Related Research Articles

Giardia is a genus of anaerobic flagellated protozoan parasites of the phylum Metamonada that colonise and reproduce in the small intestines of several vertebrates, causing the disease giardiasis. Their life cycle alternates between a swimming trophozoite and an infective, resistant cyst. Giardia were first described by the Dutch microscopist Antonie van Leeuwenhoek in 1681. The genus is named after French zoologist Alfred Mathieu Giard.

Giardia duodenalis, also known as Giardia intestinalis and Giardia lamblia, is a flagellated parasitic protozoan microorganism of the genus Giardia that colonizes the small intestine, causing a diarrheal condition known as giardiasis. The parasite attaches to the intestinal epithelium by an adhesive disc or sucker, and reproduces via binary fission. Giardiasis does not spread to other parts of the gastrointestinal tract, but remains confined to the lumen of the small intestine. The microorganism has an outer membrane that makes it possible to survive even when outside of its host, and which can render it tolerant to certain disinfectants. Giardia trophozoites are anaerobic, and absorb their nutrients from the intestinal lumen. If the organism is stained, its characteristic pattern resembles the familiar "smiley face" symbol.

Cryptosporidiosis, sometimes informally called crypto, is a parasitic disease caused by Cryptosporidium, a genus of protozoan parasites in the phylum Apicomplexa. It affects the distal small intestine and can affect the respiratory tract in both immunocompetent and immunocompromised individuals, resulting in watery diarrhea with or without an unexplained cough. In immunosuppressed individuals, the symptoms are particularly severe and can be fatal. It is primarily spread through the fecal-oral route, often through contaminated water; recent evidence suggests that it can also be transmitted via fomites contaminated with respiratory secretions.

Babesiosis or piroplasmosis is a malaria-like parasitic disease caused by infection with a eukaryotic parasite in the order Piroplasmida, typically a Babesia or Theileria, in the phylum Apicomplexa. Human babesiosis transmission via tick bite is most common in the Northeastern and Midwestern United States and parts of Europe, and sporadic throughout the rest of the world. It occurs in warm weather. People can get infected with Babesia parasites by the bite of an infected tick, by getting a blood transfusion from an infected donor of blood products, or by congenital transmission . Ticks transmit the human strain of babesiosis, so it often presents with other tick-borne illnesses such as Lyme disease. After trypanosomes, Babesia is thought to be the second-most common blood parasite of mammals. They can have major adverse effects on the health of domestic animals in areas without severe winters. In cattle, the disease is known as Texas cattle fever or redwater.

Giardiasis is a parasitic disease caused by Giardia duodenalis. Infected individuals who experience symptoms may have diarrhoea, abdominal pain, and weight loss. Less common symptoms include vomiting and blood in the stool. Symptoms usually begin one to three weeks after exposure and, without treatment, may last two to six weeks or longer.
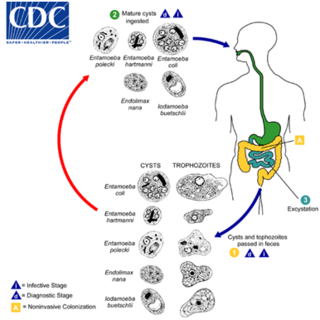
Entamoeba coli is a non-pathogenic species of Entamoeba that frequently exists as a commensal parasite in the human gastrointestinal tract. E. coli is important in medicine because it can be confused during microscopic examination of stained stool specimens with the pathogenic Entamoeba histolytica. This amoeba does not move much by the use of its pseudopod, and creates a "sur place (non-progressive) movement" inside the large intestine. Usually, the amoeba is immobile, and keeps its round shape. This amoeba, in its trophozoite stage, is only visible in fresh, unfixed stool specimens. Sometimes the Entamoeba coli have parasites as well. One is the fungus Sphaerita spp. This fungus lives in the cytoplasm of the E. coli. While this differentiation is typically done by visual examination of the parasitic cysts via light microscopy, new methods using molecular biology techniques have been developed. The scientific name of the amoeba, E. coli, is often mistaken for the bacterium, Escherichia coli. Unlike the bacterium, the amoeba is mostly harmless, and does not cause as many intestinal problems as some strains of the E. coli bacterium. To make the naming of these organisms less confusing, "alternate contractions" are used to name the species for the purpose making the naming easier; for example, using Esch. coli and Ent. coli for the bacterium and amoeba, instead of using E. coli for both.

Strongyloidiasis is a human parasitic disease caused by the nematode called Strongyloides stercoralis, or sometimes the closely related S. fülleborni. These helminths belong to a group of nematodes called roundworms. These intestinal worms can cause a number of symptoms in people, principally skin symptoms, abdominal pain, diarrhea and weight loss, but also many other specific and vague symptoms in disseminated disease, and severe life-threatening conditions through hyperinfection. In some people, particularly those who require corticosteroids or other immunosuppressive medication, Strongyloides can cause a hyperinfection syndrome that can lead to death if untreated. The diagnosis is made by blood and stool tests. The medication ivermectin is widely used to treat strongyloidiasis.

