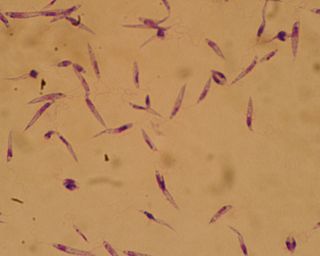
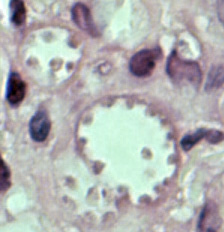
Leishmania is a parasitic protozoan, a single-celled organism of the genus Leishmania that is responsible for the disease leishmaniasis. They are spread by sandflies of the genus Phlebotomus in the Old World, and of the genus Lutzomyia in the New World. At least 93 sandfly species are proven or probable vectors worldwide. Their primary hosts are vertebrates; Leishmania commonly infects hyraxes, canids, rodents, and humans.

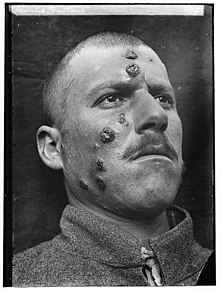
Leishmaniasis is a wide array of clinical manifestations caused by parasites of the Trypanosomatida genus Leishmania. It is generally spread through the bite of phlebotomine sandflies, Phlebotomus and Lutzomyia, and occurs most frequently in the tropics and sub-tropics of Africa, Asia, the Americas, and southern Europe. The disease can present in three main ways: cutaneous, mucocutaneous, or visceral. The cutaneous form presents with skin ulcers, while the mucocutaneous form presents with ulcers of the skin, mouth, and nose. The visceral form starts with skin ulcers and later presents with fever, low red blood cell count, and enlarged spleen and liver.

Sandfly or sand fly is a colloquial name for any species or genus of flying, biting, blood-sucking dipteran (fly) encountered in sandy areas. In the United States, sandfly may refer to certain horse flies that are also known as "greenheads", or to members of the family Ceratopogonidae. The bites usually result in a small, intensely itchy bump or welt, the strength of which intensifies over a period of 5-7 days before dissipating. Moderate relief is achieved with varying success through the application of over the counter products such as Benadryl (ingested) or an analgesic cream such as After Bite. Outside the United States, sandfly may refer to members of the subfamily Phlebotominae within the Psychodidae. Biting midges (Ceratopogonidae) are sometimes called sandflies or no-see-ums. New Zealand sandflies are in the genus of sand fly Austrosimulium, a type of black fly.

Lutzomyia is a genus of phlebotomine sand flies consisting of nearly 400 species, at least 33 of which have medical importance as vectors of human disease. Species of the genus Lutzomyia are found only in the New World, distributed in southern areas of the Nearctic and throughout the Neotropical realm. Lutzomyia is one of the two genera of the subfamily Phlebotominae to transmit the Leishmania parasite, with the other being Phlebotomus, found only in the Old World. Lutzomyia sand flies also serve as vectors for the bacterial Carrion's disease and a number of arboviruses.

Phlebotomus is a genus of "sand flies" in the Diptera family Psychodidae. In the past, they have sometimes been considered to belong in a separate family, Phlebotomidae, but this alternative classification has not gained wide acceptance.

Visceral leishmaniasis (VL), also known as kala-azar or "black fever", is the most severe form of leishmaniasis and, without proper diagnosis and treatment, is associated with high fatality. Leishmaniasis is a disease caused by protozoan parasites of the genus Leishmania.

Miltefosine, sold under the trade name Impavido among others, is a medication mainly used to treat leishmaniasis and free-living amoeba infections such as Naegleria fowleri and Balamuthia mandrillaris. This includes the three forms of leishmaniasis: cutaneous, visceral and mucosal. It may be used with liposomal amphotericin B or paromomycin. It is taken by mouth.
A canine vector-borne disease (CVBD) is one of "a group of globally distributed and rapidly spreading illnesses that are caused by a range of pathogens transmitted by arthropods including ticks, fleas, mosquitoes and phlebotomine sandflies." CVBDs are important in the fields of veterinary medicine, animal welfare, and public health. Some CVBDs are of zoonotic concern.

Leishmania infantum is the causative agent of infantile visceral leishmaniasis in the Mediterranean region and in Latin America, where it has been called Leishmania chagasi. It is also an unusual cause of cutaneous leishmaniasis, which is normally caused by specific lineages. Wild canids and domestic dogs are the natural reservoir of this organism. The sandfly species Lutzomyia longipalpis serves as the primary vector for the transmission of the disease.
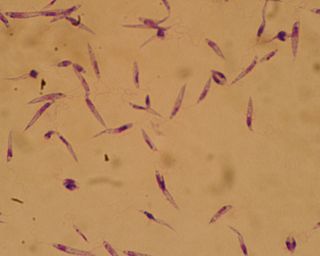
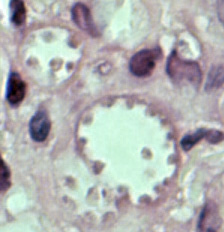
Leishmania major is a species of parasite found in the genus Leishmania, and is associated with the disease zoonotic cutaneous leishmaniasis. L. major is an intracellular pathogen which infects the macrophages and dendritic cells of the immune system. Though Leishmania species are found on every continent aside from Antarctica, Leishmania major is found only in the Eastern Hemisphere, specifically in Northern Africa, the Middle East, Northwestern China, and Northwestern India.

