol Challenge Responses Predict Future Alcohol Use Disorder Symptoms: A 6-Year Prospective Study". Biological Psychiatry. 75 (10): 798–806. doi:10.1016/j.biopsych.2013.08.001. PMC 4280017 . PMID 24094754.
- ↑ King, Andrea C.; Hasin, Deborah; O'Connor, Sean J.; McNamara, Patrick J.; Cao, Dingcai (15 March 2016). "A Prospective 5-Year Re-examination of Alcohol Response in Heavy Drinkers Progressing in Alcohol Use Disorder". Biological Psychiatry. 79 (6): 489–498. doi:10.1016/j.biopsych.2015.05.007. PMC 4644521 . PMID 26117308.
- ↑ Judd, Lewis L. (1 April 1977). "Lithium Carbonate and Ethanol Induced "Highs" in Normal Subjects". Archives of General Psychiatry. 34 (4): 463–7. doi:10.1001/archpsyc.1977.01770160097008. ISSN 0003-990X. PMID 322635.
- ↑ Schuckit, Marc A. (1 March 1988). "A Simultaneous Evaluation of Multiple Markers of Ethanol/Placebo Challenges in Sons of Alcoholics and Controls". Archives of General Psychiatry. 45 (3): 211–6. doi:10.1001/archpsyc.1988.01800270019002. ISSN 0003-990X. PMID 3422553.
- ↑ Morean, Meghan E.; Corbin, William R.; Treat, Teresa A. (2013). "The Subjective Effects of Alcohol Scale: Development and psychometric evaluation of a novel assessment tool for measuring subjective response to alcohol". Psychological Assessment. 25 (3): 780–795. doi:10.1037/a0032542. PMC 3822039 . PMID 23647036.
- ↑ Arias, Albert; Feinn, Richard; Kranzler, Henry R. (July 2006). "Association of an Asn40Asp (A118G) polymorphism in the μ-opioid receptor gene with substance dependence: A meta-analysis". Drug and Alcohol Dependence. 83 (3): 262–268. doi:10.1016/j.drugalcdep.2005.11.024. PMID 16387451.
- 1 2 3 Jones, Jermaine D.; Comer, Sandra D.; Kranzler, Henry R. (1 March 2015). "The Pharmacogenetics of Alcohol Use Disorder". Alcoholism: Clinical and Experimental Research. 39 (3): 391–402. doi:10.1111/acer.12643. ISSN 1530-0277. PMC 4348335 . PMID 25703505.
- ↑ Koob, George F.; Le Moal, Michel (1 February 2001). "Drug Addiction, Dysregulation of Reward, and Allostasis". Neuropsychopharmacology. 24 (2): 97–129. doi: 10.1016/S0893-133X(00)00195-0 . ISSN 0893-133X. PMID 11120394.
- ↑ C. Garbutt, James (1 June 2010). "Efficacy and Tolerability of Naltrexone in the Management of Alcohol Dependence". Current Pharmaceutical Design. 16 (19): 2091–2097. doi:10.2174/138161210791516459. PMID 20482515.
- ↑ King, Andrea C.; Volpicelli, Joseph R.; Frazer, A.; O'Brien, Charles P. (1997). "Effect of naltrexone on subjective alcohol response in subjects at high and low risk for future alcohol dependence". Psychopharmacology. 129 (1): 15–22. doi:10.1007/s002130050156. ISSN 0033-3158. PMID 9122358. S2CID 25116120.
- ↑ McCaul, Mary E.; Wand, Gary S.; Eissenberg, Thomas; Rohde, Charles A.; Cheskin, Lawrence J. (1 May 2000). "Naltrexone Alters Subjective and Psychomotor Responses to Alcohol in Heavy Drinking Subjects". Neuropsychopharmacology. 22 (5): 480–492. doi: 10.1016/S0893-133X(99)00147-5 . ISSN 0893-133X. PMID 10731623.
- ↑ Ray, Lara A.; Hutchison, Kent E. (1 September 2007). "Effects of Naltrexone on Alcohol Sensitivity and Genetic Moderators of Medication Response". Archives of General Psychiatry. 64 (9): 1069–77. doi: 10.1001/archpsyc.64.9.1069 . ISSN 0003-990X. PMID 17768272.
- ↑ Drobes, David J.; Anton, Raymond F.; Thomas, Suzanne E.; Voronin, Konstantin (1 September 2004). "Effects of Naltrexone and Nalmefene on Subjective Response to Alcohol Among Non-Treatment-Seeking Alcoholics and Social Drinkers". Alcoholism: Clinical and Experimental Research. 28 (9): 1362–1370. doi: 10.1097/01.ALC.0000139704.88862.01 . ISSN 1530-0277. PMID 15365307.