Echinococcus granulosus, also called the hydatid worm or dog tapeworm, is a cyclophyllid cestode that dwells in the small intestine of canids as an adult, but which has important intermediate hosts such as livestock and humans, where it causes cystic echinococcosis, also known as hydatid disease. The adult tapeworm ranges in length from 3 mm to 6 mm and has three proglottids ("segments") when intact—an immature proglottid, mature proglottid and a gravid proglottid. The average number of eggs per gravid proglottid is 823. Like all cyclophyllideans, E. granulosus has four suckers on its scolex ("head"), and E. granulosus also has a rostellum with hooks. Several strains of E. granulosus have been identified, and all but two are noted to be infective in humans.

Taeniasis is an infection within the intestines by adult tapeworms belonging to the genus Taenia. There are generally no or only mild symptoms. Symptoms may occasionally include weight loss or abdominal pain. Segments of tapeworm may be seen in the stool. Complications of pork tapeworm may include cysticercosis.
Bartonellosis is an infectious disease produced by bacteria of the genus Bartonella. Bartonella species cause diseases such as Carrión's disease, trench fever, cat-scratch disease, bacillary angiomatosis, peliosis hepatis, chronic bacteremia, endocarditis, chronic lymphadenopathy, and neurological disorders.

Balantidiasis is a protozoan infection caused by infection with Balantidium coli.

A subclinical infection—sometimes called a preinfection or inapparent infection—is an infection by a pathogen that causes few or no signs or symptoms of infection in the host. Subclinical infections can occur in both humans and animals. Depending on the pathogen, which can be a virus or intestinal parasite, the host may be infectious and able to transmit the pathogen without ever developing symptoms; such a host is called an asymptomatic carrier. Many pathogens, including HIV, typhoid fever, and coronaviruses such as COVID-19 spread in their host populations through subclinical infection.

Blastocystis is a genus of single-celled parasites belonging to the Stramenopiles that includes algae, diatoms, and water molds. There are several species, living in the gastrointestinal tracts of species as diverse as humans, farm animals, birds, rodents, reptiles, amphibians, fish, and cockroaches. Blastocystis has low host specificity, and many different species of Blastocystis can infect humans, and by current convention, any of these species would be identified as Blastocystis hominis.
The discovery of disease-causing pathogens is an important activity in the field of medical science. Many viruses, bacteria, protozoa, fungi, helminthes and prions are identified as a confirmed or potential pathogen. In the United States, a Centers for Disease Control program, begun in 1995, identified over a hundred patients with life-threatening illnesses that were considered to be of an infectious cause, but that could not be linked to a known pathogen. The association of pathogens with disease can be a complex and controversial process, in some cases requiring decades or even centuries to achieve.

Blastocystosis refers to a medical condition caused by infection with Blastocystis. Blastocystis is a protozoal, single-celled parasite that inhabits the gastrointestinal tracts of humans and other animals. Many different types of Blastocystis exist, and they can infect humans, farm animals, birds, rodents, amphibians, reptiles, fish, and even cockroaches. Blastocystosis has been found to be a possible risk factor for development of irritable bowel syndrome.

Protozoan infections are parasitic diseases caused by organisms formerly classified in the kingdom Protozoa. These organisms are now classified in the supergroups Excavata, Amoebozoa, Harosa, and Archaeplastida. They are usually contracted by either an insect vector or by contact with an infected substance or surface.

Amoebiasis, or amoebic dysentery, is an infection of the intestines caused by a parasitic amoeba Entamoeba histolytica. Amoebiasis can be present with no, mild, or severe symptoms. Symptoms may include lethargy, loss of weight, colonic ulcerations, abdominal pain, diarrhea, or bloody diarrhea. Complications can include inflammation and ulceration of the colon with tissue death or perforation, which may result in peritonitis. Anemia may develop due to prolonged gastric bleeding.
Entamoeba polecki is an intestinal parasite of the genus Entamoeba. E. polecki is found primarily in pigs and monkeys and is largely considered non-pathogenic in humans, although there have been some reports regarding symptomatic infections of humans. Prevalence is concentrated in New Guinea, with distribution also recorded in areas of southeast Asia, France, and the United States.
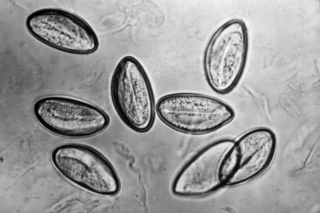
Pinworm infection, also known as enterobiasis, is a human parasitic disease caused by the pinworm, Enterobius vermicularis. The most common symptom is itching in the anal area. The period of time from swallowing eggs to the appearance of new eggs around the anus is 4 to 8 weeks. Some people who are infected do not have symptoms.

