An antiemetic is a drug that is effective against vomiting and nausea. Antiemetics are typically used to treat motion sickness and the side effects of opioid analgesics, general anaesthetics, and chemotherapy directed against cancer. They may be used for severe cases of gastroenteritis, especially if the patient is dehydrated.
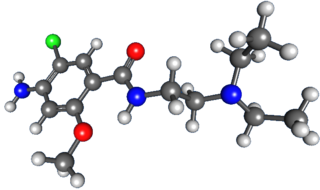
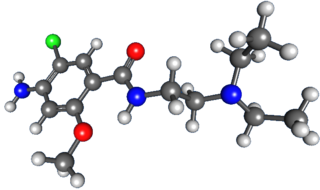
Metoclopramide is a medication used for stomach and esophageal problems. It is commonly used to treat and prevent nausea and vomiting, to help with emptying of the stomach in people with delayed stomach emptying, and to help with gastroesophageal reflux disease. It is also used to treat migraine headaches.

Granisetron is a serotonin 5-HT3 receptor antagonist used as an antiemetic to treat nausea and vomiting following chemotherapy and radiotherapy. Its main effect is to reduce the activity of the vagus nerve, which is a nerve that activates the vomiting center in the medulla oblongata. It does not have much effect on vomiting due to motion sickness. This drug does not have any effect on dopamine receptors or muscarinic receptors.
Postoperative nausea and vomiting (PONV) is the phenomenon of nausea, vomiting, or retching experienced by a patient in the post-anesthesia care unit (PACU) or within 24 hours following a surgical procedure. PONV affects about 10% of the population undergoing general anaesthesia each year. PONV can be unpleasant and lead to a delay in mobilization and food, fluid, and medication intake following surgery.

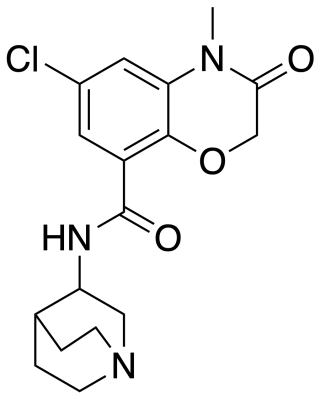
Ondansetron, sold under the brand name Zofran among others, is a medication used to prevent nausea and vomiting caused by cancer chemotherapy, radiation therapy, migraines or surgery. It is also effective for treating gastroenteritis. It can be given orally, intramuscularly, or intravenously.
The chemoreceptor trigger zone (CTZ) is an area of the medulla oblongata that receives inputs from blood-borne drugs or hormones, and communicates with other structures in the vomiting center to initiate vomiting. The CTZ is located within the area postrema, which is on the floor of the fourth ventricle and is outside of the blood–brain barrier. It is also part of the vomiting center itself. The neurotransmitters implicated in the control of nausea and vomiting include acetylcholine, dopamine, histamine, substance P, and serotonin. There are also opioid receptors present, which may be involved in the mechanism by which opiates cause nausea and vomiting. The blood–brain barrier is not as developed here; therefore, drugs such as dopamine which cannot normally enter the CNS may still stimulate the CTZ.

Nabilone, sold under the brand name Cesamet among others, is a synthetic cannabinoid with therapeutic use as an antiemetic and as an adjunct analgesic for neuropathic pain. It mimics tetrahydrocannabinol (THC), the primary psychoactive compound found naturally occurring in Cannabis.

Dolasetron (trade name Anzemet) is a serotonin 5-HT3 receptor antagonist used to treat nausea and vomiting following chemotherapy. Its main effect is to reduce the activity of the vagus nerve, which is a nerve that activates the vomiting center in the medulla oblongata. It does not have much antiemetic effect when symptoms are due to motion sickness. This drug does not have any effect on dopamine receptors or muscarinic receptors.
ABVD is a chemotherapy regimen used in the first-line treatment of Hodgkin lymphoma, replacing the older MOPP protocol. It consists of concurrent treatment with the chemotherapy drugs:

Vomiting is the involuntary, forceful expulsion of the contents of one's stomach through the mouth and sometimes the nose.
Neurokinin 1 (NK1) antagonists (-pitants) are a novel class of medications that possesses unique antidepressant, anxiolytic, and antiemetic properties. NK-1 antagonists boost the efficacy of 5-HT3 antagonists to prevent nausea and vomiting. The discovery of neurokinin 1 (NK1) receptor antagonists was a turning point in the prevention of nausea and vomiting associated with cancer chemotherapy.
Radiation enteropathy is a syndrome that may develop following abdominal or pelvic radiation therapy for cancer. Many affected people are cancer survivors who had treatment for cervical cancer or prostate cancer; it has also been termed pelvic radiation disease with radiation proctitis being one of the principal features.

