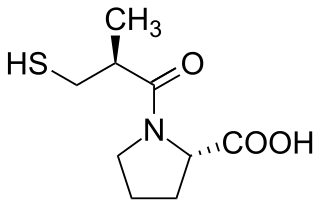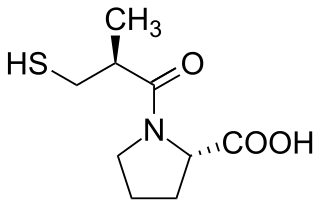
Angiotensin-converting-enzyme inhibitors are a class of medication used primarily for the treatment of high blood pressure and heart failure. This class of medicine works by causing relaxation of blood vessels as well as a decrease in blood volume, which leads to lower blood pressure and decreased oxygen demand from the heart.
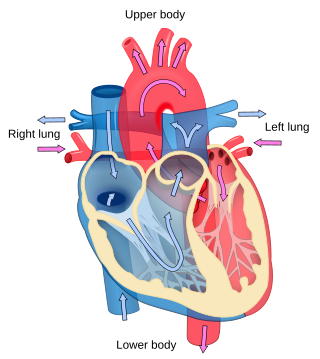
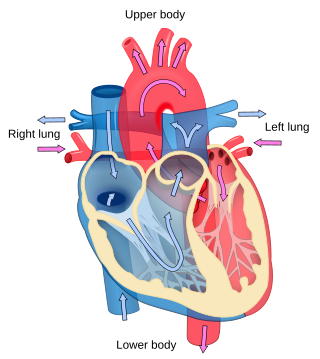
Cardiology is the study of the heart. Cardiology is a branch of medicine that deals with disorders of the heart and the cardiovascular system. The field includes medical diagnosis and treatment of congenital heart defects, coronary artery disease, heart failure, valvular heart disease, and electrophysiology. Physicians who specialize in this field of medicine are called cardiologists, a specialty of internal medicine. Pediatric cardiologists are pediatricians who specialize in cardiology. Physicians who specialize in cardiac surgery are called cardiothoracic surgeons or cardiac surgeons, a specialty of general surgery.

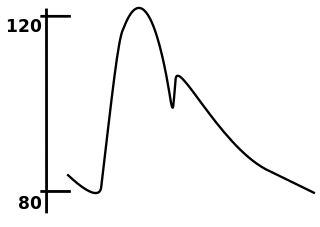
Blood pressure (BP) is the pressure of circulating blood against the walls of blood vessels. Most of this pressure results from the heart pumping blood through the circulatory system. When used without qualification, the term "blood pressure" refers to the pressure in a brachial artery, where it is most commonly measured. Blood pressure is usually expressed in terms of the systolic pressure over diastolic pressure in the cardiac cycle. It is measured in millimeters of mercury (mmHg) above the surrounding atmospheric pressure, or in kilopascals (kPa). The difference between the systolic and diastolic pressures is known as pulse pressure, while the average pressure during a cardiac cycle is known as mean arterial pressure.

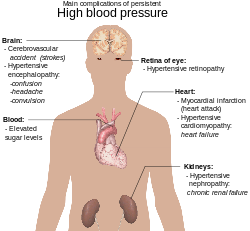
Hypertension, also known as high blood pressure, is a long-term medical condition in which the blood pressure in the arteries is persistently elevated. High blood pressure usually does not cause symptoms. It is, however, a major risk factor for stroke, coronary artery disease, heart failure, atrial fibrillation, peripheral arterial disease, vision loss, chronic kidney disease, and dementia. Hypertension is a major cause of premature death worldwide.

Microangiopathy is a disease of the microvessels, small blood vessels in the microcirculation. It can be contrasted to macroangiopathies such as atherosclerosis, where large and medium-sized arteries are primarily affected.

Pulse pressure is the difference between systolic and diastolic blood pressure. It is measured in millimeters of mercury (mmHg). It represents the force that the heart generates each time it contracts. Healthy pulse pressure is around 40 mmHg. A pulse pressure that is consistently 60 mmHg or greater is likely to be associated with disease, and a pulse pressure of 50 mmHg or more increases the risk of cardiovascular disease. Pulse pressure is considered low if it is less than 25% of the systolic. A very low pulse pressure can be a symptom of disorders such as congestive heart failure.
Antihypertensives are a class of drugs that are used to treat hypertension. Antihypertensive therapy seeks to prevent the complications of high blood pressure, such as stroke, heart failure, kidney failure and myocardial infarction. Evidence suggests that reduction of the blood pressure by 5 mmHg can decrease the risk of stroke by 34% and of ischaemic heart disease by 21%, and can reduce the likelihood of dementia, heart failure, and mortality from cardiovascular disease. There are many classes of antihypertensives, which lower blood pressure by different means. Among the most important and most widely used medications are thiazide diuretics, calcium channel blockers, ACE inhibitors, angiotensin II receptor antagonists (ARBs), and beta blockers.
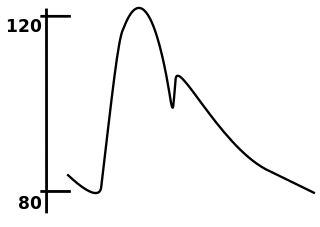
In medicine, the mean arterial pressure (MAP) is an average calculated blood pressure in an individual during a single cardiac cycle. Although methods of estimating MAP vary, a common calculation is to take one-third of the pulse pressure, and add that amount to the diastolic pressure. A normal MAP is about 90 mmHg.