Dientamoeba fragilis is a species of single-celled excavates found in the gastrointestinal tract of some humans, pigs and gorillas. It causes gastrointestinal upset in some people, but not in others. It is an important cause of travellers diarrhoea, chronic diarrhoea, fatigue and, in children, failure to thrive. Despite this, its role as a "commensal, pathobiont, or pathogen" is still debated. D. fragilis is one of the smaller parasites that are able to live in the human intestine. Dientamoeba fragilis cells are able to survive and move in fresh feces but are sensitive to aerobic environments. They dissociate when in contact or placed in saline, tap water or distilled water.
References
- ↑ Vandenberg O, Peek R, Souayah H, et al. (2006). "Clinical and microbiological features of dientamoebiasis in patients suspected of suffering from a parasitic gastrointestinal illness: a comparison of Dientamoeba fragilis and Giardia lamblia infections". Int. J. Infect. Dis. 10 (3): 255–61. doi: 10.1016/j.ijid.2005.05.011 . PMID 16469517.
- 1 2 Norberg A, Nord CE, Evengård B (2003). "Dientamoeba fragilis—a protozoal infection that may cause severe bowel distress". Clin. Microbiol. Infect. 9 (1): 65–8. doi: 10.1046/j.1469-0691.2003.00459.x . PMID 12691546.
- 1 2 3 4 5 Johnson EH, Windsor JJ, Clark CG (2004). "Emerging from obscurity: biological, clinical, and diagnostic aspects of Dientamoeba fragilis". Clin. Microbiol. Rev. 17 (3): 553–70, table of contents. doi:10.1128/CMR.17.3.553-570.2004. PMC 452553 . PMID 15258093.
- ↑ Stark D, Beebe N, Marriott D, Ellis J, Harkness J (2005). "Prospective study of the prevalence, genotyping, and clinical relevance of Dientamoeba fragilis infections in an Australian population" (PDF). J. Clin. Microbiol. 43 (6): 2718–23. doi:10.1128/JCM.43.6.2718-2723.2005. PMC 1151954 . PMID 15956388.
- ↑ Johnson JA, Clark CG (2000). "Cryptic genetic diversity in Dientamoeba fragilis". J. Clin. Microbiol. 38 (12): 4653–4654. doi:10.1128/JCM.38.12.4653-4654.2000. PMC 87656 . PMID 11101615.
- 1 2 3 Lagacé-Wiens PR, VanCaeseele PG, Koschik C (2006). "Dientamoeba fragilis: an emerging role in intestinal disease". Canadian Medical Association Journal. 175 (5): 468–9. doi:10.1503/cmaj.060265. PMC 1550747 . PMID 16940260.
- ↑ Ogren J, Dienus O, Löfgren S, Iveroth P, Matussek A (2013). "Dientamoeba fragilis DNA detection in Enterobius vermicularis eggs". Pathogens and Disease. 69 (2): 157–8. doi:10.1111/2049-632X.12071. PMC 3908373 . PMID 23893951.
- ↑ Bottone, Edward J. (17 January 2006). Atlas of the Clinical Microbiology of Infectious Diseases: Viral, Fungal and Parasitic Agents. CRC Press. ISBN 9781842142400 – via Google Books.
- ↑ Grendon JH, Digiacomo RF, Frost FJ (1991). "Dientamoeba fragilis detection methods and prevalence: a survey of state public health laboratories". Public Health Rep. 106 (3): 322–5. PMC 1580247 . PMID 1905055.
- ↑ Steinitz H, Talis B, Stein B (1970). "Entamoeba histolytica and Dientamoeba fragilis and the syndrome of chronic recurrent intestinal amoebiasis in Israel". Digestion. 3 (3): 146–53. doi:10.1159/000197025. PMID 4317789.
- ↑ Windsor JJ, Macfarlane L, Hughes-Thapa G, Jones SK, Whiteside TM (2003). "Detection of Dientamoeba fragilis by culture". Br. J. Biomed. Sci. 60 (2): 79–83. doi:10.1080/09674845.2003.11783678. PMID 12866914. S2CID 3530597.
- ↑ Sawangjaroen N, Luke R, Prociv P (1993). "Diagnosis by faecal culture of Dientamoeba fragilis infections in Australian patients with diarrhoea". Trans. R. Soc. Trop. Med. Hyg. 87 (2): 163–5. doi:10.1016/0035-9203(93)90472-3. PMID 8337717.
- ↑ Borody T, Warren E, Wettstein A, et al. (2002). "Eradication of Dientamoeba fragilis can resolve IBS-like symptoms". J Gastroenterol Hepatol. 17 (Suppl): A103. doi:10.1046/j.1440-1746.2002.02681.x. PMID 11895561. S2CID 37118600.