The 5-HT3 antagonists, informally known as "setrons", are a class of drugs that act as receptor antagonists at the 5-HT3 receptor, a subtype of serotonin receptor found in terminals of the vagus nerve and in certain areas of the brain. With the notable exceptions of alosetron and cilansetron, which are used in the treatment of irritable bowel syndrome, all 5-HT3 antagonists are antiemetics, used in the prevention and treatment of nausea and vomiting. They are particularly effective in controlling the nausea and vomiting produced by cancer chemotherapy and are considered the gold standard for this purpose.
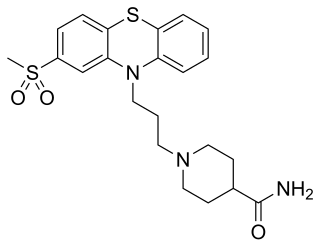
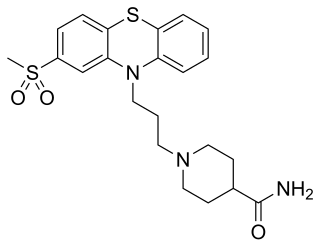
Metopimazine, sold under the brand names Vogalen and Vogalene, is an antiemetic of the phenothiazine group which is used to treat nausea and vomiting. It is marketed in Europe, Canada, and South America. As of August 2020, metopimazine has been repurposed and is additionally under development for use in the United States for the treatment of gastroparesis.
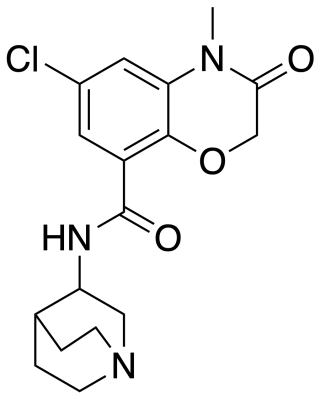
Azasetron is an antiemetic which acts as a 5-HT3 receptor antagonist, pKi = 9.27 It is used in the management of nausea and vomiting induced by cancer chemotherapy (such as cisplatin chemotherapy). Azasetron hydrochloride is given in a usual dose of 10 mg once daily by mouth or intravenously. It is approved for marketing in Japan, and marketed exclusively by Torii Pharmaceutical Co., Ltd. under the trade names "Serotone I.V. Injection 10 mg" and "Serotone Tablets 10 mg". Pharmacokinetics data from S. Tsukagoshi.

Nausea is a diffuse sensation of unease and discomfort, sometimes perceived as an urge to vomit. While not painful, it can be a debilitating symptom if prolonged and has been described as placing discomfort on the chest, abdomen, or back of the throat.

Dazopride (AHR-5531) is an antiemetic and gastroprokinetic agent of the benzamide class which was never marketed. It acts as a 5-HT3 receptor antagonist and 5-HT4 receptor agonist. In addition to its gastrointestinal effects, dazopride facilitates learning and memory in mice.
Chemotherapy-induced nausea and vomiting (CINV) is a common side-effect of many cancer treatments. Nausea and vomiting are two of the most feared cancer treatment-related side effects for cancer patients and their families. In 1983, Coates et al. found that patients receiving chemotherapy ranked nausea and vomiting as the first and second most severe side effects, respectively. Up to 20% of patients receiving highly emetogenic agents in this era postponed, or even refused, potentially curative treatments. Since the 1990s, several novel classes of antiemetics have been developed and commercialized, becoming a nearly universal standard in chemotherapy regimens, and helping to better manage these symptoms in a large portion of patients. Efficient mediation of these unpleasant and sometimes debilitating symptoms results in increased quality of life for the patient, and better overall health of the patient, and, due to better patient tolerance, more effective treatment cycles.

Rolapitant (INN, trade name Varubivə-ROO-bee in the US and Varuby in the European Union) is a drug originally developed by Schering-Plough and licensed for clinical development by Tesaro, which acts as a selective NK1 receptor antagonist (antagonist for the NK1 receptor). It has been approved as a medication for the treatment of chemotherapy-induced nausea and vomiting (CINV) after clinical trials showed it to have similar or improved efficacy and some improvement in safety over existing drugs for this application.
Paul L. R. Andrews is a British physiologist whose basic research on the mechanisms of action and efficacy of antiemetic substances contributed to development of treatments for anti-cancer chemotherapy-induced nausea and vomiting.