Canine leishmaniasis (LEESH-ma-NIGH-ah-sis) is a zoonotic disease caused by Leishmania parasites transmitted by the bite of an infected phlebotomine sandfly. Canine leishmaniasis was first identified in Europe in 1903, and in 1940, 40% of all dogs in Rome were determined to be positive for leishmaniasis. Traditionally thought of as a disease only found near the Mediterranean basin, 2008 research claims new findings are evidence that canine leishmaniasis is currently expanding in continental climate areas of northwestern Italy, far from the recognized disease-endemic areas along the Mediterranean coasts. Cases of leishmaniasis began appearing in North America in 2000, and, as of 2008, Leishmania-positive foxhounds have been reported in 22 U.S. states and two Canadian provinces.

Leishmania donovani is a species of intracellular parasites belonging to the genus Leishmania, a group of haemoflagellate kinetoplastids that cause the disease leishmaniasis. It is a human blood parasite responsible for visceral leishmaniasis or kala-azar, the most severe form of leishmaniasis. It infects the mononuclear phagocyte system including spleen, liver and bone marrow. Infection is transmitted by species of sandfly belonging to the genus Phlebotomus in Old World and Lutzomyia in New World. The species complex it represents is prevalent throughout tropical and temperate regions including Africa, China, India, Nepal, southern Europe, Russia and South America. The species complex is responsible for thousands of deaths every year and has spread to 88 countries, with 350 million people at constant risk of infection and 0.5 million new cases in a year.

Leishmania tropica is a flagellate parasite and the cause of anthroponotic cutaneous leishmaniasis in humans. This parasite is restricted to Afro-Eurasia and is a common cause of infection in Afghanistan, Iran, Syria, Yemen, Algeria, Morocco, and northern India.
Leishmania braziliensis is a Leishmania species.
Leishmania mexicana is a species of obligate intracellular parasites of the protozoan genus Leishmania. In Mexico and Central America, this parasite is the primary cause of cutaneous leishmaniasis.

Post-kala-azar dermal leishmaniasis (PKDL) is a complication of visceral leishmaniasis (VL); it is characterised by a macular, maculopapular, and nodular rash in a patient who has recovered from VL and who is otherwise well. The rash usually starts around the mouth from where it spreads to other parts of the body depending on severity.
Leishmania amazonensis is a parasite responsible for the disease leishmaniasis. This species has been known to spread by using sandflies as its vector and a vertebrate as its primary host, just like other species of Leishmania. They have also been known to spread throughout the Brazilian Amazon region due to their ecological niches needed for survival and reproduction. However, when the host is infected, the Leishmania can cause 3 different forms of Leishmaniasis. For this species, it has been known to cause cutaneous leishmaniasis and mucocutaneous leishmaniasis. Cutaneous leishmaniasis is commonly characterized with skin lesions, which can appear localized, or throughout the body. While mucocutaneous leishmaniasis is characterized with ulcers around the skin, mouth, and nose. This form of Leishmaniasis has also been known to can spread by metastasis and can be deadly.

Lutzomyia longipalpis is a species complex of sandfly belonging to the family Psychodidae. This species is primarily present in Central and South America, but has also appeared in Mexico. There have been reports of L. longipalpis as far south as Argentina, as they are found in a wide variety of ecological conditions. Both males and females feed on sugars from plants and aphids, but only adult females feed on the blood of other mammals. The species has recently begun appearing in urban areas throughout Brazil, and serves as a key vessel for the propagation of the parasite Leishmania infantum. The presence of these flies appears to be strongly correlated to the presence of domestic chickens in Latin America. The first major urban outbreak of the lethal Visceral leishmanias epidemic was detected in Teresina, Piauí State in the early 1980s following a massive planting of acacias.
Kala azar in India refers to the special circumstances of the disease kala azar as it exists in India. Kala azar is a major health problem in India with an estimated 146,700 new cases per year as of 2012. In the disease a parasite causes sickness after migrating to internal organs such as the liver, spleen and bone marrow. If left untreated the disease almost always results in the death. Signs and symptoms include fever, weight loss, fatigue, anemia, and substantial swelling of the liver and spleen.

A Leishmaniasis vaccine is a vaccine which would prevent leishmaniasis. As of 2017, no vaccine for humans was available. Currently some effective leishmaniasis vaccines for dogs exist.