A hypertensive emergency is very high blood pressure with potentially life-threatening symptoms and signs of acute damage to one or more organ systems. It is different from a hypertensive urgency by this additional evidence for impending irreversible hypertension-mediated organ damage (HMOD). Blood pressure is often above 200/120 mmHg, however there are no universally accepted cutoff values.

Hypertensive heart disease includes a number of complications of high blood pressure that affect the heart. While there are several definitions of hypertensive heart disease in the medical literature, the term is most widely used in the context of the International Classification of Diseases (ICD) coding categories. The definition includes heart failure and other cardiac complications of hypertension when a causal relationship between the heart disease and hypertension is stated or implied on the death certificate. In 2013 hypertensive heart disease resulted in 1.07 million deaths as compared with 630,000 deaths in 1990.

Perindopril is a medication used to treat high blood pressure, heart failure, or stable coronary artery disease.
The DASH diet is a dietary pattern promoted by the U.S.-based National Heart, Lung, and Blood Institute to prevent and control hypertension. The DASH diet is rich in fruits, vegetables, whole grains, and low-fat dairy foods. It includes meat, fish, poultry, nuts, and beans, and is limited in sugar-sweetened foods and beverages, red meat, and added fats. In addition to its effect on blood pressure, it is designed to be a well-balanced approach to eating for the general public. DASH is recommended by the United States Department of Agriculture (USDA) as a healthy eating plan. The DASH diet is one of three healthy diets recommended in the 2015–2020 US Dietary Guidelines, which also include the Mediterranean diet and a vegetarian diet. The American Heart Association (AHA) considers the DASH diet "specific and well-documented across age, sex and ethnically diverse groups."
Spontaneously hypertensive rat (SHR) is a laboratory rat which is an animal model of primary hypertension, used to study cardiovascular disease. It is the most studied model of hypertension measured as number of publications. The SHR strain was obtained during the 1960s by Okamoto and colleagues, who started breeding Wistar-Kyoto rats with high blood pressure.
Arterial stiffness occurs as a consequence of biological aging and arteriosclerosis. Inflammation plays a major role in arteriosclerosis development, and consequently it is a major contributor in large arteries stiffening. Increased arterial stiffness is associated with an increased risk of cardiovascular events such as myocardial infarction, hypertension, heart failure and stroke, the two leading causes of death in the developed world. The World Health Organization predicts that in 2010, cardiovascular disease will also be the leading killer in the developing world and represents a major global health problem.
In medicine, systolic hypertension is defined as an elevated systolic blood pressure (SBP). If the systolic blood pressure is elevated (>140) with a normal (<90) diastolic blood pressure (DBP), it is called isolated systolic hypertension. Eighty percent of people with systolic hypertension are over the age of 65 years old.

Diabetic cardiomyopathy is a disorder of the heart muscle in people with diabetes. It can lead to inability of the heart to circulate blood through the body effectively, a state known as heart failure(HF), with accumulation of fluid in the lungs or legs. Most heart failure in people with diabetes results from coronary artery disease, and diabetic cardiomyopathy is only said to exist if there is no coronary artery disease to explain the heart muscle disorder.

Pathophysiology is a study which explains the function of the body as it relates to diseases and conditions. The pathophysiology of hypertension is an area which attempts to explain mechanistically the causes of hypertension, which is a chronic disease characterized by elevation of blood pressure. Hypertension can be classified by cause as either essential or secondary. About 90–95% of hypertension is essential hypertension. Some authorities define essential hypertension as that which has no known explanation, while others define its cause as being due to overconsumption of sodium and underconsumption of potassium. Secondary hypertension indicates that the hypertension is a result of a specific underlying condition with a well-known mechanism, such as chronic kidney disease, narrowing of the aorta or kidney arteries, or endocrine disorders such as excess aldosterone, cortisol, or catecholamines. Persistent hypertension is a major risk factor for hypertensive heart disease, coronary artery disease, stroke, aortic aneurysm, peripheral artery disease, and chronic kidney disease.
Orthostatic hypertension is a medical condition consisting of a sudden and abrupt increase in blood pressure (BP) when a person stands up. Orthostatic hypertension is diagnosed by a rise in systolic BP of 20 mmHg or more when standing. Orthostatic diastolic hypertension is a condition in which the diastolic BP raises to 98 mmHg or over in response to standing, but this definition currently lacks clear medical consensus, so is subject to change. Orthostatic hypertension involving the systolic BP is known as systolic orthostatic hypertension.

Heart failure with preserved ejection fraction (HFpEF) is a form of heart failure in which the ejection fraction – the percentage of the volume of blood ejected from the left ventricle with each heartbeat divided by the volume of blood when the left ventricle is maximally filled – is normal, defined as greater than 50%; this may be measured by echocardiography or cardiac catheterization. Approximately half of people with heart failure have preserved ejection fraction, while the other half have a reduction in ejection fraction, called heart failure with reduced ejection fraction (HFrEF).

Hypertension is a condition characterized by an elevated blood pressure in which the long term consequences include cardiovascular disease, kidney disease, adrenal gland tumors, vision impairment, memory loss, metabolic syndrome, stroke and dementia. It affects nearly 1 in 2 Americans and remains as a contributing cause of death in the United States. There are many genetic and environmental factors involved with the development of hypertension including genetics, diet, and stress.